Is Adding HA to PRP for Knee OA Worth the Cost?
One of my jobs at Regenexx is ensuring that our corporate partners spend insurance money wisely on orthobiologics. Basically, the money they’re spending is helping patients avoid more expensive procedures. One of the more popular add-ons to PRP is hyaluronic acid (HA). Is this worth the additional cost? If it makes PRP better, how much better?
HA and PRP
What is hyaluronic acid? Basically, it’s a component of normal synovial fluid that helps lubricate the knee. Doctors have used HA injections since the late 90s to help knee arthritis patients.
PRP is platelet-rich plasma created by concentrating blood platelets in plasma. There is strong evidence for its efficacy in treating knee arthritis, and now, there is evidence that it could be the world’s first DMOAD. That means that it may slow the progression of arthritis.
Because of the evidence that each of these treatments can be effective, some physicians have tested whether adding them together in the same injection session may better treat knee arthritis than either alone. Hence, several randomized controlled trials have been initiated, showing good efficacy for this combo. The big question I want to answer is, what is the magnitude of the effect you get from adding HA to PRP? Is that worth the added cost of the HA? Let’s dive in.
The Research Review
I counted 20 RCTs that involved HA and PRP. Some of these compare HA to PRP, showing that PRP is superior or non-inferior to HA for treating knee arthritis. Based on a systematic review and meta-analysis by Zhang, there are 9 RCTs on whether adding HA to PRP improves the outcome of treating knee arthritis (2). Four of these studies have follow-up periods of at least 12 months (3-6).
The Ke study is in Chinese, and I cannot get the full text (3).
The Yu study compared four knee OA groups: one with PRP alone, one with HA alone, one with PRP+HA, and a placebo (4). The study concluded that PRP was better than HA, and PRP+HA was better than either alone. Uniquely, not only did the study look at functional scores but also the plasma concentrations of various OA metabolites and inflammatory markers, finding the same order of efficacy in those measures. Here are the total one-year WOMAC scores graphed:
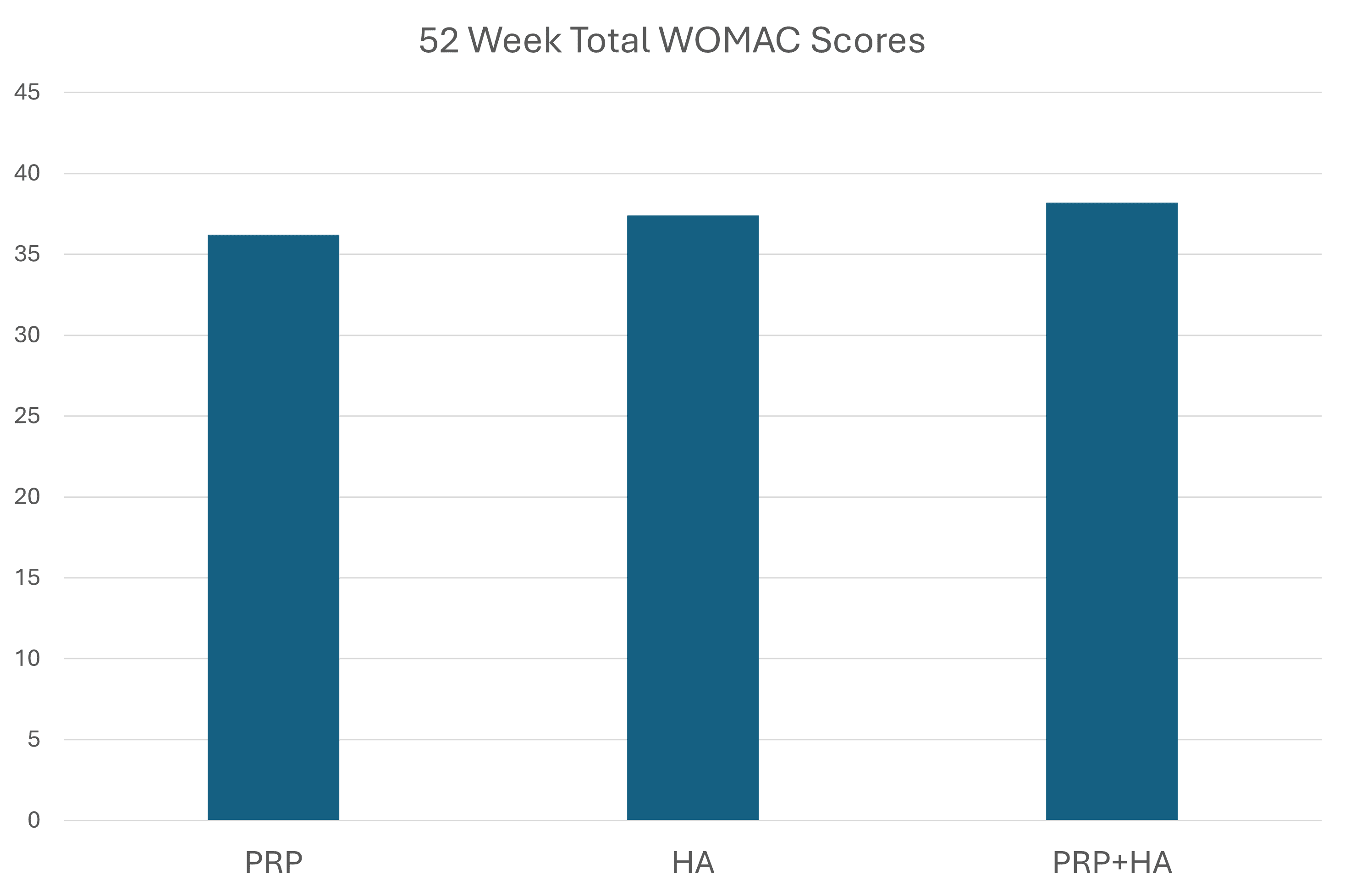
It should be noted that it was difficult to find out what concentration of PRP was used or even the blood draw and final volume for an estimate. As you can see above, these groups have minimal clinical differences.
The Lana study again showed that PRP beats HA, and PRP+HA was better at 1 and 3 months than PRP alone (5). However, it should be noted that this was a “fake PRP” study, with an 8-ml blood draw producing 5 ml of less than 2X PRP. Why was the concentration so low? This was a test tube gel PRP system (see my prior blog on that topic). Here are the WOMAC physical activity scores that look much better at 1 and 3 months but almost indistinguishable at six months and a year:
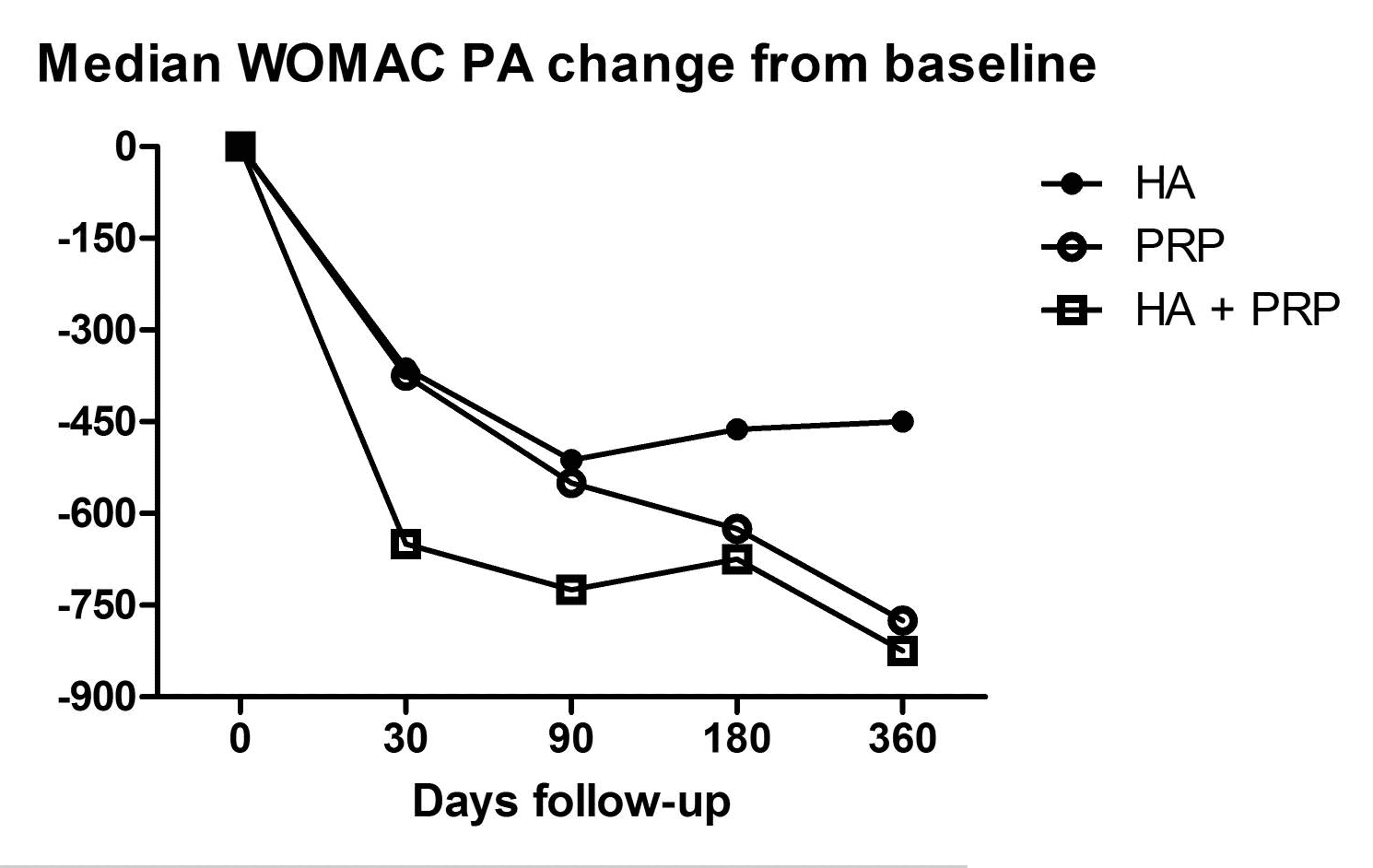
However, because this is a fake PRP study, it’s hard to know if the PRP would have worked much better had it been over 2X in concentration.
Finally, we have the Xu study, which used real PRP with about 5X concentration (6). Here are WOMAC index scores for this study:
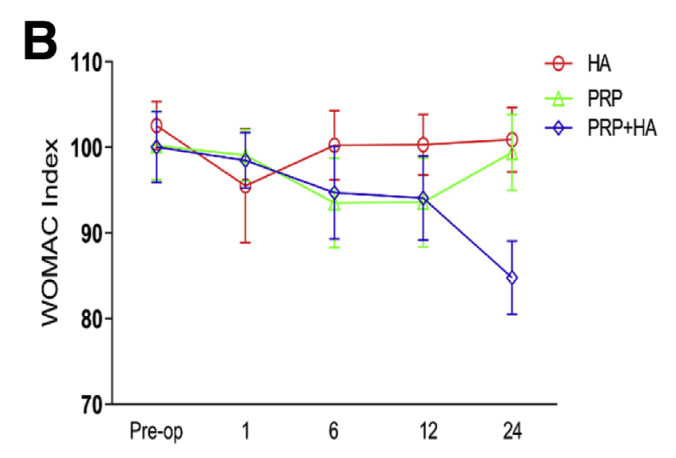
The PRP group does as well as the PRP+HA group up through 12 months, and then the PRP+HA group does better at 24 months. This looked a little fishy because that’s a BIG difference, so I dove in deeper. These were all moderate knee OA patients at KL 2 and 3. There were about 20% more KL 3 patients in the PRP group than in the PRP+HA group. The mean ages of the groups were similar. At 12 months, the synovial membrane thickness was better in the PRP+HA group.
Summarizing This Data
We have four studies that compare PRP vs. PRP+HA. Of the three that can be analyzed, only two allow us to estimate or determine the concentration of PRP injected. The Yu study, where this data is unavailable, shows little difference between the functional scores of these two groups. The Yu study also doesn’t have data on the severity of the OA being treated.
The Lana study, IMHO, should be disqualified outright as it doesn’t use real PRP, but I have included the functional scores for comparison. It should be noted that Lana also included a significant number of patients with mild KL1 OA.
Finally, we have the Xu study of moderate OA patients, which shows a significant difference in function at two years for the PRP+HA patients. While there is a slight difference in more severe OA patients in the PRP-only group, everything else seems to check out in this study.
Is Adding HA to PRP Worth It?
All we have to go on is one RCT, but so far, I would say yes. HA is relatively cheap these days, and until we have more studies that refute the results seen by Xu et al., I would say that the differences between the groups at two years warrant adding in a cheap additive like HA. Now, realize this is a soft recommendation based on a single RCT that could be refuted tomorrow by another well-done study that doesn’t show the same thing.
The upshot? HA is a cheap additive to PRP that, based on the existing evidence, seems to help the long-term efficacy of treating knee OA. While all of that could change tomorrow if another high-quality study shows something else, given its low cost, it’s a reasonable educated bet to make that adding HA will likely save money in the long run.
____________________________________
References:
(1) Lana JF, Weglein A, Sampson SE, Vicente EF, Huber SC, Souza CV, Ambach MA, Vincent H, Urban-Paffaro A, Onodera CM, Annichino-Bizzacchi JM, Santana MH, Belangero WD. Randomized controlled trial comparing hyaluronic acid, platelet-rich plasma and the combination of both in the treatment of mild and moderate osteoarthritis of the knee. J Stem Cells Regen Med. 2016 Nov 29;12(2):69-78. doi: 10.46582/jsrm.1202011. PMID: 28096631; PMCID: PMC5227106. https://pubmed.ncbi.nlm.nih.gov/28096631/
(2) Zhang, Q., Liu, T., Gu, Y., Gao, Y., & Ni, J. (2022). Efficacy and safety of platelet-rich plasma combined with hyaluronic acid versus platelet-rich plasma alone for knee osteoarthritis: A systematic review and meta-analysis. Journal of Orthopaedic Surgery and Research, 17. https://doi.org/10.1186/s13018-022-03398-6
(3) Chen-Rong KE, Rui Z, Ji-Xin X. Clinical efficacy of autologous platelet-rich plasma combined with intra-articular hyaluronic acid injection for knee osteoarthritis. Chin J Gen Pract. 2016;14(11):1810–1812.
(4) Yu W, Xu P, Huang G, Liu L. Clinical therapy of hyaluronic acid combined with platelet-rich plasma for the treatment of knee osteoarthritis. Exp Ther Med. 2018;16(3):2119–2125.
(5) Lana JF, Weglein A, Sampson SE, Vicente EF, Huber SC, Souza CV, et al. Randomized controlled trial comparing hyaluronic acid, platelet-rich plasma and the combination of both in the treatment of mild and moderate osteoarthritis of the knee. J Stem Cells Regen Med. 2016;12(2):69–78.
(6) Xu Z, He Z, Shu L, Li X, Ma M, Ye C. Intra-articular platelet-rich plasma combined with hyaluronic acid injection for knee osteoarthritis is superior to platelet-rich plasma or hyaluronic acid alone in inhibiting inflammation and improving pain and function. Arthroscopy. 2021;37(3):903–915.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
