Can You Avoid Spinal Stenosis Surgery?
How do you avoid spinal stenosis surgery? How effective is spinal stenosis surgery? How dangerous is spinal stenosis surgery? How long is recovery after spinal stenosis surgery? What activities should be avoided with spinal stenosis? Is walking bad for spinal stenosis? Let’s dig in.
What is Spinal Stenosis?
Rumruay/Shutterstock
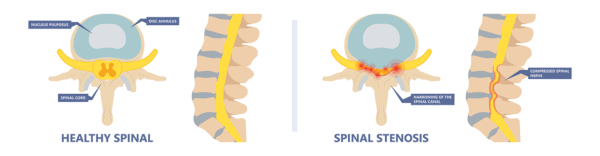
When you hear a doctor say “spinal stenosis” oftentimes what that means is central canal stenosis. There is a hole that runs through the spine bones (vertebrae) which is where the spinal cord and nerves run. This hole can become smaller with arthritis, bone spurs, swollen ligaments, and/or disc bulges (5). When this happens, it’s called spinal stenosis. To understand this more, watch my video on the neck (which is similar in the back):
How is Spinal Stenosis Treated?
For patients who have difficulty standing without symptoms and who fail physical therapy, spinal stenosis is often treated with surgery to decompress the area (6). This often means removing bone, disc, and ligaments around the tight spot in the central canal. Oftentimes a fusion is added, which is were hardware is inserted to bolt the spine bones together.
How Effective is Spinal Stenosis Surgery?
To decide if you want to avoid spinal stenosis surgery, we have to first review if the procedure works. The SPORT trial looked at patients who had spinal stenosis surgery versus those who didn’t (1). Interestingly there was no difference between the patients once they got to four years plus out form the procedure. Another high-level study randomized patients to stenosis surgery versus physical therapy, but the surgery patients didn’t do any better than those who just had PT (2). Finally, another investigation that reviewed many studies on the topic also found that surgery was no better than PT (4).
Hence, the answer is that the results of spinal stenosis aren’t impressive. In fact, over the long run, they’re no better than either no surgery or physical therapy. So why again are we performing these surgeries on patients?
How Dangerous is Spinal Stenosis Surgery?
One of the reasons why patients would want to avoid spinal stenosis surgery would be the complications. To take a deeper dive there we first need to understand that some of what spine surgeons report in research studies on complications is often different than what patients report as a complication, meaning surgeons can underestimate complications (3). In an analysis that looked at five large studies, the complication rate of surgery as reported by surgeons for spinal stenosis surgery is 10-24% (4). That’s 1 in 10 to 1 in 4 patients operated! Those include infection, nerve damage, increased pain, the need for more surgery, and other problems.
How Long is the Recovery After Spinal Stenosis Surgery?
Expect to be “down” for several days after the procedure. Most patients take narcotic medications for one to several weeks. However, if a fusion is added to the surgery, most patients will be on narcotics for about two months after the procedure (7). Short walks in a brace can likely happen for most people after the first week or two. However, don’t expect to back to full activities for 6 months. For patients with surgical success, most patients feel that they’re back to 100% by one year.
Can You Avoid Spinal Stenosis Surgery?
There are a few ways to avoid spinal stenosis surgery, some more invasive than others. One option is called a Coflex device, which is a metal spacer that is implanted in between the spinous processes (8). This is often after surgical decompression. The main concept behind the device is that it preserves some motion, but implanting it can destroy the normal fascia, muscles, and ligaments in the area.
There are other treatments which are performed or implanted using just x-ray guidance without surgery. One type is the MILD procedure which cuts the ligamentum flavum (the swollen ligament that often places pressure on the spinal cord or nerves), which then retracts back like a cut rubber band (9). This does open up the area, but this also reduces the stability in the spine as this ligament helps to keep things stable. There are also newer implant-based solutions like interspinous spacers that can be inserted using fluoroscopy like the Superion device (10). The issues with this implanted contraption is that even though this is placed without surgery, the implant still nukes the original ligament architecture and then puts more pressure on the discs.
Is There a Way to Avoid Spinal Surgery Without Destroying the Stuff I Was Born With?
The Regenexx-DDD procedure is the only one out there that is able to maintain the normal anatomy, not implant any pieces of metal, and still, have patients report that they’re much better. How is that possible? We use precision injections of orthobiologics, which in this case is usually your own platelets and a multitude of things we can make from that source including advanced lysates and plasmas. We can also use your own stem cells if needed. To find out more about how that works, see my video below:
How well does this work? Take for example a 66-year-old nurse I just re-evaluated yesterday. She has severe central canal stenosis in her low back and could only stand for about 15 minutes before we started. Now after three injection-based treatments using both fluoroscopy and ultrasound guidance, all of which only gave her soreness for a few days while she went about her usual activities, she’s now back to standing for more than an hour and is planning a trip to England next month where she intends to walk for miles.
What Activities Should Be Avoided with Spinal Stenosis?
Realize that the biggest problem with spinal stenosis is extension. This causes the swollen ligament in the back of the spinal canal (ligamentum flavum) to push against the nerves or spinal cord and then this is what generates symptoms. Hence, activities in flexion usually work better. meaning before you get the problem fixed, bike riding is a better activity than running, because this keeps you in that flexed position.
Is Walking Bad for Spinal Stenosis?
It’s not that there’s anything bad about walking, but that being upright while walking can set off symptoms by forcing the swollen ligament into the nerves which can then reduce the power in the legs for most patients. So until you get the problem fixed (hopefully without surgery), if you want to get exercise through walking, use a rolling walker so you can stay in slight flexion.
The upshot? Surgery isn’t all it’s cracked up to be for spinal stenosis. In fact, it’s laden with side effects and not any better than physical therapy. So do yourself a favor and try to avoid it!
___________________________________________
References:
(1) Lurie JD, Tosteson TD, Tosteson A, et al. Long-term outcomes of lumbar spinal stenosis: eight-year results of the Spine Patient Outcomes Research Trial (SPORT). Spine (Phila Pa 1976). 2015;40(2):63–76. doi:10.1097/BRS.0000000000000731
(2) Delitto A, Piva SR, Moore CG, Fritz JM, Wisniewski SR, Josbeno DA, et al. Surgery Versus Nonsurgical Treatment of Lumbar Spinal Stenosis: A Randomized Trial. Ann Intern Med. 2015;162:465–473. doi: 10.7326/M14-1420
(3) Ratliff JK, Lebude B, Albert T, Anene-Maidoh T, Anderson G, Dagostino P, Maltenfort M, Hilibrand A, Sharan A, Vaccaro AR. Complications in spinal surgery: comparative survey of spine surgeons and patients who underwent spinal surgery. J Neurosurg Spine. 2009 Jun;10(6):578-84. doi: 10.3171/2009.2.SPINE0935.
(4) Zaina F, Tomkins-Lane C, Carragee E, Negrini S. Surgical versus non-surgical treatment for lumbar spinal stenosis. Cochrane Database Syst Rev. 2016;2016(1):CD010264. Published 2016 Jan 29. doi:10.1002/14651858.CD010264.pub2
(5) Epstein NE, Hollingsworth RD. Nursing Review Section of Surgical Neurology International Part 2: Lumbar Spinal Stenosis. Surg Neurol Int. 2017;8:139. Published 2017 Jul 7. doi:10.4103/sni.sni_150_17
(6) Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ. 2016 Jan 4;352:h6234. doi: 10.1136/bmj.h6234.
(7) Vail D, Azad TD, O’Connell C, Han SS, Veeravagu A, Ratliff JK. Postoperative Opioid Use, Complications, and Costs in Surgical Management of Lumbar Spondylolisthesis. Spine (Phila Pa 1976). 2018;43(15):1080–1088. doi:10.1097/BRS.0000000000002509
(8) Li D, Hai Y, Meng X, Yang J, Yin P. Topping-off surgery vs posterior lumbar interbody fusion for degenerative lumbar disease: a comparative study of clinical efficacy and adjacent segment degeneration. J Orthop Surg Res. 2019;14(1):197. Published 2019 Jun 28. doi:10.1186/s13018-019-1245-3
(9) Chen H, Kelling J. Mild procedure for lumbar decompression: a review. Pain Pract. 2013 Feb;13(2):146-53. doi: 10.1111/j.1533-2500.2012.00574.x.
(10) Nunley PD, Deer TR, Benyamin RM, Staats PS, Block JE. Interspinous process decompression is associated with a reduction in opioid analgesia in patients with lumbar spinal stenosis. J Pain Res. 2018;11:2943–2948. Published 2018 Nov 20. doi:10.2147/JPR.S182322

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
