Is PRP Really as Good as MFat for Knee OA?
Credit: Shutterstock
Two recent studies were published that seemed to show that platelet-rich plasma was as good as a common adipose tissue treatment to treat knee arthritis. However, anytime a study produces a result that goes against what we see clinically, it’s worth digging a bit into how they did the study. Both of these have some glaring issues, so let’s dig in.
What is PRP?
PRP is platelet-rich plasma and is made from concentrating platelets in a centrifuge. There have been dozens of published RCTs that show that it helps knee arthritis patients.
What is MFat?
MFat stands for Microfragmented Fat which is created by using liposuction to harvest adipose tissue. That tissue is then processed and broken down into tiny chunks of fat. The most common trade name of the kit used to create MFat is Lipogems. As I have blogged before, this is quite different than adipose SVF, which is a stem cell procedure that digests away the collagen holding onto stem cells. In MFat, there aren’t many free stem cells. Having said that, this has become a popular treatment for knee arthritis and there is some literature supporting that it may work for that application.
RCT 1-Half a Study
The first randomized controlled trial on the use of MFat in knee arthritis that we’ll review comes out of the PMR Department at Ohio State (1). From reading the abstract you would think that it’s a definitive study when it concludes that MFat didn’t beat PRP for the treatment of knee arthritis. However, just reading the full text of the paper proves otherwise.
The KL Grade Problem
In our clinical experience, PRP does well in the treatment of mild to moderate knee arthritis, but once you get to moderate to severe arthritis, then cell-based treatments like BMC or MFat tend to produce more reliable positive effects. Hence, when a study states that PRP and MFat are the same, the first thing to look at is the arthritis severity of each of the groups. Just 60 seconds with the full study here was enough to find a big problem.
KL grading is a system that assigns a number to knee arthritis from 0-4, depending on the radiographic severity of the disease, with 1 being the least arthritis (0 being normal x-ray) and 4 being the worst. Hence, when we look at the results of this study, we should see an equal distribution of the KL numbers in each group. However, this is what we see:
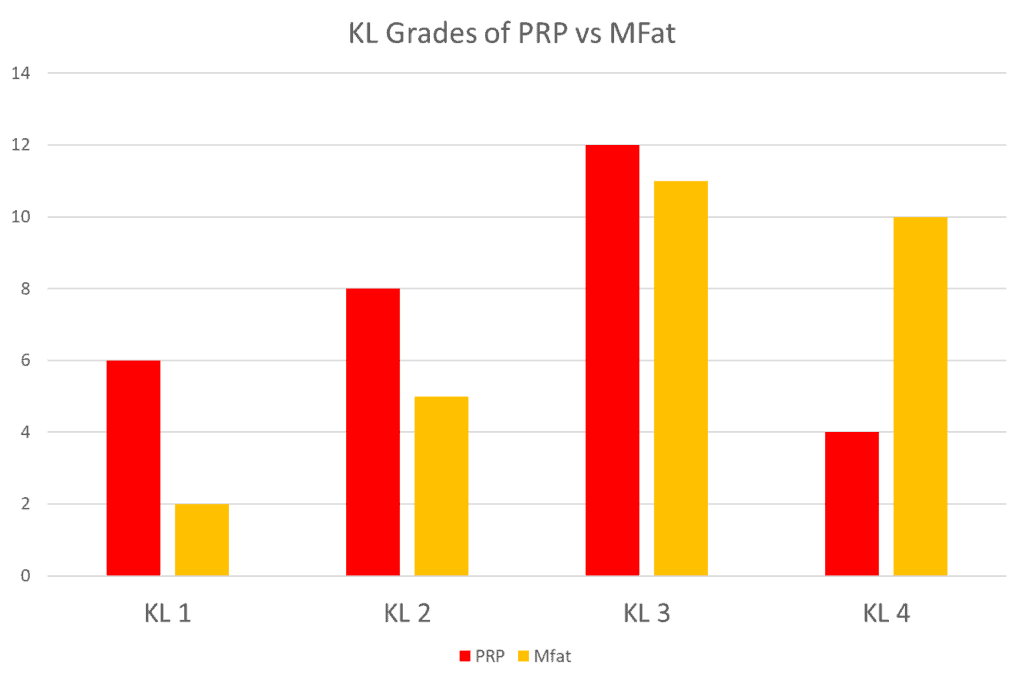
There are more patients with less severe KL grade 1 and 2 knee arthritis in the PRP group and more patients with more severe KL3 and KL4 knee arthritis in the MFat group. If we group those two categories, it looks like this:
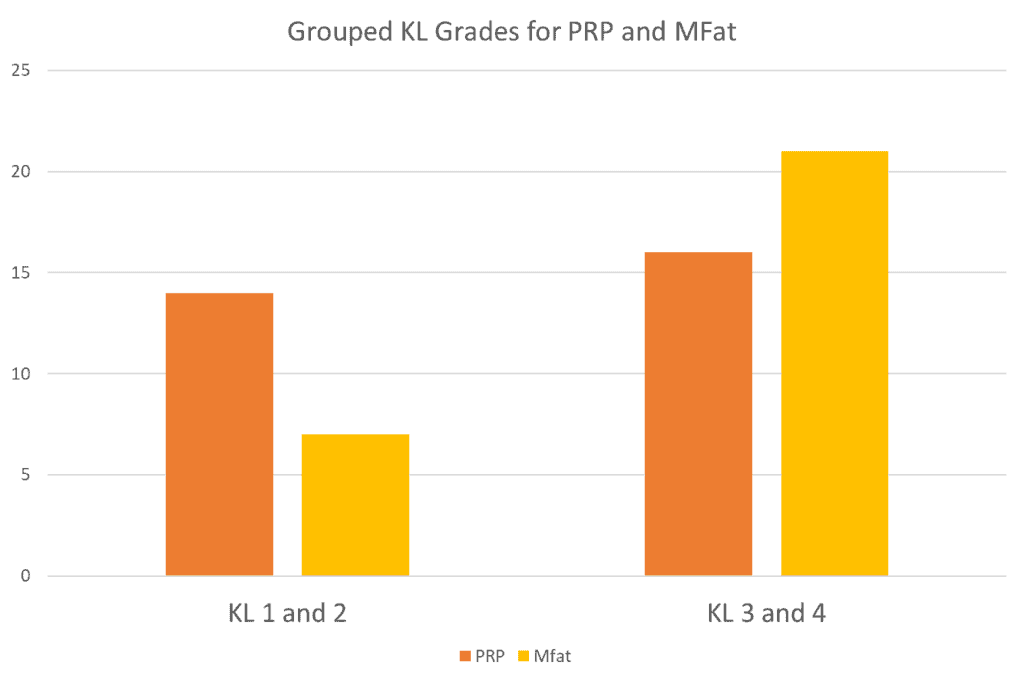
Hence, without looking too hard, this RCT wasn’t comparing apples in the PRP group to apples in the MFat group, but apples to oranges. Why might this severe imbalance of case severity have happened? The authors explain that in their discussion.
Half a Study
The authors of this study explain a serious problem in their discussion:
“This study has several limitations that warrant a discussion. The most important is that this study did not meet the power determined a priori to be sufficient to detect a difference between groups. This occurred because of evolving regulatory perspectives within our institution.”
So while the issue of asymmetric severity wasn’t discussed in the limitations section of the study, it was likely caused by the abrupt stop that was put on recruiting patients. The authors do discuss that this stop caused them to miss hitting study numbers that might have been able to show statistical differences between the groups.
The authors also discuss this limitation:
“Additionally, 6-month outcomes are relatively short-term.”
That’s right, the 6-month follow-up period used in this study is not standard. The standard follow-up period for these types of studies is 24 months or 2 years.
RCT 2-A Better Study?
There is a second RCT comparing these two technologies that was published by Gobbi et al and that fixes two of the issues in the Ohio State study (2). In the Gobbi study, they restrict the KL grades to 0-2 and follow up for two years. This study also includes 80 knees, so it hit its recruiting goals to get to a number of patients that should be able to show statistical significance between the groups. Gobbi et al compared multiple PRP injections with hyaluronic acid to MFat.
The study ultimately concluded that PRP and MFat were similar in outcome, but let’s dig into that data. We’ll review the results of several of the standardized questionnaires the authors used. First up is the IKDC:
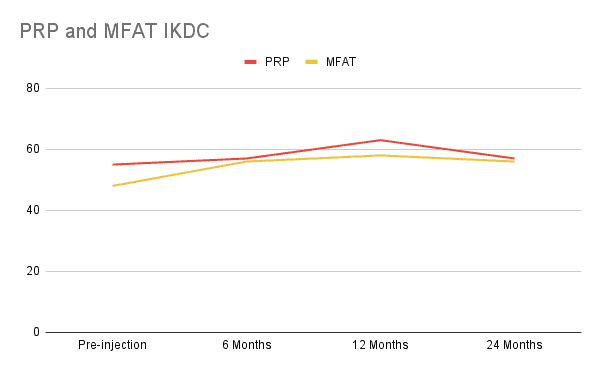
Here the PRP group began with a much higher level of disability with a score of 55 in the IKDC compared to a score of 48 for the MFat group. The improvement for IKDC over baseline gets as high as 8 points for the PRP group and 10 points for the MFat group. The MCID for the IKDC questionnaire, when used for surgeries like cartilage repair, is 9.8, so only MFat archives that degree of score improvement (3).
It’s critical to note that the MCID or Minimal Clinical Important Difference is defined as the score change that patients would find clinically meaningful. Our research group has looked at this closely and the problem is that it’s calculated specifically for each therapy/follow-up time point and no MCIDs exist for orthobiologic treatments like PRP or MFat. Hence, we’re using a score here that was calculated for a cartilage repair surgical procedure. In addition, there’s a questionnaire-based method that uses patient satisfaction and a statistical variance method for calculating MCID. So the best we can say here is that based on a cartilage repair MCID, the PRP underperformed the MFat on this specific IKDC questionnaire.
Next, let’s look at what happened with knee pain (VAS or Visual Analog Scale):
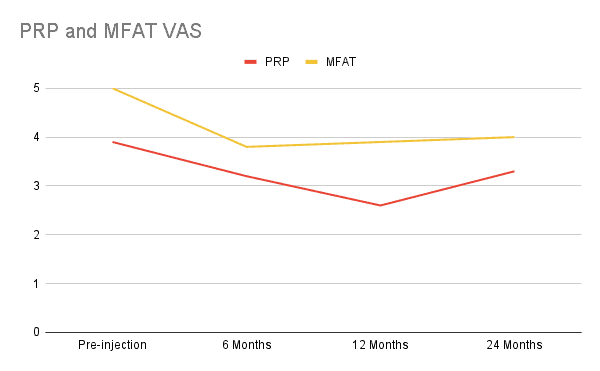
Here the MFat group begins with a higher pain score than the PRP group and seems to do a better job at maintaining the drop in pain which is an unimpressive 1-point drop. PRP has a similar but slightly more impressive 1+ point drop, but then the pain rebounds at 2 years.
Finally, let’s look at the KOOS questionnaire. Here the authors only reported the subscales, which will make this a bit harder to tease out because there 5 different scores to review. Many of these scores didn’t show statistically significant changes. Hence I picked the one that seemed to show the biggest dichotomy between the two procedures:
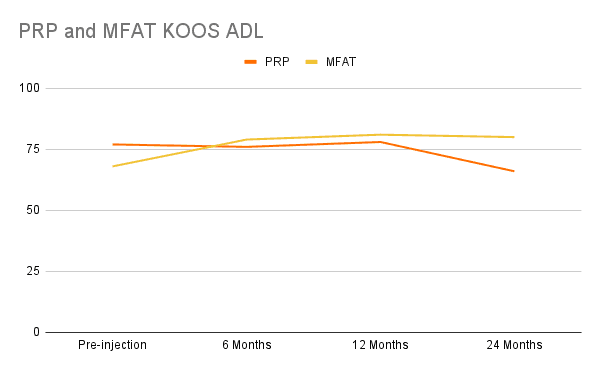
For the Activities of Daily Living (ADL) KOOS subscore, above we see that PRP doesn’t improve that score and shows a deterioration in function (score goes down) at one year, but MFat not only improves that score but the gains are also maintained. However, when looking at the MCID for a cartilage preservation surgery (not an orthobiologic injection), neither of these treatments met the 17-point improvement that represents the MCID (4).
Finally, let’s look at the KOOS Sports subscale as that shows some squirrely data that doesn’t fit with what we see clinically:
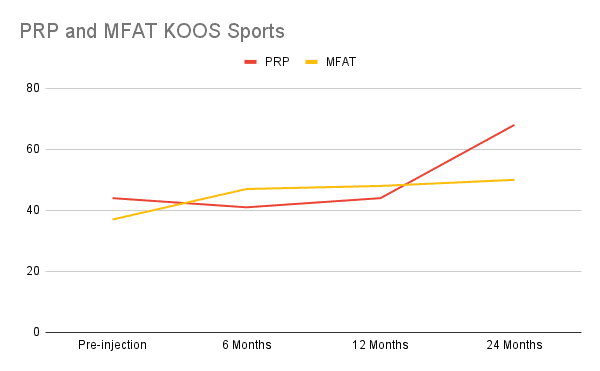
Here PRP actually makes patients a bit worse at 6 months and then the score returns back to baseline at 12 months only to rocket up big time at 24 months. Given that we have no mechanism for how that would occur nor is that something seen clinically or in other studies, this is likely an artifact and not a real effect of the treatment. The MFat data looks more solid, with improvement at 6 months which is maintained and improves slightly over time. Given that the PRP data looks like an artifact, applying the MCID here makes no sense.
Regrettably, the Gobbi study brings up more questions than answers. Neither treatment was an absolute homerun, but both seemed to improve pain and function. However, on the functional questionnaires, only MFat seems to have surpassed the MCID borrowed from another treatment.
Why the poor performance of PRP in this study when we have dozens of RCTs where it has performed very well against saline, steroid, and hyaluronic acid? This may be a clue from the paper:
“The system provides a 1.6-1.8 fold increase in platelets.”
Hence the platelet preparation method used didn’t meet the Marx minimal level of concentration to be classified as PRP (2x) (5). I’ve blogged on this topic of fake PRP before and the need to make sure that for older patients, we have PRP at least 10-20X concentrated. This is a real issue here, as the average age in this study was in the early 60s.
PRP vs MFat-Final Conclusions
We have two RCTs that have compared PRP and MFat. The first study was stopped in the middle and recruited more severe patients for the MFat group, so no conclusions can be drawn about the outcome. The second study produced results that kept going in and out of statistical significance and didn’t actually use PRP. Hence, despite lots of resources being expended on both studies, the jury is still out on this one.
The upshot? Does a PRP injection produce the same level of improvement as an MFat procedure? We still don’t know based on flaws in both of the RCTs we have, so maybe some research group will come out with a better study comparing the two.
_____________________________________________________
References:
(1) Baria M, Pedroza A, Kaeding C, Durgam S, Duerr R, Flanigan D, Borchers J, Magnussen R. Platelet-Rich Plasma Versus Microfragmented Adipose Tissue for Knee Osteoarthritis: A Randomized Controlled Trial. Orthop J Sports Med. 2022 Sep 16;10(9):23259671221120678. doi: 10.1177/23259671221120678. PMID: 36147791; PMCID: PMC9486262.
(2) Gobbi A, Dallo I, D’Ambrosi R. Autologous microfragmented adipose tissue and leukocyte-poor platelet-rich plasma combined with hyaluronic acid show comparable clinical outcomes for symptomatic early knee osteoarthritis over a two-year follow-up period: a prospective randomized clinical trial. Eur J Orthop Surg Traumatol. 2022 Aug 23. doi: 10.1007/s00590-022-03356-2. Epub ahead of print. PMID: 35997833.
(3) Ogura T, Ackermann J, Mestriner AB, Merkely G, Gomoll AH. The Minimal Clinically Important Difference and Substantial Clinical Benefit in the Patient-Reported Outcome Measures of Patients Undergoing Osteochondral Allograft Transplantation in the Knee. Cartilage. 2021 Jan;12(1):42-50. doi: 10.1177/1947603518812552. Epub 2018 Nov 22. PMID: 30463426; PMCID: PMC7755969.
(4) Jacquet C, Pioger C, Khakha R, Steltzlen C, Kley K, Pujol N, Ollivier M. Evaluation of the “Minimal Clinically Important Difference” (MCID) of the KOOS, KSS and SF-12 scores after open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2021 Mar;29(3):820-826. doi: 10.1007/s00167-020-06026-0. Epub 2020 Apr 27. PMID: 32342141.
(5) Marx RE. Platelet-rich plasma (PRP): what is PRP and what is not PRP? Implant Dent. 2001;10(4):225-8. doi: 10.1097/00008505-200110000-00002. PMID: 11813662.

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
