Can Your Neck Cause Hip Pain?
On this page:
“How often have I said to you that when you have eliminated the impossible, whatever remains, however improbable, must be the truth?” —Sherlock Holmes
You would think it would be quite easy to find the source of someone’s pain. After all, can’t you just look at an MRI and conclude that whatever is abnormal is the causing pain? While many physicians do it that way, regrettably, research studies have concluded that this is a surefire way to misdiagnose a patient.
Case in point is, “Can your neck cause hip pain?” Surprisingly, Yes…
Finding the Cause of Hip Pain
When looking for the source of pain, most of my medical colleagues only look as far as the “bright shiny object.” We all do this to some extent, focus on what seems to be the most obvious answer even when the truth turns out to be quite different.
In truth, finding the cause of someone’s pain can sometimes be hard. Why? Study after study continues to show that MRIs are notoriously bad at predicting which patients have pain based on an abnormal finding (1). This is true for just about every joint—MRIs that show severe problems often belong to patients with minimal pain, and images that look pretty normal often belong to patients in severe pain.
I guess the only saving grace is that there are a few detective findings in MRIs that can be associated more frequently with pain. In addition, a good doctor knows how to piece together physical-exam findings, imaging, and history like a detective puts together clues.
How Your Neck and Hip Pain Are Related
As you may recall, I diagnosed myself with cervical stenosis two years ago after a bad episode with nerve pain. While I’ve always been a good pain detective who knows intellectually that the neck can cause far-flung areas to hurt, there’s nothing like experiencing it firsthand.
The outside of my hips began occasionally hurting about a year ago. The pain comes and goes and really isn’t dependent on activity. At first I thought this could be hip arthritis or tendinitis in my iliotibial band. However, while some of these areas were mildly point tender, I was unable to really convince myself that either diagnosis made sense.
In addition my hip X-rays were normal for my age. At one point I chalked it up to a new medication I was taking, so I stopped that, but eventually the hip pain returned.
One night my hips began hurting. I then noticed that when I changed my neck position by adjusting the pillow, the pain went away. I have since replicated this hundreds of times, so this is reproducible. How does this work?
Cervical Stenosis and Hip Pain
Rumruay/Shutterstock
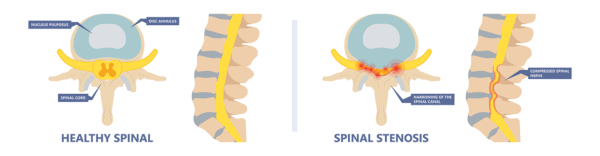
Cervical stenosis is when the hole for the spinal cord in the neck bones becomes too small due to wear-and-tear arthritis. The discs, facets, or joints called “uncovertebral” can place pressure on the cord (2). Since the job of the spinal cord is to carry signals to and from the body to the brain, placing pressure on the cord can result in a disruption of those signals.
It’s sometimes hard for patients to understand how pressure in the neck can make someone believe that a distant area is hurting (like the hips); however, a light-bulb-wiring analogy may help. If you mess with the wires that go to a light bulb at any point from the switch to the bulb, the bulb will go out.
From the perspective of the bulb, all it knows is that it’s not working. It’s ignorant to whether the issue is at the connection with the bulb, halfway there, or right after the switch. In the same way, pressure on the nerves at any point from the hip to the brain will be perceived by the brain as being in the hip.
The upshot? Can your neck cause hip pain? Yes. I now know this intuitively, which is a bit different from knowing it academically. My issue is managed well by using platelet lysate epidurals to keep the nerves and spinal cord in tip-top shape and avoiding certain positions I know cause my bone spurs to bump into my spinal cord. In the meantime, I lead a normal and very active life without surgery!
__________________________________________________
References
(1) Silvis ML, Mosher TJ, Smetana BS, et al. High prevalence of pelvic and hip magnetic resonance imaging findings in asymptomatic collegiate and professional hockey players. Am J Sports Med. 2011;39(4):715-721. doi:10.1177/0363546510388931

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
