Hip Surgery Results: Little Evidence the Procedure Works
You would think that with the explosion of hip arthroscopy surgeries in the United States and worldwide that we would have excellent research supporting that the procedure is very successful for patients with hip impingement. You would, of course, be wrong. Despite the surgical melee, we don’t have a single high-quality study of excellent hip surgery results. The fact that a paper was just published describing a research study that is now being planned highlights this research void.
The Levels of Evidence for Surgical Procedures
First, I’m not a card-carrying and proselytizing member of the evidence-based-medicine mafia so prevalent in medicine today. In fact, being a clinical provider responsible for the day-to-day outcome of the patients I treat and taking that responsibility seriously, I’m more of an empiricist, which means that I have no issues with relying on observational evidence that a procedure works. Why?
Oftentimes, waiting for the highest levels of evidence before treating a patient is not ethical. For example, if you observe that a procedure works and the calculus is correct (i.e., low risk and the possibility of high return), then waiting a decade until the evidence catches up while the patient suffers is not right. Having said that, a key part of that equation is always risk (i.e., how likely is it that the procedure will cause a horrible side effect?).
This has always been my problem with many surgical procedures. Unlike precise injections, which are inherently low risk, orthopedic surgery is inherently higher risk. Infections, nerve injuries, and damage caused by the surgery are real issues. In addition, for many hip arthroscopy surgeries, you’re rearranging the structural anatomy, which carries with it bigger risks of creating a lifetime of abnormal function. Hence, in my book, orthopedic surgery has a higher evidence burden to bear than any injection-based procedure. Interestingly, the entire specialty has some of the weakest evidence base of any medical specialty with very few common procedures having any high-level evidence of efficacy. Hip arthroscopy is certainly in this club of higher-risk, low-evidence procedures.
What Is the Evidence That We Should Be Operating on Hip Impingement at All?
First, if this type of impingement or tear in the labrum was a common source of hip pain, we would expect that patients without hip pain wouldn’t have these findings and patients with hip pain would be the only patients who have them. Is this the case? No! In fact, many patients have these findings on hip MRI but have never experienced a day of hip pain.
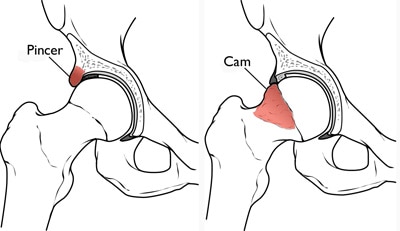
In addition, there’s another really disconcerting fact about these surgeries. One of the most common bone spurs that’s removed is called a “pincer” deformity. This means that the socket of the hip grows an extra piece of bone that usually extends to the side of the joint. Surgeons love removing this because early studies showed that the spur was associated with patients who had hip arthritis. However, these studies just said that the two things were related to each other, but they didn’t say how. Recently, the largest study done on this issue showed that the relationship was that the spur formed to protect the joint and that patients who had it developed less arthritis over time. So instead of causing arthritis, it protected against it! Hence, removing the spur is the opposite of what should be done based on the research.
The New Study
The new research will finally answer whether this invasive surgery is worth the risk. For example, this statement from the abstract says it all: “The current evidence to support both surgical and conservative interventions for femoroacetabular impingement is based on low-level research.” So for the first time, hip impingement patients will be randomized to get either surgery or physical therapy. Will this study show that the procedure actually works? Well, the recent history of testing common orthopedic surgeries versus physical therapy haven’t been helpful to surgeons. For example, a recent study showed that the most common orthopedic surgery in developed countries, surgery for meniscus tears, was no better than physical therapy.
The upshot? It’s great to see this invasive procedure finally get researched to show whether or not it works. Maybe it produces excellent hip surgery results; maybe it doesn’t. In the meantime, we usually prefer to use less-invasive stem cell injections rather than surgery.
To find out if you might be a candidate for a Regenexx stem cell procedure, complete our Regenexx Procedure Candidate Form online.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.

