Disc Replacement Side Effects: New Research Is Concerning
The whole idea behind disc replacement is that it should have fewer side effects than fusing the spine. The artificial disc allows motion, which is, in theory, similar to a normal biologic disc. However, what if an artificial disc ended up distorting normal motion so badly that it still caused the disc above and below to fail, just like a fusion? A new study suggests that abnormal motion in these devices may be responsible for a whole new class of disc replacement side effects.
The Concept Behind an Artificial Disc
Rumruay/Shutterstock
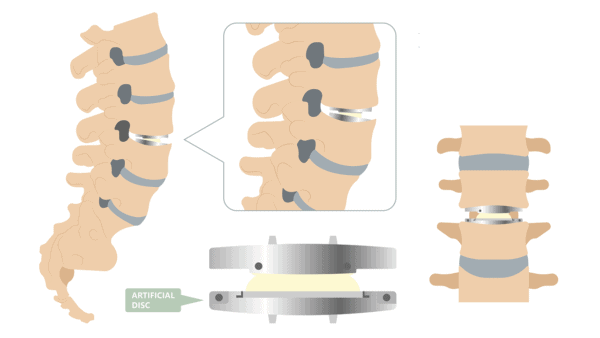
The concept behind disc replacement is to try to eliminate pain and retain movement in the spine by removing an injured disc and replacing it with an artificial (metal or plastic) one, about the size of a small hockey puck. This is in contrast to a fusion where the disc would be removed and the vertebrae fused together to stop movement in that part of the spine. While on the surface it sounds like a better option than a fusion, this is also a very big surgery that can lead to many problems, such as wear-and-tear ions (from metal- or plastic-device breakdown) in the blood, revision surgeries, ongoing pain, and now as the new study shows even adjacent segment disease (typically associated with fusions) due to abnormal motion in the spine.
Before we look at our feature study, let’s review some prior studies we’ve covered concerning disc replacement side effects.
Other Studies Looking at Disc Replacement Side Effects
We’ve known about metal ions in joint-replacement devices, such as knees and hips, for a long time, but a recent study also found significant metal ion concentrations in the blood of patients who’d had cervical disc replacements.
Another study found tissue reactions to wear particles that were just as severe following disc replacement as they were following hip or knee replacements. The most concerning issue was that inflammatory cells were found alongside the wear particles, and unlike in the hip or knee, the spinal nerves are very close here, so inflammation in this area will cause other symptoms.
While this one isn’t a study, it shows a disturbing issue: even young people, as young as teens, are being offered these surgeries despite the serious fusion and disc replacement side effects The young patient featured in the linked post was on the path to disc replacement surgery when her insurance, thankfully, rejected not only the disc replacement but also the aggressive fusion surgery. She was able to find relief through precise injections of her own growth factors.
What Is Adjacent Segment Disease?
To understand adjacent segment disease (ASD), you need to understand the structure of the spine. There are 24 movable vertebrae or back bones. These stack one of top of the other, and stretch from the neck all the way down to the lower back. Between each vertebra is a disc that provides a cushion, and the vertebrae meet in the back at facet joints at each disc level. All of this functions to protect the spinal cord, that big bundle of nerves that runs through our spinal column.
In a fusion, the hardware is installed along two or more vertebrae to permanently “lock,” or immobilize the fused vertebrae. ASD occurs when the fused section overloads the vertebrae above and below it, causing a breakdown in those neighboring unfused levels as well. In ASD bone spurs and arthritis develop, causing a significant amount of pain.
While we’ve know fusion leads to ASD, we’re now finding out that ASD may also be a disc replacement side effect. Let’s look at the new research.
The New Research
The purpose of the new study was to look at the configuration of the vertebral joints and disc in patients who’d had a total disc arthroplasty (TDA), or disc replacement. Researchers concluded, “Under axial rotation of the cervical spine, additional lateral and/or ventral/dorsal displacements are produced by TDA. Consequently, adjacent level disease (ALD) may be mechanically stimulated.” So while adjacent segment disease can be caused by the lack of movement created by fusion surgery locking the spine in place, this study shows it can also be caused by the abnormal motion in the spine that is created by a disc replacement.
The upshot? There is no free lunch in spine surgery. Meaning that all of it is causing damage at some level in an attempt to restore something. In most cases we see, the risks often outweigh the benefits, and in some cases the risk of damage due to surgery is reasonable. In the case of disc replacement side effects, abnormal motion created by these devices may get rid of the main argument for using them—that they don’t cause adjacent segment disease. In fact, the opposite may be true!

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
