Listening to the Body on Exam: An Old Car Crash Upper Back Injury Speaks…
One of the most famous physicians of all time is Sir William Osler, the father of the modern residency program that uses real-world clinical experiences to train young doctors. One of his most famous sayings was, “Listen to your patient; he is telling you the diagnosis.” I’ve heard that same mantra paraphrased through the years and morphed into, “If you listen to the patient, he’ll tell you the diagnosis; if you listen even longer, he’ll tell you how to treat it…” However, this “listening” doesn’t jive well with our fast-paced, see-20-plus-patients-a-day world of modern medicine. While we at our Colorado clinic book an hour of doctor face-to-face time with every new patient, there are some orthopedic clinics where the face time with the doctor is 5–15 minutes! This morning I’d like to both highlight a specific patient who had injuries from a head-on car crash as well as discuss what her body was telling me years later about her thoracic-spine and rib injuries and put that in the context of what Osler tried to teach doctors, but that has, for the most part, been lost.
Listening to Patients
I can remember many years ago when we had the standard insurance-based practice and we hired an “efficiency expert” that had been recommended to us by colleagues. This person came in and was appalled at the time we spent with patients. Her vision of the modern medical practice specializing in orthopedic injuries and pain was that the physician would see a patient every 15 minutes. To accomplish that feat, we would have to run multiple patient rooms at once, have a “scribe” who followed behind who would chart everything, extensively use physician extenders such as nurse practitioners and physician assistants, and basically see double the number of patients we were seeing. Thankfully, we realized, at that point, that while we would make much more money, the quality of care would go way down as there was just no way that in many patients you could do a good job in the factory-mill-type medical setting. Hence, we went the exact opposite direction: our 40-minute new-patient evaluations have moved to 60 minutes, and our 20-minute follow-ups have moved to 30.
Because of that format, which is very unusual in medicine, we try to listen to patients. Sometimes this takes the form of actual history, and sometimes it’s performing an extensive exam to see what the patient’s body is saying to us. The patient I’d like to highlight today verbally told me some important things, and her detailed exam confirmed what she said.
The Thoracic Spine and Rib Cage—the Undiscovered Country
If you see a physician who’s experienced in interventional spine or surgery and you have a neck or low-back condition, he or she will immediately dive in. However, tell that same physician that you have a thoracic (upper-back) or rib injury, and you’ll likely get a blank stare. As an example, while injections under X-ray or ultrasound guidance are commonly taught and performed for the neck and thoracic spine, from what I have seen, for every 100 neck injections performed, there are less than 1–5 thoracic injections performed, despite the prevalence of car crash upper back injury. Considering that the thoracic spine has just as many parts and pieces that can be injured as the neck and likely even more (since it attaches to the rib cage and sternum), this makes no common sense.
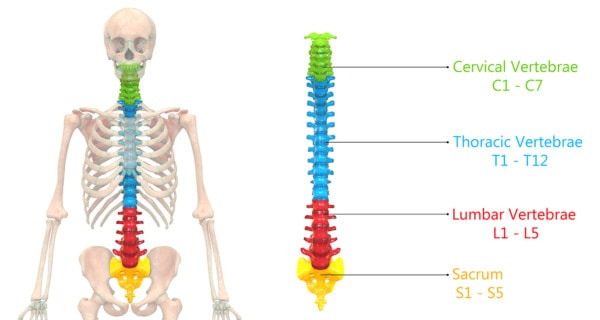
Magic Mine/Shutterstock
The thoracic spine is your upper back. It sits between the neck (cervical spine) and low back (lumbar spine) and is where your ribs attach. The ribs and thoracic spine are, therefore, heavily involved in breathing, turning the body to take pressure off the neck, and bending forward. The whole structure is less mobile than the neck and the low back. Injuries to this area are common, and the ones we most often see in clinic follow:
- Car crash upper back injury. Ribs and the thoracic spine commonly get injured in car crashes. In our experience, rear-end crashes can cause the area where the ribs attach to the spine to be injured. Frontal crashes can hurt the joints where the ribs attach to the sternum.
- Disc bulges and herniations that press on nerves, just like we see in the neck and low back. Way back when, we published a paper showing consistent thoracic-nerve problems on exam in patients involved in car crashes.
- Facet joint injuries or arthritis, like we see in the neck and back. These are the joints that connect the back part of the thoracic spine bones.
- Ligament and muscle sprains, tears, and injuries.
Listening to the Patient, and Exam of a Patient with a Car Crash Upper Back Injury
The patient mentioned above is a woman in her early 60s who was involved in a head-on car crash a few years ago. She had been treated with extensive physical therapy, facet injections and epidurals in her neck, and radiofrequency. She even had a little rib treatment in the lower right thoracic area with prolotherapy. Despite all of this, she still had tightness and pain that centered mostly around her bra line.
When I first examined her, I listened to her story. What I found interesting was that right after the crash, she had a big “bump” on her sternum due to the airbag deployment. If I followed this injured area back from her sternum along the connecting ribs, this was right where she had pain in her upper back near the bra line. In essence, she had told me what was wrong—the airbag damaged the joints where the ribs connect up front to the sternum and to the spine at her bra line. What was really fascinating was what her body was about to yell at me…
For her exam, I began with the same kind of pinwheel test described in the paper above. I took a device that has sharp pins in a wheel configuration and ran it up and down her upper back to see which levels she could feel or not feel well. Since the thoracic nerves supply the skin over or near where they exit the spine, this is the only way to see if those nerves are working or are compromised due to a disc bulge. However, as I watched her upper back, this is a picture of what I saw:
Notice that despite the fact that I rolled the pinwheel up and down her whole back, there are red marks right around the bra line (dashed gray circles). What’s going on? Her body is telling me the diagnosis…
The red is a histamine response in the skin. What is histamine? It’s a nerve transmitter that’s heavily involved in itching and the immune response. Surprisingly, we know that our nerves are made up of a small number of fibers that work hand in hand with histamine. Hence, it’s not surprising to me that the upper thoracic nerves are irritated in this patient and the small injury to the skin caused by the pinwheel is exaggerated here at this part of the upper back. This is suggested by another paper that shows how histamine is connected to irritated nerves. I see this redness as a great example of what Osler taught us—in this case “listening” to what the body is trying to tell us. Therefore, in this patient, my focus will be using regenerative-medicine injection techniques on the joints that connect these upper ribs to the sternum in the front and the ribs in the back.
The upshot? Osler taught us as physicians to listen and look. I think he would not be happy about our over reliance today on diagnostic tests that don’t often really explain the cause of the pain and our de-emphasis on exam and taking the time to listen. In this case, a bump on the sternum from an airbag and irritated nerves that tipped their hand by a little redness that might go unnoticed and solved the mystery of a car crash upper back injury undiagnosed for years.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.

