Is There Solid Research on Using PRP to Treat Spinal Pain?
Art: Credit Dall-E with the prompt: “A human spine in 3D surrounded by red blood cells in the style of impressionism.”
As you know, I often write about what I experience. This week an interventional spine physician questioned whether PRP would be useful in the treatment of lumbar radiculopathy or painful facet joints in the neck. Let’s review the RCT data that we have on this topic and the spine in general.
What Are We Talking About Here?
Platelet-rich plasma (PRP) is created by concentrating the platelets found in the blood. The idea is that these platelets assist healing by excreting both growth factors and specific exosomes. There are dozens of randomized controlled trials now that show that PRP is better than steroids, saline, and hyaluronic acid in helping problems like knee arthritis, epicondylitis, and carpal tunnel syndrome.
This blog will also discuss platelet lysate, which is created by stripping the platelets of their growth factors. Since platelets slowly degranulate their growth factors over 7-10 days, PL has more immediate growth factors available to the patient’s tissues (1). In addition, our in-vitro data shows that PL is more anti-inflammatory than PRP.
The Linkedin Comments
A Linkedin poster who is an interventional spine physician stated that he couldn’t figure out how PRP would work to treat lumbar radiculopathy as, in his mind, this is caused by compression. He also reported that, in his limited experience, injecting PRP into painful neck facet joints didn’t work. I responded that I would put together a blog summarizing what we know about using platelet injections to help spinal pain.
Why Would Platelet Products Help Nerves or the Cartilage in Facet Joints?
PRP has been shown to release various growth factors. One of those growth factors is NGF (Nerve Growth Factor), and it’s believed that through this growth factor as well as others like VEGF (which builds new blood vessels), PRP may be able to help nerves repair (2-6).
The cervical and lumbar facet joints have cartilage like a knee joint (10). The other growth factors in PRP, like TGF-b, also likely have a positive impact on cartilage repair (7-9).
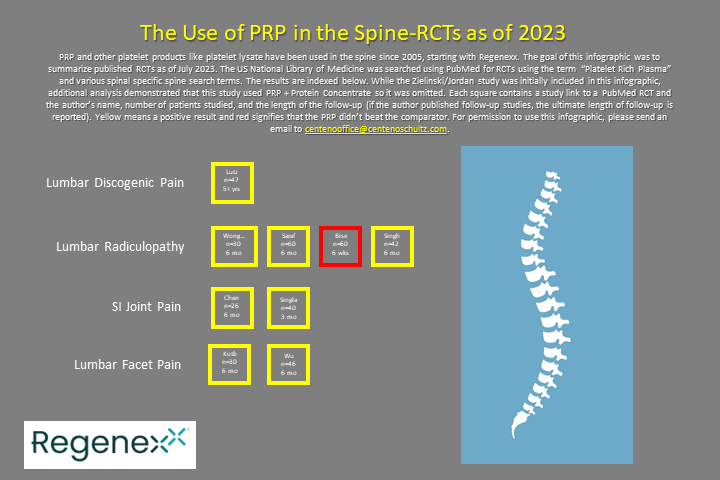
The Use of Platelets in the Spine: What Do We Know?
The infographic above summarizes the RCTs described below. Click on the image above to be taken to the PDF. Each square represents a study with a link to PubMed. A yellow square indicates that the study was positive (PRP was better than the comparison treatment). Each square has the author’s name, the number of patients, and the follow-up period. If you find studies I missed, please don’t hesitate to contact me at [email protected] so I can issue another version of the infographic.
Painful Discs
The intervertebral disc can get damaged and produce pain (17). The treatment options outside of physical therapy, chiropractic, and surgical fusion are limited.
Animal models show that PRP can reduce disc degeneration (16). One of the mechanisms behind this effect has been linked to platelets degranulating a specific type of exosome (14,15).
We have a solid randomized controlled trial (RCT) data that used a radiographic contrast-only control group with a very long-term follow-up that PRP can help painful low back discs (11-13). That result is quite different than a 2022 study that showed no results when compared to saline but only followed patients up for eight weeks (29). More importantly, this study used PRP + Protein Concentrate; hence it was ultimately excluded from this infographic.
Lumbar Radiculopathy
When a spinal nerve is irritated, this is called radiculopathy; the nerve can misfire, leading to numbness or tingling down a leg or weakness. There is also the possibility of compression of the nerve.
What clinical data do we have that platelets can help? We published a large case series of epidural platelet lysate for the treatment of radiculopathy, and a much smaller case series was published on epidural PRP (18, 20). One recent RCT compared epidural PRP versus steroid injection in patients with a herniated disc, and PRP beat the traditional treatment (19). Another PRP RCT showed that PRP beat steroids in patients with lumbar radiculopathy when the outcomes at six months were reported (21). This result was mirrored in a second similar study that found that epidural PRP results lasted longer than corticosteroids (23). Finally, this result is consistent with another RCT, which used CT-guided interlaminar epidurals in radiculopathy patients and showed that in the short run (6 weeks), the PRP was equivalent to steroid (22).
SI Joint Pain
The sacroiliac or SI joint can cause pain, with instability being a major cause (24). Steroid injections are often used in patients who fail physical therapy or manipulative care.
One recent study used ultrasound-guided PRP injections and concluded that they worked better in the mid-term (3 months) than steroids (26). A separate study showed that intra-articular PRP helps but is less effective than steroids (25).
Facet Pain
There are joints in your spine at each level. These joints can get injured or damaged like any other joint with cartilage. Facet pain that is resistant to conservative care is often treated with either a steroid injection or radiofrequency ablation.
A recent RCT compared PRP to steroids for reducing lumbar facet pain and the signs of synovitis on lumbar MRI and showed the PRP to be superior (27). Yet another similar study looking only at pain/functional outcomes concluded that the PRP had longer-lasting effects (28).
My Analysis
I have been using PRP and platelet lysate in the spine since 2005, which would make me the first physician to use PRP in that way. We have observed excellent results in helping patients avoid spinal surgery since then and, as of this month, are tracking 12,964 lumbar and 4,655 cervical orthobiologic procedures. Despite knowing the excellent results represented by that registry data, I’m blown away by the proliferation of high-quality data present on the use of platelet products on multiple indications in the spine.
The Right Way to Use Platelets in the Spine Versus Using Them Like Steroids
Another problem we have in using PRP or PL in the spine is the conceptualization by interventional spine physicians that they should utilize orthobiologics in the same way they used to inject steroids. For example, merely switching out the steroid in the syringe for PRP. Or combining traditional interventional approaches to the spine with PRP. On that note, our physician above seems to have performed RFA to destabilize the neck muscles and then injected PRP into the denervated joints. That approach makes no common sense.
The advantage of using orthobiologics in the spine is the ability to treat the entire functional spinal unit. For example, degenerative instability is common in patients with facet pain. While the research above shows that you can get a certain result by injecting only the joint with PRP, you can likely do far better by injecting the lax ligaments causing the instability and beating up the facet joints. That also means that procedures like RFA that destroy the normal stabilization system of the neck would be antithetical to the use of orthobiologics.
The upshot? It’s great to see the explosion of RCTs on PRP use in the spine these past few years. These results, in general, support what I have been observing since 2005. In other words, I have little doubt that PRP will eventually become a mainstay treatment for the spine.
___________________________________________________
(1) Martineau I, Lacoste E, Gagnon G. Effects of calcium and thrombin on growth factor release from platelet concentrates: kinetics and regulation of endothelial cell proliferation. Biomaterials. 2004 Aug;25(18):4489-502. doi: 10.1016/j.biomaterials.2003.11.013. PMID: 15046940.
(2) Monje PV, Rendon S, Athauda G, Bates M, Wood PM, Bunge MB. Non-antagonistic relationship between mitogenic factors and cAMP in adult Schwann cell re-differentiation. Glia. 2009 Jul;57(9):947-61. doi: 10.1002/glia.20819. PMID: 19053056; PMCID: PMC2829776.
(3) Oudega M, Xu XM, Guénard V, Kleitman N, Bunge MB. A combination of insulin-like growth factor-I and platelet-derived growth factor enhances myelination but diminishes axonal regeneration into Schwann cell grafts in the adult rat spinal cord. Glia. 1997 Mar;19(3):247-58. doi: 10.1002/(sici)1098-1136(199703)19:3<247::aid-glia7>3.0.co;2-w. PMID: 9063731.
(4) Höke A, Sun HS, Gordon T, Zochodne DW. Do denervated peripheral nerve trunks become ischemic? The impact of chronic denervation on vasa nervorum. Exp Neurol. 2001 Dec;172(2):398-406. doi: 10.1006/exnr.2001.7808. PMID: 11716563.
(5) Kuffler DP, Reyes O, Sosa IJ, Santiago-Figueroa J. Neurological recovery across a 12-cm-long ulnar nerve gap repaired 3.25 years post trauma: case report. Neurosurgery. 2011 Dec;69(6):E1321-6. doi: 10.1227/NEU.0b013e31822a9fd2. PMID: 21712738.
(6) Zhu Y, Jin Z, Wang J, Chen S, Hu Y, Ren L, Wang Y, Song Q, Tian X, Xie F, Peng J, Peng N, Luo Y, Wang Y. Ultrasound-guided platelet-rich plasma injection and multimodality ultrasound examination of peripheral nerve crush injury. NPJ Regen Med. 2020 Nov 20;5(1):21. doi: 10.1038/s41536-020-00101-3. PMID: 33298932; PMCID: PMC7680141.
(7) Fang, D, Jin, P, Huang, Q, Yang, Y, Zhao, J, Zheng, L. Platelet-rich plasma promotes the regeneration of cartilage engineered by mesenchymal stem cells and collagen hydrogel via the TGF-β/SMAD signaling pathway. J Cell Physiol. 2019; 234: 15627– 15637. https://doi.org/10.1002/jcp.28211
(8) Liang Y, Li J, Wang Y, et al. Platelet Rich Plasma in the Repair of Articular Cartilage Injury: A Narrative Review. CARTILAGE. 2022;13(3). doi:10.1177/19476035221118419
(9) Kennedy MI, Whitney K, Evans T, LaPrade RF. Platelet-Rich Plasma and Cartilage Repair. Curr Rev Musculoskelet Med. 2018 Dec;11(4):573-582. doi: 10.1007/s12178-018-9516-x. PMID: 30203333; PMCID: PMC6220001.
(10) Almeer G, Azzopardi C, Kho J, Gupta H, James SL, Botchu R. Anatomy and pathology of facet joint. J Orthop. 2020 Apr 8;22:109-117. doi: 10.1016/j.jor.2020.03.058. PMID: 32322140; PMCID: PMC7163055.
(11) Tuakli-Wosornu YA, Terry A, Boachie-Adjei K, Harrison JR, Gribbin CK, LaSalle EE, Nguyen JT, Solomon JL, Lutz GE. Lumbar Intradiskal Platelet-Rich Plasma (PRP) Injections: A Prospective, Double-Blind, Randomized Controlled Study. PM R. 2016 Jan;8(1):1-10; quiz 10. doi: 10.1016/j.pmrj.2015.08.010. Epub 2015 Aug 24. PMID: 26314234.
(12) Monfett M, Harrison J, Boachie-Adjei K, Lutz G. Intradiscal platelet-rich plasma (PRP) injections for discogenic low back pain: an update. Int Orthop. 2016 Jun;40(6):1321-8. doi: 10.1007/s00264-016-3178-3. Epub 2016 Apr 12. PMID: 27073034.
(13) Cheng J, Santiago KA, Nguyen JT, Solomon JL, Lutz GE. Treatment of symptomatic degenerative intervertebral discs with autologous platelet-rich plasma: follow-up at 5-9 years. Regen Med. 2019 Sep;14(9):831-840. doi: 10.2217/rme-2019-0040. Epub 2019 Aug 29. PMID: 31464577; PMCID: PMC6770415.
(14) Xu J, Xie G, Yang W, Wang W, Zuo Z, Wang W. Platelet-rich plasma attenuates intervertebral disc degeneration via delivering miR-141-3p-containing exosomes. Cell Cycle. 2021 Aug;20(15):1487-1499. doi: 10.1080/15384101.2021.1949839. Epub 2021 Jul 7. PMID: 34229586; PMCID: PMC8354670.
(15) Qian J, Wang X, Su G, Shu X, Huang Z, Jiang H, Zhu Q. Platelet-rich plasma-derived exosomes attenuate intervertebral disc degeneration by promoting NLRP3 autophagic degradation in macrophages. Int Immunopharmacol. 2022 Sep;110:108962. doi: 10.1016/j.intimp.2022.108962. Epub 2022 Jun 24. PMID: 35753124.
(16) Li P, Zhang R, Zhou Q. Efficacy of Platelet-Rich Plasma in Retarding Intervertebral Disc Degeneration: A Meta-Analysis of Animal Studies. Biomed Res Int. 2017;2017:7919201. doi: 10.1155/2017/7919201. Epub 2017 Jul 2. PMID: 28752097; PMCID: PMC5511641.
(17) Fujii K, Yamazaki M, Kang JD, Risbud MV, Cho SK, Qureshi SA, Hecht AC, Iatridis JC. Discogenic Back Pain: Literature Review of Definition, Diagnosis, and Treatment. JBMR Plus. 2019 Mar 4;3(5):e10180. doi: 10.1002/jbm4.10180. PMID: 31131347; PMCID: PMC6524679.
(18) Centeno C, Markle J, Dodson E, Stemper I, Hyzy M, Williams C, Freeman M. The use of lumbar epidural injection of platelet lysate for treatment of radicular pain. J Exp Orthop. 2017 Nov 25;4(1):38. doi: 10.1186/s40634-017-0113-5. PMID: 29177632; PMCID: PMC5701904.
(19) Wongjarupong A, Pairuchvej S, Laohapornsvan P, Kotheeranurak V, Jitpakdee K, Yeekian C, Chanplakorn P. “Platelet-Rich Plasma” epidural injection an emerging strategy in lumbar disc herniation: a Randomized Controlled Trial. BMC Musculoskelet Disord. 2023 Apr 28;24(1):335. doi: 10.1186/s12891-023-06429-3. PMID: 37118707; PMCID: PMC10141936.
(20) Le VT, Nguyen Dao LT, Nguyen AM. Transforaminal injection of autologous platelet-rich plasma for lumbar disc herniation: A single-center prospective study in Vietnam. Asian J Surg. 2023 Jan;46(1):438-443. doi: 10.1016/j.asjsur.2022.05.047. Epub 2022 May 28. PMID: 35637114.
(21) Saraf A, Hussain A, Sandhu AS, Bishnoi S, Arora V. Transforaminal Injections of Platelet-Rich Plasma Compared with Steroid in Lumbar radiculopathy: A Prospective, Double-Blind Randomized Study. Indian J Orthop. 2023 May 5;57(7):1126-1133. doi: 10.1007/s43465-023-00898-3. PMID: 37384009; PMCID: PMC10293530.
(22) Bise S, Dallaudiere B, Pesquer L, Pedram M, Meyer P, Antoun MB, Hocquelet A, Silvestre A. Comparison of interlaminar CT-guided epidural platelet-rich plasma versus steroid injection in patients with lumbar radicular pain. Eur Radiol. 2020 Jun;30(6):3152-3160. doi: 10.1007/s00330-020-06733-9. Epub 2020 Feb 24. PMID: 32095875.
(23) Singh GK, Talawar P, Kumar A, Sharma RS, Purohit G, Bhandari B. Effect of autologous platelet-rich plasma (PRP) on low back pain in patients with prolapsed intervertebral disc: A randomised controlled trial. Indian J Anaesth. 2023 Mar;67(3):277-282. doi: 10.4103/ija.ija_821_22. Epub 2023 Mar 16. PMID: 37250523; PMCID: PMC10220156.
(24) Raj MA, Ampat G, Varacallo M. Sacroiliac Joint Pain. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470299/
(25) Chen AS, Solberg J, Smith C, Chi M, Lowder R, Christolias G, Singh JR. Intra-Articular Platelet Rich Plasma vs Corticosteroid Injections for Sacroiliac Joint Pain: A Double-Blinded, Randomized Clinical Trial. Pain Med. 2022 Jul 1;23(7):1266-1271. doi: 10.1093/pm/pnab332. PMID: 34850180.
(26) Singla V, Batra YK, Bharti N, Goni VG, Marwaha N. Steroid vs. Platelet-Rich Plasma in Ultrasound-Guided Sacroiliac Joint Injection for Chronic Low Back Pain. Pain Pract. 2017 Jul;17(6):782-791. doi: 10.1111/papr.12526. Epub 2016 Dec 1. PMID: 27677100.
(27) Kotb SY, Sherif NM, Saleh HA, Ahmed SF, Sakr HM, Taeimah MO. The role of intra-articular injection of autologous platelet-rich plasma versus corticosteroids in the treatment of synovitis in lumbar facet joint disease. Saudi Med J. 2022 Nov;43(11):1200-1208. doi: 10.15537/smj.2022.43.11.20220449. PMID: 36379530.
(28) Wu J, Zhou J, Liu C, Zhang J, Xiong W, Lv Y, Liu R, Wang R, Du Z, Zhang G, Liu Q. A Prospective Study Comparing Platelet-Rich Plasma and Local Anesthetic (LA)/Corticosteroid in Intra-Articular Injection for the Treatment of Lumbar Facet Joint Syndrome. Pain Pract. 2017 Sep;17(7):914-924. doi: 10.1111/papr.12544. Epub 2017 Feb 22. PMID: 27989008.
(29) Zielinski MA, Evans NE, Bae H, Kamrava E, Calodney A, Remley K, Benyamin R, Franc D, Peterson MR, Lovine J, Barrows HR, Mahdavi K, Kuhn TP, Jordan S. Safety and Efficacy of Platelet Rich Plasma for Treatment of Lumbar Discogenic Pain: A Prospective, Multicenter, Randomized, Double-blind Study. Pain Physician. 2022 Jan;25(1):29-34. PMID: 35051141.

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.