How to Avoid ACL Surgery: Good Enough Is Great in This Case
Want to know how to avoid ACL surgery? Use the power of your own stem cells. Madeline, who is seen skiing hard above, skipped surgery for her complete ACL tear and instead had her own cells precisely and carefully injected into her torn ligament. That’s her tearing it just six months after her procedure. Huh? Is that possible?
What Is the ACL, and How Does It Work?
In order to teach you how to avoid ACL surgery, we have to start at the beginning. The ACL is a ligament that lives in the middle of the knee and that has two bundles that attach at different places. It prevents the forward motion of the tibia on the femur and also limits rotation of the tibia on the femur. From a practical perspective, this means that it provides front-back and twisting stability to the knee. In fact, it’s the two-bundle design that supplies the stability in the cutting and twisting movements of the joint.
What Is an ACL Reconstruction?
When the ACL ligament is torn, it’s generally accepted that it doesn’t heal well on it’s own. Hence, many times, patients undergo ACL reconstruction where the old ligament is taken out and a piece of tendon is strung between two points to act as a substitute for the ligament. It’s not perfect, as the two bundles are generally replaced with only one and the artificial ligament goes in at a much steeper angle than the original equipment. In addition, the lack of a double-bundle design means that the knee will always be more unstable in twisting or cutting movements.
What Are Some of the Problems with ACL Surgery That We Know About?
Most patients don’t realize that there can be quite a few problems with the surgically replaced ACLs. First, for example, with an autograft, the muscle the tendon graft is taken from never fully recovers its strength. Second, the operated knee never regains its normal position sense to guide normal landing. Finally, few patients ever return back to their prior levels of sports, and two-thirds of young ACL surgery patients will have arthritis by the time they’re 30. In addition, the new surgically installed ACL ligament has no ability to sense stretch, so the knee loses proprioception, or sense of position. As a result, we often recommend to our patients that they consider newer precise biologic injection options, like stem cells, before considering a surgical ACL replacement.
MW’s Knee ACL Journey
We pride ourselves in transparency when it comes to results. This means that we’re happy to talk about the patients that don’t respond at all or that respond partially. MW’s case is one of those where we didn’t get a perfect result, but the final outcome was pretty good for her purposes.
She tore her ACL in late summer and saw a surgeon who recommended an ACL reconstruction surgery. When I first saw her in the clinic, I wasn’t really sure we could help. One band of her ACL was torn in half and snapped back like a rubber band, and the other was hanging on by a thread. She also had an MCL injury that hadn’t been picked up and severe bone bruising with microfracturing of her tibia. She was also freaked out in general at the concept of an injection in her knee.
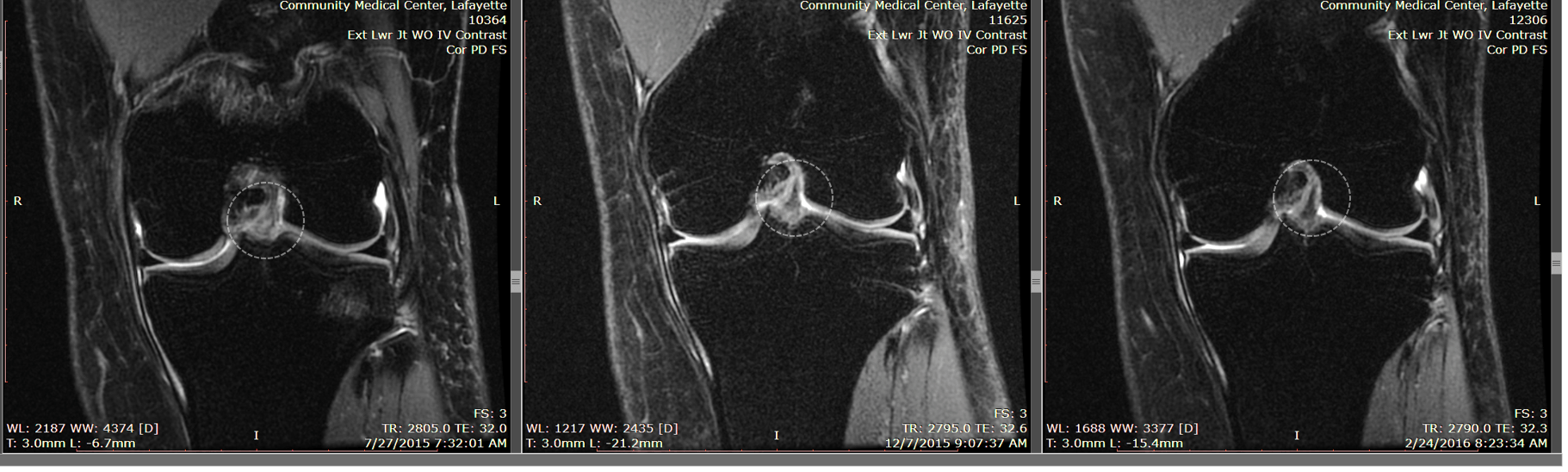
What did her MRIs show?
The pictures above show her ACL (in the gray dashed circles) before the injection, at three months after, and at six months after. What you’re seeing is a ligament that looks ghost-like on the first image and that looks more robust and darker by the third. More importantly, her knee on exam on this side is as stable as the other side.
While we appear to have complete healing on one of the main portions of the ACL, the other bundle (that was retracted back like a rubber band) never regenerated. Is that an issue? Based on her activity level and ability to do anything at this point, she doesn’t think so. In addition, this is about what she would have had if she had chosen surgery (single-bundle ACL), except that this one is her own ligament with full position sense and at a normal physiologic angle.
The upshot? Madeline dodged the surgery bullet by using advanced interventional orthopedics techniques and her own stem cells. No ripped out ligaments or a year or more to get back to full activity (which as you can see for her is ripping down a mountain with virgin snow at 60 mph on teleskis). She learned the easy way how to avoid ACL surgery, and we’re happy to see her back doing what she loves!

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.