Can a Large Cervical Disc Bulge Be Treated with Platelets?

Credit: Shutterstock
Just 5 years ago, the spine cases that I would accept for treatment with precise image-guided orthobiologics were determined by the severity of the MRI. Meaning more severe cases of disc bulges, stenosis, and degeneration were turned down and told to seek surgery. However, as time when on, some cases seemed to break that mold and since then, I’ve pushed the envelope of what this technology can do in the spine. This is one of those cases that broke the mold. Let’s dig in.
Platelet DDD Spine Treatment
I always tell patients that my job is to pick the least invasive thing that’s the most likely to work. Oftentimes that’s a platelet-based procedure rather than one derived from bone marrow that contains stem cells. The DDD treatment for the spine involves using:
- Ultra-high Dose Leurkocyte Poor Platelet-rich Plasma (PRP)
- High Dose Platelet Lysate (PL)
- Platelet-Poor Plasma (PPP)
Basically, these three different things can’t be made by bedside kits used by 99% of physicians, so they are created in an on-site lab like the one used by Regenexx affiliates. The doctor begins with a blood draw and then the PRP is injected into the damaged facet joints, the PL is injected epidural around irritated nerves and into lax ligaments, and then finally the PPP is injected into atrophied muscles.
If you want to learn more, watch my video below:
The above video is about the lumbar spine, but the same principles apply to the cervical spine.
Mike’s Neck
I love to get random emails from old patients telling me how they’ve progressed. This one recently came from Mike, a patient with cervical stenosis and a large bulging disc in his neck:
“I’ve come a long way since you first saw me back in Feb. My pain is virtually gone. Strength has returned to normal. Numbness is infrequent. However, the nerve does get irritated with certain movements, much less than before. I have been taking it easy because when I move a lot it gets slightly irritated.
I feel at this point I can forgo surgery. But since I have a spot on your schedule, do you believe one last Tx would benefit me at this point?
My life has greatly improved because of your services. I can’t imagine where I would be without you. Thank you so much!”
So let’s review where Mike started.
A Really Bad Neck MRI
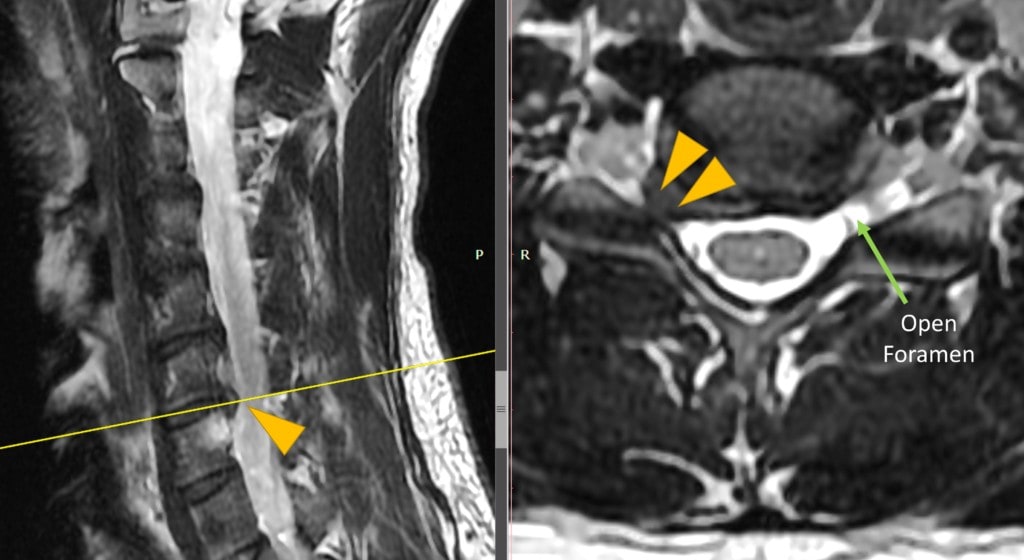
Mike began getting severe neck pain and right-hand numbness after bike riding. When I saw the MRI above, I was concerned that while our cervical DDD platelet procedure could help, the fact that the foramen was closed off by a huge disc bulge may make what we do ineffective. As you can see above, on the left the sagittal image shows a disc bulge at the arrow. The image on the right shows an axial image where the arrows point to a huge disc bulge into the foramen (the place where the spinal nerve exits). Despite these challenges, we decided to use the platelet DDD procedure.
Mike’s Progress
Mike made great progress after the first treatment with less neck pain and less hand numbness. By the second treatment he was riding his bike and the third extended what he could do. You can see by his email above where he is after the last treatment.
A Change in How We Look at MRIs
Since Mike and many other patients, how I determine who is a candidate for this procedure has changed. Before I would very much look at the severity of the MRI and often tell patients with more severe degenerative disc disease that they needed surgery. Now I realize that these MRI findings are likely less important in predicting who will respond to this type of therapy. Now I have dozens of examples of patients with severe degenerative issues that have positively responded to the DDD procedure.
The upshot? It’s great to see that Mike has done well and that we can help a broader spectrum of patients with the game-changing DDD procedure. I look forward to Mike’s fourth treatment and keeping him away from invasive neck surgery!

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
