How We Think about Treating Knee Arthritis with Stem cells
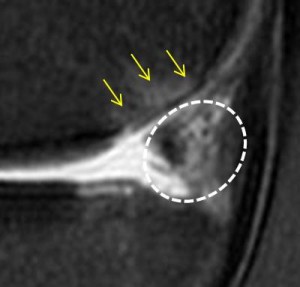
I examined a new knee patient this month who I thought would be helpful to illustrate how our clinic plans a patient’s knee treatment with stem cells. The patient is a middle aged Veterinarian who injured his right knee skiing 25 years ago and likely sustained a complete rupture of his ACL. He did well with it for many years, remaining very active, until recently in December he injured his right knee again while skiing. When the problems didn’t resolve on their own, he saw an orthopedic surgeon who performed debridement of a cartilage lesion and removed the better part of his torn medial meniscus (menisectomy-which can cause long-term problems with knee arthritis). While this helped a bit, he was unable to return to high level activity because every time he bent his knee (as with stair climbing, biking, or skiing), he had medial knee pain. In his particular case, his MRI tells the story (while in other patients it may not). His picture is above and shows a sagittal slice (sideways view). I’ve marked up a BML or bone marrow lesion, which is an area of swelling in the back of the medial femoral condyle. This is associated with cartilage loss, more of which was “debrided” (read removed) in his recent surgery. This post surgery MRI picture shows that this area is swollen. These BML’s have good correlation with pain, while many other types of MRI findings such as meniscus tears in middle aged patients, don’t have a good correlation with knee pain.
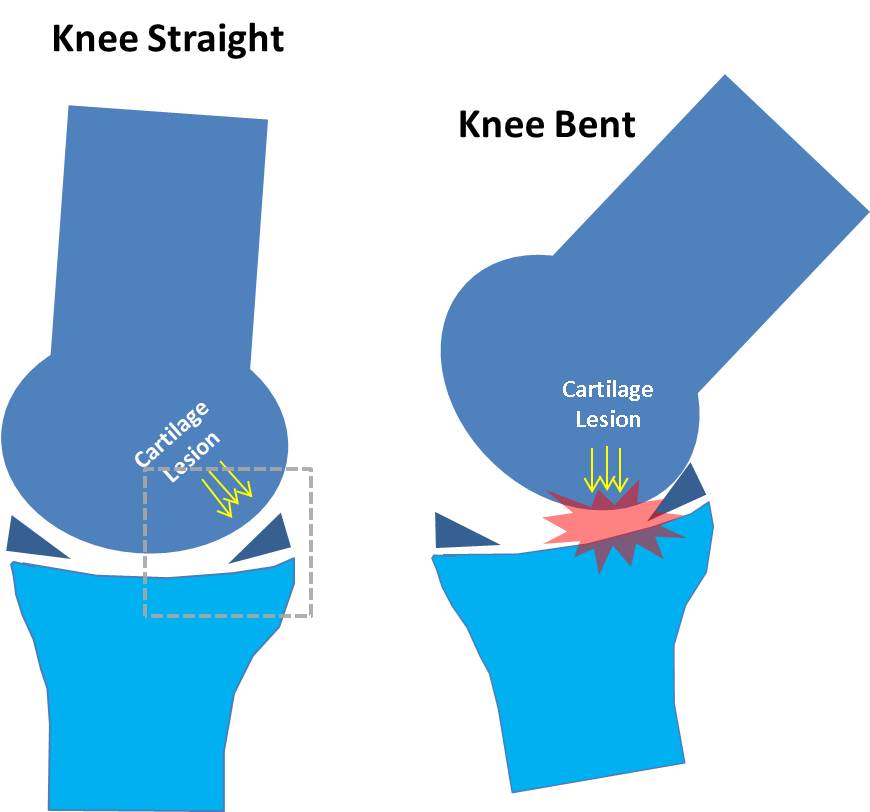
Why would this area in the back part of the femur bone be swollen? In the “knee straight” picture above, the cartilage lesion is protected by what’s left of his meniscus (the navy blue triangle). However, when he bends his knee (for instance with skiing), the cartilage lesion moves forward and becomes weight bearing. This new position causes more forces to be applied to this area. Why is all of this important? Where you place stem cells in knee has a big impact on whether the patient’s knee will respond and so in planning treating knee arthritis with stem cells it is crucial to determine where to place the stem cells for maximum benefit. Cells in this patient could be placed into his degenerative, remaining meniscus (dashed white circle) or into his cartilage lesion. In this case his MRI and some detective work identified the best place to put the stem cells is in the cartilage lesion. The upshot? Don’t settle for anything less than a sophisticated analysis of where your stem cells need to go within your knee. If someone wants to inject stem cells blindly in the joint and claims they will go where they are needed, that concept isn’t supported by the research.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.