Jugular Vein Compression Due to the Neck and CCI
Can your neck compress critical blood vessels and cause other symptoms? Yes, it can and one of the most common causes is Craniocervical Instability or CCI causing C2 to compress the internal Jugular Vein. What is Jugular Vein Compression? How exactly does it happen? What can be done? Let’s dig in.
What Is the Jugular Vein?
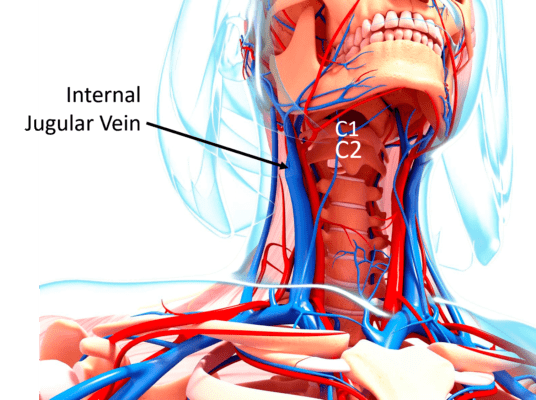
You have two Jugular Veins, the external and the internal. Here we’re talking about the internal Jugular Vein which runs from your brain, through a hole in your skull called the Jugular Foramen, and then down the inside front of your neck. It takes blood from the brain to your heart, so when it’s compressed, this causes blood to back up in the brain. It runs in front of the upper neck bones (c1 and c2).
Getty Images | By SHUBHANGI GANESHRAO KENE
Jugular Vein Compression
The most common site of Jugular Vein Compression seen clinically is in the upper neck. This can happen when the ligaments that hold the head on are loose which is a condition known as Craniocervical Instability or CCI. How does that work? Note above that the Jugular Vein runs right in front of C2. If that neck bone rotates, then the vein can be compressed when one side of C2 pivots forward. For example, the yellow arrow above points to the part of C2 that would rotate forward to compress the blue Jugular Vein.
Why Would C2 Rotate?
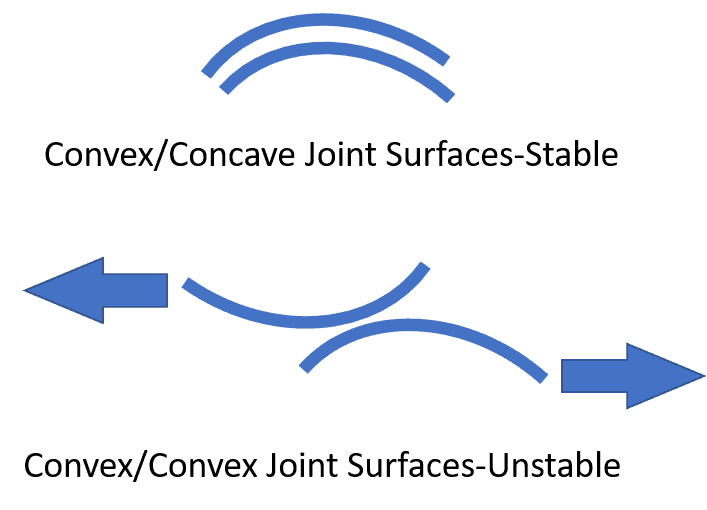
The C1-C2 joint is inherently unstable. Why? Most joints in the body are like a ball and socket (convex/concave) as shown above. As a result, they are inherently stable. Meaning without muscles or ligaments acting on them, they will mostly stay put. However, the C1-C2 joint is different. It’s a convex on convex joint. Hence, if the ligaments that hold the head onto the neck are loose, one joint surface will slide down the other as shown above. What that means is that C2 will rotate on C1. Which is where we can now tie in Jugular Vein Compression.
Jugular Vein Compression Due to CCI: A Patient Example
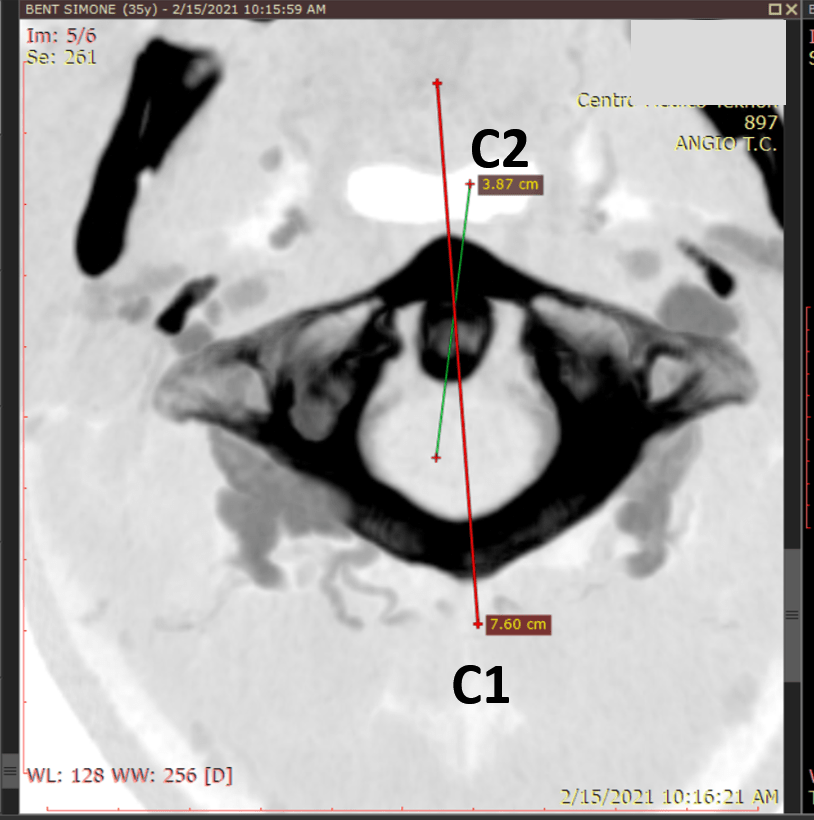
So now let’s look at some real patient images that demonstrate that this is happening. The first image shown above is a top-down view CT scan through the C1 bone. That’s the ring-shaped structure in black. The oval sitting in the front of that C1 bone is the dens of the C2 bone. The lines represent the front-back angle of each bone. Note that the two lines are off meaning that the bones are rotated against each other. The line marked C1 is almost straight (pointing slightly off to the left) and the line through the dens shows that C2 is rotated to the right. They shouldn’t be positioned like this as strong ligaments usually prevent this from happening, so this is reasonable evidence that the ligaments that hold the head on are too loose (CCI).
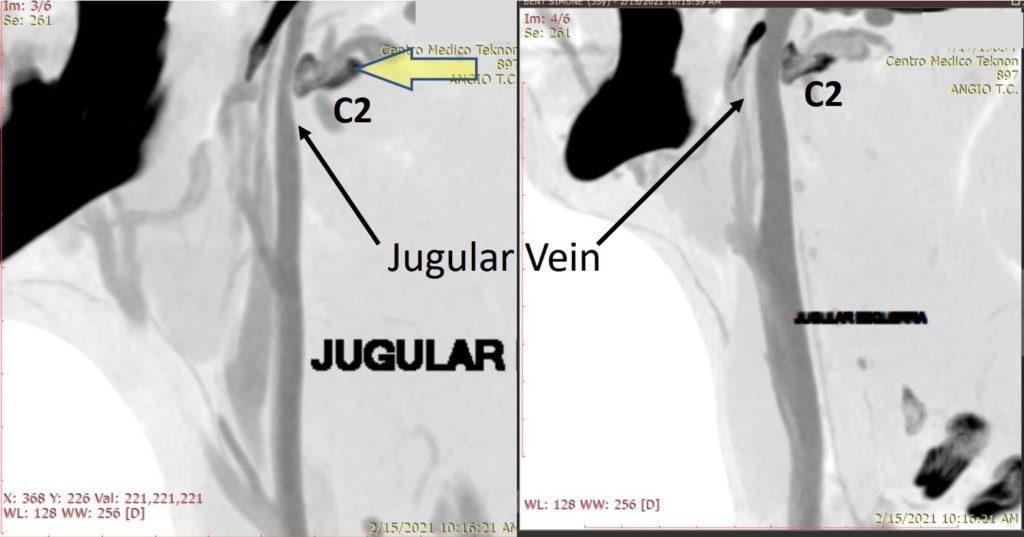
Next, we have actual images of the Jugular Vein filled with radiographic contrast so that it can be seen on a CT scan. The C2 bone is marked as a dark oblong-shaped structure. In the image on the left, C2 has rotated forward, placing pressure on the Jugular Vein so the vein is much smaller as it passes this bone. In the image on the right, the vein is normal size because the bone has gone slightly backward on that side. Hence, the image on the left shows Jugular Vein Compression.
What Are The Symptoms of Jugular Vein Compression?
Jugular Vein Compression can cause headaches, noises heard in the head, tinnitus (ringing in the ears), problems hearing, neck discomfort, stiffness, double or blurry vision, insomnia, and even transient amnesia (1). Some of these symptoms also overlap with CCI, so which problem is causing which symptoms may be hard to determine.
Eagle’s Syndrome and Jugular Vein Compression
This topic also overlaps with another condition called “Eagle Syndrome” which involves the styloid process that extends from the base of the skull. The ligaments that extend downward from this bone can become calcified and this can compress the internal Jugular Vein as well (2). In our experience, given that an elongated styloid process is common in patients without any problems at all, many of the patients diagnosed with Eagle Syndrome also have CCI, which makes diagnosing the issue causing the symptoms even more challenging. Other bones in the front of the neck like the Hyoid can also compress the Jugular Vein (3).
How Is this Problem Treated?
Most often, if this problem doesn’t resolve with conservative care like upper cervical chiropractic (NUCCA or AO), the next step that’s recommended is often upper neck fusion surgery. Here, most commonly, screws are placed across the C1-C2 joints to permanently immobilize this joint. However, we have seen high complication rates with these procedures.
Alternatively, tightening down the ligaments that hold the head-on with specific injections may help. Traditional prolotherapy where the ligaments in the back of the neck are injected is rarely effective in our experience. More likely to be effective is the PICL procedure which comes from the front using x-ray guidance to inject the patient’s bone marrow concentrate to tighten these ligaments.
How can tightening ligaments help? Realize that instability is a dynamic concept. Meaning that the vein gets compressed with head movement because the C1 and C2 bones move too much in the wrong directions (rotation against each other). Hence, tightening the ligaments that are supposed to prevent this motion can help avoid compressing the vein.
The upshot? Your neck bones can compress the vein that takes blood from your brain. This can cause all sorts of symptoms from brain fog to ringing in the ears. Helping this problem used to require surgery, but these days newer injection techniques help many patients avoid the knife!
_________________________________________
References:
(1) Li M, Su C, Fan C, Chan CC, Bai C, Meng R. Internal jugular vein stenosis induced by tortuous internal carotid artery compression: two case reports and literature review. J Int Med Res. 2019;47(8):3926-3933. doi:10.1177/0300060519860678
(2) Zamboni P, Scerrati A, Menegatti E, Galeotti R, Lapparelli M, Traina L, Tessari M, Ciorba A, De Bonis P, Pelucchi S. The eagle jugular syndrome. BMC Neurol. 2019 Dec 21;19(1):333. doi: 10.1186/s12883-019-1572-3. PMID: 31864313; PMCID: PMC6925502.
(3) Oushy S, Wald JT, Janus J, Fulgham JR, Lanzino G. Dynamic Internal Jugular Vein Compression by Hypertrophic Hyoid Bone: Management and Outcomes. Cureus. 2020;12(3):e7445. Published 2020 Mar 28. doi:10.7759/cureus.7445

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
