More Fake PRP Studies
Credit: Shutterstock
I’ve covered a few different “PRP” studies that didn’t actually use real PRP. However, none were as ridiculous as a study that was recently published in JAMA on knee arthritis. Let’s dig in.
When is PRP not PRP?
PRP stands for platelet-rich plasma. The idea is supposed to be that PRP concentrates platelets many times over their usual concentration in your blood. That’s because platelets contain all sorts of goodies including growth factors and other extracellular vesicles that can assist tissue healing. Hence, concentrating the platelets means more healing power.
However, the many convenient bedside PRP systems out there all do this with varying levels of efficiency. Most can only achieve concentrations of 3-7X (times concentration) and some are really bad, unable to achieve even the minimum definition of PRP, which is 2X based on a seminal paper published by Marx in 2004 (21).
Why would a doctor buy a bad PRP system like this? Because people buy bad products all the time and medicine isn’t that different than anything else. In addition, medicine has aggressive sales reps who push various machines based on their existing physician relationships and the amount of commission paid by the manufacturer.
Why Would You Study PRP Out of a Machine that Makes Piss Poor PRP?
As I have blogged before, studies that use this non-PRP or very low concentration (underdosed) PRP have been appearing lately. The study designs are generally good except for one problem, the PRP is bad. Today we’ll dig deeper into a new knee arthritis study published in the Journal of the American Medical Association (JAMA).
The Most Recent Study
The new study looked at hundreds of knee arthritis patients treated with what they claimed were PRP injections (1). On the surface, it’s a well-designed and documented study with a fancy name. However, unlike more than a dozen randomized controlled trials before it that showed that PRP was an effective treatment for knee arthritis, this one didn’t find that to be true (3-20). So what is the problem? The problem is the study didn’t actually use PRP.
The name of the PRP kit the authors used is called RegenLab. Independent research was performed in 2014 on that system. Here we see how it performed in that study:

Note in the red and yellow highlighted box that the RegenLab PRP kit was only able to produce about 1.6X concentration of platelets, therefore not meeting the minimum requirements to be PRP of 2X (2). Given that this paper was very much available to the lead authors of this study when in the design phase, who in their right mind would pick this commercial system to study?
In addition, since these authors reported the concentration of platelets in the “PRP” samples they injected, we can also look at that data. This is from the JAMA knee arthritis paper:
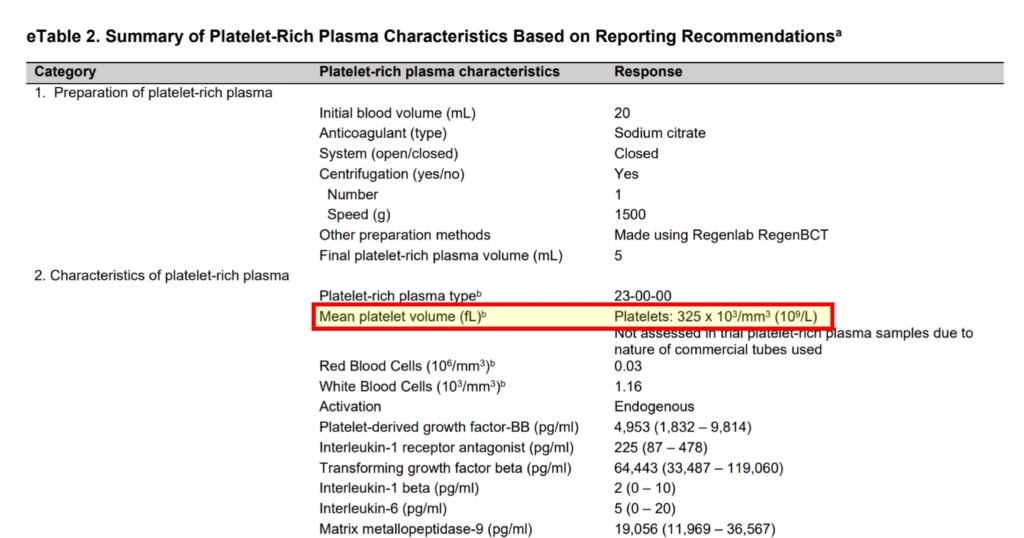
The average platelet count was 325. Why is that a problem? The average platelet count in normal blood is 150-450. Hence, there was no significant concentration of platelets that happened in this study. When you do the math, the concentration factor was LESS than that of the prior study on RegenLab PRP at a ridiculously low 1.2!
PRP Concentration vs Age
As I’ve blogged before, our published data shows that older patients need higher concentrations of PRP. What was the average age in this study? 62 years of age. Hence, a PRP concentration this low in a patient population this old was doomed to failure before the trial began.
Why Does This Keep Happening?
That’s a great question. Let’s look at the authors of this study. The lead author is a Ph.D. not licensed to practice medicine, so again, she has ZERO practical experience in treating patients with PRP. Which always seems to be the main issue here, people with no or very limited experience with the day-to-day use of orthobiologics who perform studies outside of their areas of expertise.
The bigger question is why did a major journal green light this study for publication? Given that it didn’t actually use anything that any reasonable physician would consider PRP? They could have easily looked up the data on the RegenLab kit or simply looked at the platelet count as I just did.
The upshot? The fake PRP study problem is becoming a real issue. Why? Because people who have no desire to look into the details of what was studied will assume that JAMA did their due diligence on the study when in fact, the journal failed to perform even basic peer review. The media will focus on reading the abstract of what on the surface an elegant study, but what in fact is a bait and switch.
______________________________________
(1) Bennell KL, Paterson KL, Metcalf BR, et al. Effect of Intra-articular Platelet-Rich Plasma vs Placebo Injection on Pain and Medial Tibial Cartilage Volume in Patients With Knee Osteoarthritis: The RESTORE Randomized Clinical Trial. JAMA. 2021;326(20):2021–2030. doi:10.1001/jama.2021.19415
(2) Magalon J, Bausset O, Serratrice N, Giraudo L, Aboudou H, Veran J, Magalon G, Dignat-Georges F, Sabatier F. Characterization and comparison of 5 platelet-rich plasma preparations in a single-donor model. Arthroscopy. 2014 May;30(5):629-38. doi: 10.1016/j.arthro.2014.02.020. PMID: 24725317.
(3) Uslu Güvendi E, Aşkin A, Güvendi G, Koçyiğit H. Comparison of Efficiency Between Corticosteroid and Platelet Rich Plasma Injection Therapies in Patients With Knee Osteoarthritis. Arch Rheumatol. 2017;33(3):273–281. Published 2017 Nov 2. doi: 10.5606/ArchRheumatol.2018.6608
(4) Tavassoli M, Janmohammadi N, Hosseini A, Khafri S, Esmaeilnejad-Ganji SM. Single- and double-dose of platelet-rich plasma versus hyaluronic acid for treatment of knee osteoarthritis: A randomized controlled trial. World J Orthop. 2019;10(9):310–326. Published 2019 Sep 18. doi: 10.5312/wjo.v10.i9.310
(5) Joshi Jubert N, Rodríguez L, Reverté-Vinaixa MM, Navarro A. Platelet-Rich Plasma Injections for Advanced Knee Osteoarthritis: A Prospective, Randomized, Double-Blinded Clinical Trial. Orthop J Sports Med. 2017;5(2):2325967116689386. Published 2017 Feb 13. doi: 10.1177/2325967116689386
(6) Raeissadat SA, Rayegani SM, Hassanabadi H, et al. Knee Osteoarthritis Injection Choices: Platelet- Rich Plasma (PRP) Versus Hyaluronic Acid (A one-year randomized clinical trial). Clin Med Insights Arthritis Musculoskelet Disord. 2015;8:1–8. Published 2015 Jan 7. doi: 10.4137/CMAMD.S17894
(7) Montañez-Heredia E, Irízar S, Huertas PJ, et al. Intra-Articular Injections of Platelet-Rich Plasma versus Hyaluronic Acid in the Treatment of Osteoarthritic Knee Pain: A Randomized Clinical Trial in the Context of the Spanish National Health Care System. Int J Mol Sci. 2016;17(7):1064. Published 2016 Jul 2. doi: 10.3390/ijms17071064
(8) Görmeli G, Görmeli CA, Ataoglu B, Çolak C, Aslantürk O, Ertem K. Multiple PRP injections are more effective than single injections and hyaluronic acid in knees with early osteoarthritis: a randomized, double-blind, placebo-controlled trial. Knee Surg Sports Traumatol Arthrosc. 2017 Mar;25(3):958-965. doi: 10.1007/s00167-015-3705-6.
(9) Lana JF, Weglein A, Sampson SE, et al. Randomized controlled trial comparing hyaluronic acid, platelet-rich plasma and the combination of both in the treatment of mild and moderate osteoarthritis of the knee. J Stem Cells Regen Med. 2016;12(2):69–78. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5227106/
(10) Tavassoli M, Janmohammadi N, Hosseini A, Khafri S, Esmaeilnejad-Ganji SM. Single- and double-dose of platelet-rich plasma versus hyaluronic acid for treatment of knee osteoarthritis: A randomized controlled trial. World J Orthop. 2019;10(9):310–326. Published 2019 Sep 18. doi: 10.5312/wjo.v10.i9.310
(11) Lin KY, Yang CC, Hsu CJ, Yeh ML, Renn JH. Intra-articular Injection of Platelet-Rich Plasma Is Superior to Hyaluronic Acid or Saline Solution in the Treatment of Mild to Moderate Knee Osteoarthritis: A Randomized, Double-Blind, Triple-Parallel, Placebo-Controlled Clinical Trial. Arthroscopy. 2019 Jan;35(1):106-117. doi: 10.1016/j.arthro.2018.06.035.
(12) Huang Y, Liu X, Xu X, Liu J. Intra-articular injections of platelet-rich plasma, hyaluronic acid or corticosteroids for knee osteoarthritis : A prospective randomized controlled study. Orthopade. 2019 Mar;48(3):239-247. doi: 10.1007/s00132-018-03659-5.
(13) Di Martino A, Di Matteo B, Papio T, Tentoni F, Selleri F, Cenacchi A, Kon E, Filardo G. Platelet-Rich Plasma Versus Hyaluronic Acid Injections for the Treatment of Knee Osteoarthritis: Results at 5 Years of a Double-Blind, Randomized Controlled Trial. Am J Sports Med. 2019 Feb;47(2):347-354. doi: 10.1177/0363546518814532.
(14) Yu W, Xu P, Huang G, Liu L. Clinical therapy of hyaluronic acid combined with platelet-rich plasma for the treatment of knee osteoarthritis. Exp Ther Med. 2018;16(3):2119–2125. doi: 10.3892/etm.2018.6412
(15) Buendía-López D, Medina-Quirós M, Fernández-Villacañas Marín MÁ. Clinical and radiographic comparison of a single LP-PRP injection, a single hyaluronic acid injection and daily NSAID administration with a 52-week follow-up: a randomized controlled trial. J Orthop Traumatol. 2018;19(1):3. Published 2018 Aug 20. doi: 10.1186/s10195-018-0501-3
(16) Su K, Bai Y, Wang J, Zhang H, Liu H, Ma S. Comparison of hyaluronic acid and PRP intra-articular injection with combined intra-articular and intraosseous PRP injections to treat patients with knee osteoarthritis. Clin Rheumatol. 2018 May;37(5):1341-1350. doi: 10.1007/s10067-018-3985-6.
(17) Louis ML, Magalon J, Jouve E, Bornet CE, Mattei JC, Chagnaud C, Rochwerger A, Veran J3, Sabatier F. Growth Factors Levels Determine Efficacy of Platelets Rich Plasma Injection in Knee Osteoarthritis: A Randomized Double Blind Noninferiority Trial Compared With Viscosupplementation. Arthroscopy. 2018 May;34(5):1530-1540.e2. doi: 10.1016/j.arthro.2017.11.035.
(18) Lisi C, Perotti C, Scudeller L, Sammarchi L, Dametti F, Musella V, Di Natali G. Treatment of knee osteoarthritis: platelet-derived growth factors vs. hyaluronic acid. A randomized controlled trial. Clin Rehabil. 2018 Mar;32(3):330-339. doi: 10.1177/0269215517724193
(19) Cole BJ, Karas V, Hussey K, Pilz K, Fortier LA. Hyaluronic Acid Versus Platelet-Rich Plasma: A Prospective, Double-Blind Randomized Controlled Trial Comparing Clinical Outcomes and Effects on Intra-articular Biology for the Treatment of Knee Osteoarthritis. Am J Sports Med. 2017 Feb;45(2):339-346. doi: 10.1177/0363546516665809.
(20) Kaminski R, Maksymowicz-Wleklik M, Kulinski K, Kozar-Kaminska K, Dabrowska-Thing A, Pomianowski S. Short-Term Outcomes of Percutaneous Trephination with a Platelet Rich Plasma Intrameniscal Injection for the Repair of Degenerative Meniscal Lesions. A Prospective, Randomized, Double-Blind, Parallel-Group, Placebo-Controlled Study. Int J Mol Sci. 2019 Feb 16;20(4):856. doi: 10.3390/ijms20040856. PMID: 30781461; PMCID: PMC6412887.
(21) Marx RE. Platelet-rich plasma: evidence to support its use. J Oral Maxillofac Surg. 2004 Apr;62(4):489-96. doi: 10.1016/j.joms.2003.12.003. PMID: 15085519.

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
