ACL Tear Repair Without Surgery
Are You a Regenexx Candidate?Do you have an MRI-confirmed partial or complete tear of the anterior cruciate ligament (ACL) and have been told surgery is your only option?
Perc-ACLR (percutaneous ACL repair) is a procedure that Regenexx created to treat full and partial anterior cruciate ligament tears non-surgically. ACL tears are one of the more common knee injuries treated by physicians in the licensed Regenexx network, and many non-retracted full and partial tears can be treated in all but the most serious cases.
Repair of ACL tear without surgery
ACL Tear Recovery Time Without Surgery
You have some important things to consider in making the best decision for your recovery, your return to sport or normal activity, and, ultimately, your long-term health. At Regenexx, the goal is to save your ACL, not replace it. The existing research and significant expertise support the possibility for successful natural healing of ACL injuries.
The Per-ACLR is a highly precise X-ray guided injection of your own orthopedic bone marrow concentrate and can be completed in one day. It is far less invasive than surgery, and generally requires far shorter recovery times.
| Perc-ACLR | Surgery | |
|---|---|---|
| Procedure Invasiveness | Much less | Much more |
| Return to Sports | 3 to 6 months | 1 year |
| Keep your ACL | Yes | NO |
| Recovery | Brace, much less extensive PT | Crutches, brace, extensive PT |
How Does The Regenexx Approach Work?
At Regenexx, we invented a new approach to orthopedic care we call Interventional Orthopedics. This minimally invasive alternative to ACL surgery uses ultrasound-guided technology to precisely inject your own bone marrow concentrate — which contains stem cells — directly where it’s needed in the joint.
The cells in your bone marrow concentrate work at the site of your injury to promote your body’s natural healing abilities to treat the tear and avoid surgery1.
Regenexx For ACL Tears: Perc-ACLR
The procedure usually occurs over one day. First, your doctor will extract a small amount of bone marrow using precise imaging guidance, a specialized extraction technique unique to Regenexx.
Once the marrow is drawn and processed by a Regenexx lab technician, you will have time to relax before the reinjection of the harvested bone marrow concentrate into your ACL, done three to six hours later.
Specialized local anesthesia is applied before the reinjection using fluoroscopy (real-time imaging guidance). MRI imaging along with X-ray contrast is used to carefully map the torn ligament during the procedure, providing a “roadmap” for your doctor to implant bone marrow concentrate into the damaged areas of the ligament.
After the procedure, your joint will be sore for one to three days, but the pain will become less severe and less frequent within five to seven days. Most patients note that they see improvement to their ACL within a month and can resume light activities and begin physical therapy.
Am I a candidate?Note: Like all medical procedures, procedures using Regenexx lab processes have a success and failure rate. Patient reviews and testimonials on this site should not be interpreted as a statement on the effectiveness of treatments for anyone else.
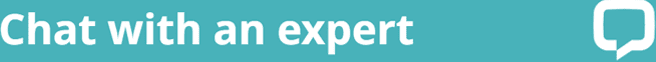
BEFORE and AFTER MRI Images
Take a look at the outcomes of patients who had a procedure with Regenexx protocol instead of ACL surgery.
The BEFORE shows a torn ACL. The area should be a dark band going diagonally, as shown on the AFTER.

FAQs
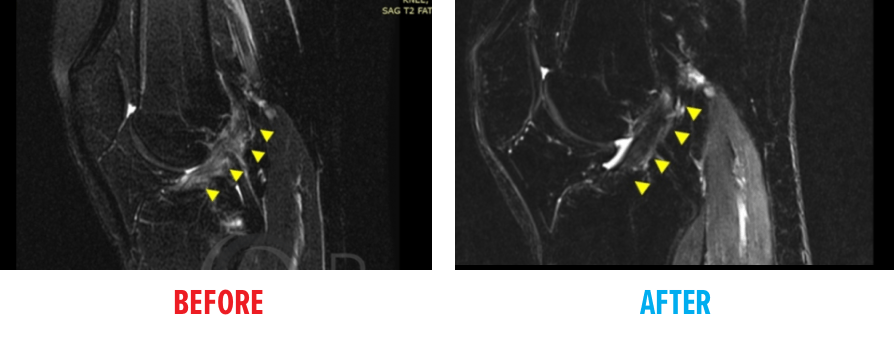
Knee joint anatomy showing ACL
There are two cruciate (meaning “cross-shape”) ligaments found inside your knee joint that work to stabilize it. They cross each other to form an X with the anterior cruciate ligament (ACL) in front and the posterior cruciate ligament (PCL) in the back. The ACL prevents the knee from sliding forward and the PCL from sliding backward.
ACL surgery is not generally an emergency procedure unless there is extensive damage to other structures, significant instability, or intense pain. Generally, if there is some joint stability, adults can delay surgery for a month or two. For young athletes, the waiting period may be slightly less and is often determined by a desire to get the injury repaired in the hope of returning to sports quickly. For some patients, delaying surgery and trying physical therapy first may help the healing process. If that fails, there are nonsurgical options, such as Perc-ACLR, to consider prior to resorting to surgery.
Research has also shown that ACL sprains and even complete ACL tears can regrow and heal on their own,2 particularly if interventional orthopedic procedures such as the Perc-ACLR procedure are utilized. These techniques do not require surgery and employ your body’s natural healing agents to repair your ACL injury. So, if your body can heal your ACL naturally, why would you choose surgery?
ACL sprains, tears, and ruptures are all essentially the same thing, and the terms are used interchangeably. Injured knee ligaments are all considered “sprains” and are graded on a severity scale.
- Grade 1 Sprains: The ligament is mildly damaged in a Grade 1 Sprain. It has been slightly stretched but is still able to help keep the knee joint stable.
- Grade 2 Sprains: A Grade 2 Sprain stretches or mildly tears the ligament to a point that the ACL becomes loose. This is also sometimes referred to as a partial tear of the ligament.
- Grade 3 Sprains: This type of sprain is most commonly referred to as a complete tear of the ligament. The ligament has been split into two pieces, and the knee joint is unstable.
An ACL rupture is another term often used to describe a tear. However, ruptures of the ACL are generally equated with complete full-thickness tears (Grade 3 Sprains) and are often associated with ligament deformity or full retraction.
Statistically, only about half of athletes who have ACL reconstruction regain complete function after rehab and are able to return to sport at the same level. The other half regain knee stability but not normal biomechanics or proprioception equal to the noninjured knee. Functional limitations in daily life are also possible. It is always advisable to get a second opinion on the need for surgery as there are a number of documented complications associated with conventional ACL reconstruction surgery and your injury could have been misdiagnosed. While surgery might be the right procedure for some ACL injuries, the vast majority of people could avoid it.
- Approximately 17 percent of adults will experience anterior knee pain or pain on kneeling, and between 5 percent and 29 percent will experience graft failure and loss of knee joint stability, with younger patients having higher rates. Other potential complications include knee stiffness or loss or range of motion (approximately 5 percent), painful hardware (approximately 6 percent), infection (approximately 1 percent to 2 percent) or patellar tendon rupture/patellar fracture in the case of bone-to-bone grafts.3-6
- Increased youth participation in high-intensity elite sports has resulted in much higher rates of ACL repair surgery in young teens, however, research is now suggesting that postsurgery complications may be worse in kids than adults. If preserving the natural physical gifts you were born with and “keeping original parts and structures intact” is your goal, you may want to consider a nonsurgical alternative like Perc-ACLR.
- A large analysis of 160 clinical trials demonstrated higher rates of postsurgery complications in young teens undergoing ACL repair and found that the risk for growth disturbances, skeletal deformities, and ligament rerupture requiring a second surgery was much higher in this young (average age = 13), skeletally immature population.7
- A 2010 Swedish research study also challenged the concept that surgery is the only way to heal ACL tears. They demonstrated that 60 percent of the athletes (average age = 26) who elected a strict physical therapy regimen over surgery never needed to have the ACL replaced and were still able to play sports.8
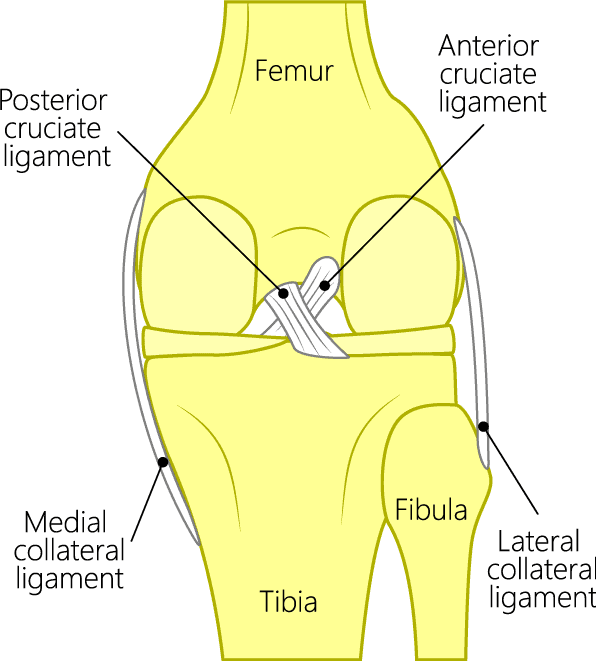
When it comes to ACL tears, there are numerous classifications and subtypes. In regenerative medicine, however, we define these tears by 3 types: partial thickness, full thickness non-retracted, and full thickness retracted. Both partial thickness and full-thickness, non-retracted tears can be treated with regenerative medicine utilizing the Regenexx knee Perc-ACL procedure to heal your tear without surgery. Full-thickness, retracted tears will likely require surgical repair to heal properly.
- Partial Thickness ACL Tear
A partial-thickness ACL tear is one that hasn’t torn completely through. It’s exactly as it sounds—on imaging, we would see that a portion of the ligament is still intact. - Full-Thickness Non-retracted ACL Tear
A full thickness nonretracted ACL tear is one that has torn all the way through; however, it hasn’t completely pulled apart or snapped back like a rubber band would. The ligament is certainly fully torn, but the pieces are still in place. - Full-Thickness Retracted ACL Tear
A full thickness retracted ACL tear is one that has torn through, but in this case, the two pieces have pulled apart or maybe even snapped back like a rubber band.
ACL tears
Get started to see if you are a Regenexx candidate
To talk one-on-one with one of our team members about how the Regenexx approach may be able to help your orthopedic pain or injury, please complete the form below and we will be in touch with you within the next business day.
References
1. Centeno C, Markle J, Dodson E, Stemper I, Williams C, Hyzy M, Ichim T, Freeman M. Symptomatic anterior cruciate ligament tears treated with percutaneous injection of autologous bone marrow concentrate and platelet products: a non-controlled registry study. J Transl Med. 2018 Sep 3;16(1):246. doi: 10.1186/s12967-018-1623-3. PMID: 30176875. PMID: 30176875. [Google Scholar]
2. Costa-Paz M, Ayerza MA, Tanoira I, Astoul J, Muscolo DL. Spontaneous healing in complete ACL ruptures: a clinical and MRI study. Clin Orthop Relat Res. 2012 Apr;470(4):979-85. doi: 10.1007/s11999-011-1933-8. PMID: 21643922. [Google Scholar]
3. Freedman KB, D’Amato MJ, Nedeff DD, Kaz A, Bach BR Jr. Arthroscopic anterior cruciate ligament reconstruction: a metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med. 2003 Jan-Feb;31(1):2-11. doi: 10.1177/03635465030310011501. PMID: 12531750. [Google Scholar]
4. Webster KE, Feller JA, Leigh WB, Richmond AK. Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med. 2014 Mar;42(3):641-7. doi: 10.1177/0363546513517540. Epub 2014 Jan 22. PMID: 24451111. [Google Scholar]
5. Burks RT, Friederichs MG, Fink B, Luker MG, West HS, Greis PE. Treatment of postoperative anterior cruciate ligament infections with graft removal and early reimplantation. Am J Sports Med. 2003 May-Jun;31(3):414-8. doi: 10.1177/03635465030310031501. PMID: 12750136. [Google Scholar]
6. Kovacic JJ in Complications of Anterior Cruciate Ligament Surgery, AAOS Monograph Series 2005. Accessed August 25, 2020.
7. Wong SE, Feeley BT, Pandya NK. Complications After Pediatric ACL Reconstruction: A Meta-analysis. J Pediatr Orthop. 2019 Sep;39(8):e566-e571. doi: 10.1097/BPO.0000000000001075. PMID: 31393290. [Google Scholar]
8. Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS. A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med. 2010 Jul 22;363(4):331-42. doi: 10.1056/NEJMoa0907797. Erratum in: N Engl J Med. 2010 Aug 26;363(9):893. PMID: 20660401. [Google Scholar]