Injection Treatment for EDS Patients
I still remember hearing about the time my niece dislocated her knee cap while cheerleading and had to go to the emergency room. Through the years of treating her, I got a crash course in injection treatment for EDS. Things can get pretty hopeless for these patients, hence I thought our shared experience was worth a blog post.
What Is EDS?
EDS stands for Ehlers-Danlos Syndrome. This syndrome represents a number of different diseases that all impact the connective tissue. The one we’re all likely most familiar with is the kid who can easily do the splits and becomes a gymnast because she’s hyper-flexible. In that case, the patient manufactures collagen that is more stretchy than usual. In addition, this is a spectrum disorder meaning that there are people who manufacture more or less of that stretch molecule (elastin) and hence are more or less hypermobile (able to move their joints too much).
There are many different EDS subtypes and here are a few:
- Hypermobile EDS (hEDS)
- Classical EDS (cEDS)
- Classical-like EDS (clEDS)
- Cardiac-valvular EDS (cvEDS)
- Vascular EDS (vEDS)
- Arthrochalasia EDS (aEDS)
- Dermatosparaxis EDS (dEDS)
- Kyphoscoliotic EDS (kEDS)
There are also many more. For example, the hypermobile type is one we all know, but there is also a type that also impacts the collagen in blood vessels (vEDS).
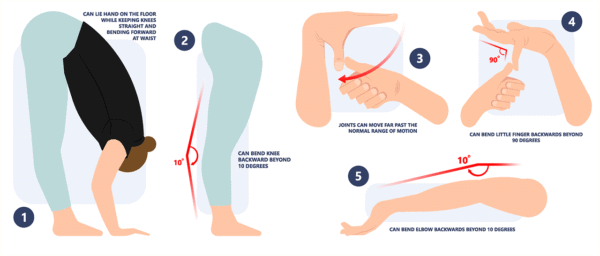
How Is EDS Diagnosed?
Rumruay/Shutterstock
These days genetic testing is often used, but the quick and dirty EDS assessment is called a Beighton score. This is a series of tests for hypermobility as shown above. Each move is scored and the points are added as discussed.
What Are the Symptoms of EDS?
This is where EDS becomes a difficult to recognize disease. EDS patients often present with painful areas due to instability. How does that work? The ligaments are designed to restrain and contain joint motion within only programmed movements. When the ligaments are damaged, they permit too much motion of the joint surfaces and the joints begin to move too much in the wrong directions. This leads to cumulative wear and tear damage on the joints, which can eventually lead to injury.
However, because EDS can cause all sorts of body areas to move too much, many other things can be impacted leading to a collection of difficult to interpret symptoms. For example, if the head moves too much on the neck (called Craniocervical Instability or CCI), the vagus nerve can become irritated leading to rapid heart rate or tachycardia. This can then lead to an expensive cardiology work-up for conditions like supraventricular tachycardia, when in fact, the cause is not something cardiology can diagnose (EDS).
Abandon Hope All Who Enter
EDS is called a zebra diagnosis. This refers to an axiom that we are all taught in medical school. The idea of a zebra is that rare diseases are rare, so physicians are taught not to spend too much time testing for rare things. Instead, it’s more common that doctors will encounter uncommon presentations of common diseases that look like rare diseases. What does that have to do with zebras? The expression is, “When you hear hoofbeats behind you, don’t expect to see a zebra.” In the case of EDS, this means that most EDS patients present with some collection of symptoms, commonly pain, and the doctor usually focuses on that painful area, often missing that there is a rare disease causing it all. So if an EDS patient presents with knee pain, the doctor will often misdiagnose this as knee arthritis because that is a more common disease.
Because of its zebra status, many EDS patients lose hope. I know this first hand through my niece. When she was in high school, I got a call that she was in the ER for a dislocated patella. All of that began a series of events that eventually lead to her almost complete disability while she was a graduate student at an elite university. Thankfully the university was great to her and we began a multi-year project of her flying out to Colorado to get periodic treatments.
Disability and EDS?
For most EDS patients, things begin to fall apart in their 20s which is when my niece’s issues shifted into high gear. Why? They’ve had EDS since they were born. They had it through puberty. However, by their 20s, all of the cumulative wear and tear is beginning to present as pain.
However, EDS patients are different than typical arthritis patients. Unlike most people who get arthritis due to wear and year which presents later in life, EDS patients are different at this age due to their regenerative abilities. What do I mean? The 50-year-old who gets arthritic pain due to lost cartilage and bone spurs has lost their natural ability to repair the dings and normal trauma that happens every day. Meaning wear and tear exceeds a waning repair response. However, a 20 something has immense natural regenerative abilities, so for EDS patients, there is serious wear and tear happening due to the hypermobility, but they also have a stout self-repair response. So for young EDS patients, wear and tear exceeds a young repair response. This seemly subtle difference is significant. Why? The 50-year-old’s joints will begin to degenerate and lose cartilage, while the young EDS patient’s joints will mostly not show rapid degeneration because of that young repair response.
EDS Treatment
My niece’s treatment began simply enough, with prolotherapy injections of problem areas. These are injections to cause a brief inflammatory response and thickening of the ligaments. The goal was to create mature scar tissue that had a different collagen mix than the stretchy type. If that didn’t happen, then at least cause thicker stretchy ligaments to form to reduce the instability. This worked well with demonstrable reductions in instability. We then advanced to platelet-rich plasma which didn’t work as well for her. Finally, we settled on using bone marrow concentrate, which worked the best of the three. This was a process whereby we isolated the stem cell fraction of her bone marrow and then reinjected that into various ligaments using x-ray or ultrasound guidance.
We ended up treating ligaments like the patellar retinaculum (ligaments that hold the knee cap in place), other knee ligaments, ankle, shoulder, SI joints, and neck. Our routine became using prolotherapy as the base treatment in many spots and reserving the bone marrow concentrate for the more severe areas.
This ligament rehabilitation and transformation program took a few years to accomplish as she was always at least one or two plane rides away and in college and then graduate school. Hence, I could see her a maximum of once or twice a year. However, I’m happy to report that now she’s no longer disabled and is now traveling with her new husband all over Europe (pre-COVID).
My Neice’s Point of View
She sent this after she read the blog:
“I love the blog!
You gave me a normal life back. There aren’t words to express how thankful I am.
There were times it looked like there was little hope and I didn’t know what my future would hold, but we got there.
- We were just talking last night about how much I’ve improved. It’s traveling to Europe and Africa, but it’s also all the small things that most people take for granted (but that I don’t). To me, a normal life means that I can now
walk all over the city, our max has been 20 km in a day - cook for us
- cuddle
- clean our apartment, organize our wardrobe
- work 8+ hrs a day, a lot more if necessary (standing desk)
- walk 10 flights of stairs up to our apartment
- not have to think about EDS when I’m getting dressed in the morning – I can get shirts over my head, wear normal/cute shoes
- Even my neck has been improving – I can turn my head a bit, look up a bit, with fewer symptoms.”
The upshot? EDS that causes pain and disability can be treated. I now have about 1 in 5 patients I see that lives somewhere along the EDS spectrum. The trick is using inexpensive treatments to tighten many different areas and saving the expensive stuff (bone marrow concentrate) for the bad spots. So if you have EDS, don’t lose hope. A more normal life is out there!

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
