ACL Surgery: Understanding The Procedure And Your Available Options

Medically Reviewed By:

Anterior cruciate ligament (ACL) surgery is used to repair a torn ACL, a common problem that accounts for almost half of all knee injuries. This injury often results from sports accidents, direct trauma, or age-related wear and tear of the ligament.
While ACL surgery is a common treatment option, it carries certain risks, including infection, long-term pain, and potential damage to other knee components. Additionally, a recent study suggests that the ACL may have some capacity to heal naturally. These findings highlight how invasive interventions are sometimes unnecessary.
It is crucial for patients to explore less invasive alternatives that offer a path to recovery without prescription medications or surgery. Procedures using Regenexx injectates utilize interventional orthobiologics to support the body’s natural healing process, offering an alternative to surgery.
Understanding ACL Injuries
The ACL sits in the center of the knee, connecting the thigh bone to the shin bone. It stabilizes the knee during standing, walking, running, and jumping.
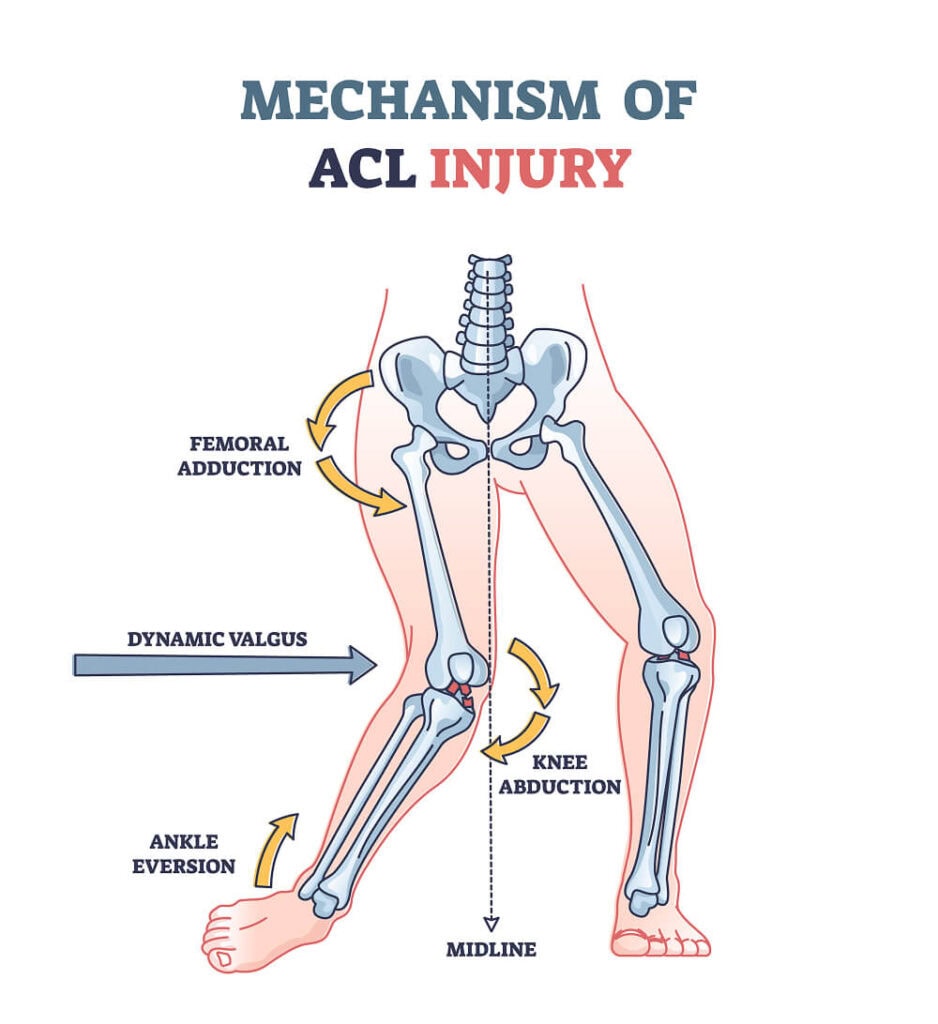
Tears often result from sudden stops, jumps, or sudden changes in direction, which are common in sports like soccer and basketball. Aging adults are also at risk because the progressive wear and tear of the knee joint weaken the ligaments, making them more prone to tearing.
ACL tears may lead to pain, discomfort, swelling, joint instability, and reduced range of motion. These injuries can also alter knee mechanics, impacting how loads are distributed during movement.
Over time, this can put undue pressure on certain knee parts, leading to faster wear and tear. According to a 2023 study, the risk of developing osteoarthritis is over eight times higher in people who experienced an ACL rupture compared to healthy individuals.
A torn ACL can restrict everyday activities and lead to disability. Among athletes, ACL tears can also shorten career length and limit the level of sports participation, according to one study. Tears are categorized depending on their severity:
Grade 1 ACL Sprain
A grade 1 ACL sprain is the mildest form of injury. The ligament is slightly stretched but retains its integrity. This type of sprain often results from minor twisting motions or low-impact activities.
The ligament fibers experience minor damage and minimal tearing. This causes mild pain and some swelling, but knee stability is generally unaffected. Recovery typically involves rest, ice, and physical therapy.
Grade 2 ACL Tear
A grade 2 ACL or partial tear involves a more significant portion of the damaged ligament. However, the ligament fibers are not fully severed and remain relatively aligned.
This injury typically results from moderate force, like a sharp twist or awkward landing. It usually causes noticeable pain, swelling, and some knee instability. Treatment may involve bracing, physical therapy, and sometimes surgery to restore function.
Grade 3 ACL Tear
A grade 3 ACL tear is a complete tear where the ligament is completely severed or ruptured. This severe injury often results from intense trauma, such as a high-impact fall, car accident, or sudden change of direction.
The ligament fibers are completely ruptured, causing pain, significant swelling, and severe knee instability. Surgical reconstruction is commonly required to regain knee stability and function.
Types Of Surgery For ACL Injuries
ACL injuries can vary in severity and nature. While a mild sprain rarely requires surgery, more severe tears are commonly treated surgically. Around 400,000 ACL reconstructions are performed annually in the United States.
These surgical interventions aim to restore knee stability and function. Physicians may opt for different surgical techniques, including ACL repair or reconstruction. Each of these procedures carries risks. So, it is crucial for both patients and their physicians to carefully consider all treatment options before opting for surgery.
ACL Repair Surgery
The first ACL repair surgery was performed by Sir Arthur Mayo-Robson in 1895. In the following years, it became increasingly popular as a new way to address torn ACLs.
However, historically, this procedure often resulted in ongoing pain and instability, so surgeons began to advise patients against it. In 1927, Erwin Payr introduced the first ACL reconstruction surgery to address the shortcomings of ACL repair surgery.
Today, technical advancements in ACL repair may lead to satisfactory outcomes. However, success rates for ACL repair are still lower than ACL reconstruction. Complications include residual instability and repair failure.
ACL Repair Procedure
During the ACL repair procedure, the surgeon makes small cuts around the knee. A camera is then used to view the inside of the knee and accurately diagnose the issue. The surgeon then inserts surgical instruments through small incisions to repair the ligament.
Usually, ACL repair involves suturing the torn ligament fibers back together. Screws may also be used to fix the ligament in place and support recovery.
After the surgery, the knee is stitched up and bandaged. The entire surgery usually takes one to two hours. Following surgery, a recovery plan typically includes physical therapy and rest to support healing and knee strength.
Considerations And Risks
ACL repair surgery is sometimes recommended for isolated or mild tears. It is often chosen for individuals without other knee injuries and who are not extremely active, such as aging adults.
This procedure often leads to shorter recovery periods compared to ACL reconstruction. However, patients should be aware of potential risks and complications. These include infection, bleeding, knee stiffness, and blood clots.
The procedure’s success depends on the body’s capacity to heal the ligament after suturing. However, this natural healing is not always sufficient. Possible reasons include:
- Movement in the knee can disrupt the sutures.
- The environment around the ligament may lack the necessary blood supply for healing.
- Over time, the sutures can potentially damage nearby structures, such as the meniscus.
Post-Operative Pain Management And Recovery Expectations
Post-operative pain management is critical after ACL repair. Pain medications, such as anti-inflammatories, help control discomfort. At-home remedies, like ice packs and elevation, can reduce swelling and improve mobility. A knee brace may often provide additional support and prevent knee injuries during healing.
Typically, patients can start with light activities within a few weeks. However, full recovery normally takes six months to a year.
ACL Reconstruction Surgery
ACL reconstruction is a surgical procedure to replace a torn ACL in the knee. Unlike ACL repair, which attempts to stitch the torn ligament back together, reconstruction involves replacing the damaged ligament with a graft.
Today, this is a common approach for severe ACL tears. One study estimates that around 22.6% of patients with an ACL injury will undergo ACL reconstruction surgery within three years of their diagnosis.
Reconstruction involves using a graft, a piece of tissue that replaces the damaged ligament. Different types of grafts are used in ACL reconstruction:
- Autograft. An autograft uses the patient’s tissue to replace a torn ligament. Compared to other graft types, an autograft is less likely to re-tear. It is often chosen for younger, active patients, like athletes under 30. However, it involves a longer recovery time and additional surgical sites to harvest the tissue to replace the ligament.
A 2001 study suggests that possible complications at the donor site, or where the autograft harvest occurs, may include chronic pain, reduced mobility, and surgical injury to surrounding tissues and nerves.
Autografts are usually sourced from other tendons:
- Patellar tendon autograft. A procedure that uses the middle section of the kneecap tendon to provide strong fixation, making it suitable for athletes.
- Hamstring tendon autograft. Uses portions of tendons from the hamstring muscles. It is a versatile option suitable for many patients and has a less painful recovery.
- Quadriceps tendon autograft. This procedure uses portions of the quadriceps tendon. It provides a thicker graft, which is useful for larger patients.
- Allograft. An allograft uses tissue from a donor. Compared to autografts, it often leads to less immediate postoperative pain and a faster return to daily activities.
Allografts are processed in high-quality tissue banks to ensure safety. However, they have a higher risk of re-tear, making them more suitable for older patients or those with less active lifestyles. A 2020 study suggests that allografts have significantly higher failure rates than autografts.
Surgeons may also use a synthetic graft, which involves replacing the ligament with synthetic materials like carbon fiber or Teflon. Each of these graft types has unique benefits and risks. A physician will consider each option based on the patient’s age, level of activity, lifestyle, and general health.
ACL reconstruction is sometimes referred to as the gold standard for treating severe ACL injuries. However, new research shows that this surgery may not be as effective or safe as previously thought. Studies highlight that ACL reconstruction aggravates the cartilage damage that occurs at the time of an ACL injury.
Additionally, this surgery may lead to long-term effects, including an increased risk of arthritis, persistent knee instability, reduced knee performance, delayed return to sports, and shorter athletic careers.
ACL Reconstruction Surgery Techniques
ACL reconstruction techniques vary based on the patient’s needs and the severity of the tear. There are two main types of ACL reconstruction surgeries:
- Open surgery. This method involves a larger incision. It allows the surgeon direct access to the knee joint. It provides a clear view and space for more precise intervention.
- Arthroscopic surgery. Arthroscopy is less invasive than open surgery. It involves using small incisions and a camera (arthroscope) to view the inside of the knee. This approach typically results in less scarring and a quicker recovery.
Generally, ACL reconstruction involves passing the graft through small tunnels drilled into the thigh bone (femur) and shinbone (tibia). These tunnels will hold the graft, which will later replace the damaged ACL. The graft is carefully positioned and anchored in place using screws.
Different ACL reconstruction techniques include:
- Single-bundle reconstruction. The ACL has two main bundles. In the single-bundle ACL reconstruction focuses on replacing just the damaged bundle. In this surgery, only one graft is passed through the tunnels. It is often chosen for its simplicity and shorter surgical time.
- Double-bundle reconstruction. This method involves replacing both the anteromedial and posterolateral bundles. It helps mimic the ACL’s natural structure and mechanics. In this surgery, two grafts are passed through two separate tunnels. This technique offers better knee stability and is suitable for athletes and patients requiring high knee functionality.
- Tunnel placement variations. Customizing the placement of the tunnels helps optimize the position of the graft. This can improve joint stability and function. A 2021 study also suggests that tunnel placement choices impact the ability of the reconstructed ACL to absorb the load needed to keep the knee stable. Variations occur in the number of tunnels and their position on the femur and tibia.
- Fixation methods. Grafts can be secured with screws, buttons, or internal braces. The choice depends on the graft type, surgeon preference, and patient-specific factors.
- Meniscus repair. Meniscus repair may be performed alongside ACL reconstruction if there is meniscal damage. This repair helps preserve knee function and decrease the risk of arthritis. The surgeon may use sutures or special meniscal repair devices to stitch the torn meniscus back together. Addressing meniscus tears during ACL surgery can improve overall knee stability and outcomes.
Considerations And Risks
Surgeons will consider several factors when choosing ACL reconstruction over ACL repair. These include the presence of multiple ligament injuries and knee instability, as well as the patient’s level of activity, goals, and overall health.
Generally, ACL reconstruction leads to better stability and function for severe conditions. However, it also carries risks and long-term complications. These include the following:
- Infection. Infection can occur from bacteria entering the surgical site. It is estimated to occur in around 1.2% of ACL surgeries.
- Damage to other knee components. Surgery can inadvertently harm surrounding tissues, tendons, or cartilage.
- Increased risk of arthritis. Surgery can speed up the wear and tear of the knee joint and change its mechanics. Over time, this can lead to joint degeneration and arthritis.
- Persistent pain. Some patients experience long-term pain even after successful surgery. One study found that 6.2% of patients experience chronic knee pain after ACL reconstruction.
- Graft failure. The new ligament may not integrate well or may tear again, necessitating further intervention. One study shows that approximately 7.7% of ACL reconstruction patients required revision surgeries at a six-year follow-up.
Post-Operative Pain Management and Recovery Expectations
Recovery from ACL reconstruction varies depending on the patient’s overall health and goals. Usually, it is possible to return to daily activities and sedentary jobs within a few weeks of the operation. However, returning to sport can take a year or longer.
One study found that only 65% of patients return to pre-injury levels of activity, and just over half return to competitive sports. Generally, it takes from nine to 12 months to return to any sports activity. New recovery methods provide an accelerated approach, promising a return to sports within six months.
During recovery, patients can use at-home remedies, pain medications, and bracing. These methods help support healing and prevent re-injury. Physicians will also prescribe physical therapy to help restore knee function and strength.
Conditions That ACL Surgery Can Address
Can Patients Avoid ACL Tear Surgery?
Sometimes, it is possible to avoid surgery by treating the ACL tear with conservative methods. These include:
- RICE. Rest, ice, compression, and elevation help reduce swelling and pain.
- Physical therapy. Strengthens the muscles around the knee to provide stability.
- Bracing. Offers support and prevents further injury during daily activities.
- Pain medication. Anti-inflammatory drugs help manage pain and swelling.
- Activity modification. Adjusting or avoiding high-risk activities reduces stress on the ACL and supports healing.
- Regenerative therapy options. Interventional orthobiologics, like the procedures using Regenexx proprietary methods, help harness the body’s natural healing ability.
Perc-ACLR: The Regenexx Approach For ACL Injuries
Procedures using Regenexx injectates for ACL injuries provide an alternative to traditional ACL reconstruction surgery. Procedures using Regenexx Perc-ACLR injectate do not involve surgery and reduce the need for prescription medications.
Depending on the severity of the tear, the customized injectate may be the patient’s own bone marrow that contains mesenchymal stem cells or concentrated platelets from the patient’s own blood.
These orthobiologics are injected into the damaged ACL area to enhance the body’s natural ability to repair tissue. Mesenchymal stem cells are typically used for more severe tears and platelet-rich plasma for smaller injuries.
This approach aims to preserve the original tissue and may offer a quicker recovery with fewer complications than traditional surgery.
Discover A Non-Surgical Option For ACL Injuries
Regenexx provides a patented protocol for ACL tear treatment. It utilizes interventional orthobiologics to support the body’s natural healing process. This proprietary method helps reduce the need for invasive surgery and prescription drugs, like opioids.
Consult a physician in the licensed Regenexx network to discuss if this customized, non-surgical option is right for your ACL injury.

Medically Reviewed By:
