Does PRP Work to Treat SI Joint Pain?

The addition of Orthobiologics to Interventional Pain Management changes the playing field, but only if you recognize that these substances allow for a different type of treatment paradigm. Today we’ll highlight a study that shows that issue and go over the evidence behind PRP and SI joint pain. Let’s dig in.
What Is the SI Joint?
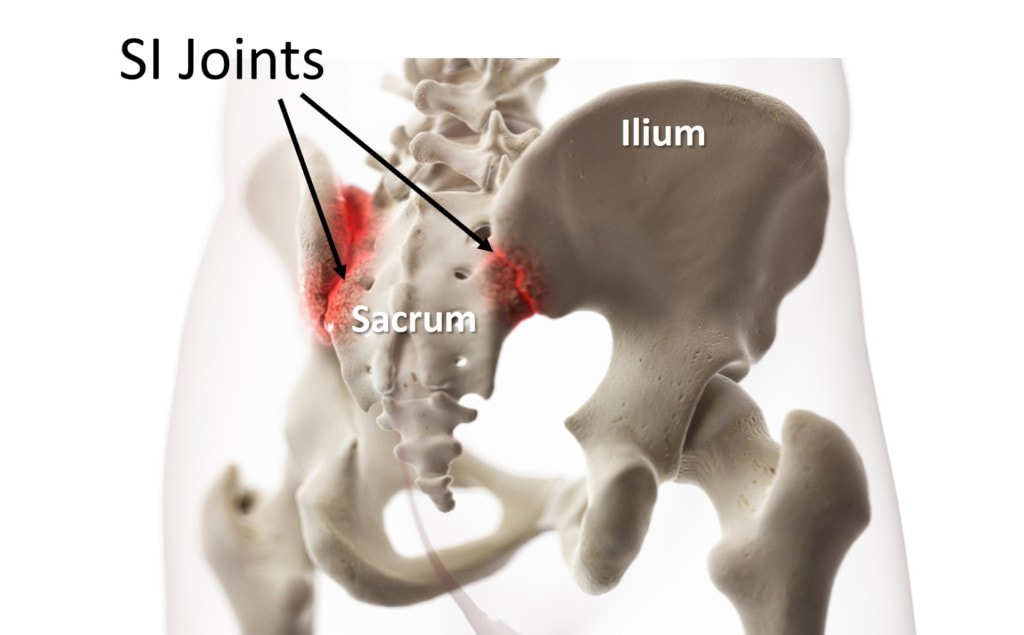
The SI joint (aka Sacroiliac joint) lives between the Sacrum and Ilium (tailbone and back of the pelvis). It’s a shock absorber, transferring force from your legs to your spine and vice versa. It can be injured in trauma such as a fall on the butt or through wear and tear. Also, pregnancy-related SI joint injuries during childbirth are also common as the baby’s head can only pass through the birth canal by stretching the SI ligaments.
That last bit about ligaments is critical:
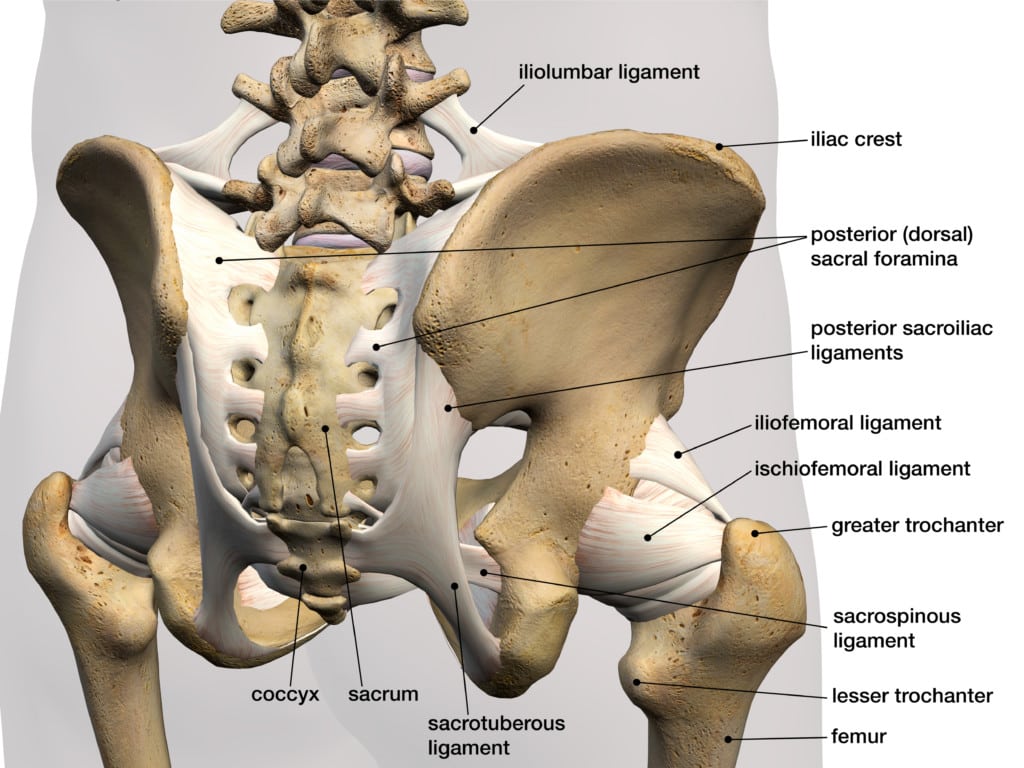
Notice how many ligaments surround this joint. In fact, it has ligaments on the inside of the joint and many on the outside located on the back/front. In addition, the ligaments create a kinetic chain with those that connect the SI joint to the rest of the spine above (Iliolumbar ligaments) and the rest of the pelvis below (Sacrotuberous and Sacrospinous ligaments). In fact, you could say that the joint is useless without these ligaments. Why? They define its force transfer function.
Pain vs. Loss of Function
I’ve spent quite a bit of time talking about how Interventional Orthobiologics (i.e. precise image-guided injection of Platelet-Rich Plasma) changes how physicians practice Interventional Pain Management (IPM). Why? First, let’s define IPM.
If you have low back pain due to Sciatica and you’re not yet a surgical candidate, more often than not these days you’re sent to a Physical Medicine or Anesthesia doctor who practices IPM. At that medical practice, you would often get an x-ray guided injection of high-dose steroids around the irritated nerve (epidural). If your low back pain is more diffuse and poorly understood, that doctor will be asked to perform diagnostic blocks. That means the precise x-ray guided numbing of specific structures to see if your pain goes away. That approach is called “finding the pain generator”.
However, there’s a real problem with that pain generator approach. It completely avoids the issue of the cause of the problem. The best way to explore why that’s a problem and how properly applied Interventional Orthobiologics avoids that pitfall is to use SI joint dysfunction as an example.
The SI Joint Dysfunction Example
The prevailing concept explaining the generation of chronic pain in the SI joint is instability (1). That means that the ligaments that hold the joint together have been damaged and aren’t doing their job. This causes extra wear and tear on the joint and pain. As a result, SI joint surgical Fusion is often recommended (2). That practice has now been expanded to include placing SI joint Fusion screws under x-ray guidance. While that’s a little less invasive, it still suffers from the same problems as SI fusion.
This is where the IPM approach to SI joint pain has a big problem. The approach is to inject a high-dose corticosteroid into the joint. While that’s a potent anti-inflammatory and can help pain over the order of a few weeks to months, it does nothing to address the cause of the problem, which is instability and loose ligaments.
In the Interventional Orthobiologics approach to SI joint pain, BOTH the joint and the ligaments are injected. For example, injecting the joint with PRP may help reduce inflammation in the joint, but injecting the ligaments can initiate repair and tightening of those structures leading to better stability in the long run and less pain generation.
The New SI Joint PRP Research
A new small study of 26 patients was just published comparing the injection of high-dose steroids in the joint versus PRP (3). This one found that the high-dose steroid worked better in the short-term (1 and 3 months) when compared to PRP. However, the study showed similar outcomes at 6 months and failed to follow these patients for any longer.
Now that you know why SI joint pain happens (instability), we can see a huge flaw in the study. It took the IPM approach (inject steroids into the joint) and simply substituted PRP for the steroid. It never attempted to use the PRP to treat the instability and ligaments.
There may well be other serious flaws with the research, but the full text of the publication is not yet out, so a more comprehensive critique will have to wait. What I can say is that 26 patients are usually not enough for an RCT with the effect sizes commonly seen in this sort of comparative study. Meaning every time we have run a power calculation for our own RCTs, about fifty patients (or more) is often the minimum study size. You can tell this was an issue here as the authors resorted to running a “responder analysis”. That’s when you try to determine if two groups with similar statistical means have one arm with more patients who reported positive responses. You never run this sort of secondary analysis if the differences between the groups are clear.
What Have Others Found?
A larger similar study using 40 patients and the same intra-articular technique also compared steroids to PRP to treat SI joint pain (4). They found the opposite. That PRP worked better at 6 weeks and 3 months when compared to a steroid. They also found that while steroids worked great early on, the effect didn’t last. Hence, this issue of steroid versus PRP to treat SI joint pain is far from settled.
IPM vs. Interventional Orthobiologics
I hope this blog has helped you understand that just switching out PRP for a steroid shot is likely not the right way to go when treating the spine. The advantage of Orthobiologics is that we can treat instability and the function of the spine by targeting ligaments. However, that’s just not part of the current IPM approach.
On the other hand, I also want to recognize a problem with studying a functional Orthobiologics approach that may have impacted the decision-making in this study. For example, we recently began to seek IRB approval for a PRP lumbar DDD study. The easy thing to do would be what they did here, which is to just substitute PRP for steroid and create two groups that way. However, while that’s the cleanest study design, that would cause the same problems. What we actually did was much harder. We defined how and when various structures should be treated with PRP and then compared that to a sham procedure. That requires the patient to be placed asleep with IV sedation while the doctor places needles in their back, but doesn’t inject. That study, even once completed, will likely be harder to get published as it’s trying to replicate what’s done in the everyday practice of Interventional Orthobiologics.
The upshot? In my clinical experience, chronic SI joint pain is easy to treat with Orthobiologics like PRP. However, I do have serious concerns that most IPM practitioners aren’t getting the memo about Orthobiologics changing what should be treated., This new study is a great example of how just switching out one injectate (steroid) with another (PRP) is likely hamstringing the Orthobiologic approach.
___________________________________
References:
(1) Hamidi-Ravari, B., Tafazoli, S., Chen, H. et al. Diagnosis and Current Treatments for Sacroiliac Joint Dysfunction: A Review. Curr Phys Med Rehabil Rep 2, 48–54 (2014). https://doi.org/10.1007/s40141-013-0037-7
(2) Lee DW, Patterson DG, Sayed D. Review of Current Evidence for Minimally Invasive Posterior Sacroiliac Joint Fusion. Int J Spine Surg. 2021;15(3):514-524. doi:10.14444/8073
(3) Chen AS, Solberg J, Smith C, Chi M, Lowder R, Christolias G, Singh JR. Intraarticular Platelet Rich Plasma vs Corticosteroid Injections for Sacroiliac Joint Pain-a Double Blinded, Randomized Clinical Trial. Pain Med. 2021 Nov 24:pnab332. doi: 10.1093/pm/pnab332. Epub ahead of print. PMID: 34850180.
(4) Singla V, Batra YK, Bharti N, Goni VG, Marwaha N. Steroid vs. Platelet-Rich Plasma in Ultrasound-Guided Sacroiliac Joint Injection for Chronic Low Back Pain. Pain Pract. 2017 Jul;17(6):782-791. doi: 10.1111/papr.12526. Epub 2016 Dec 1. PMID: 27677100.

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
