Lumbar Stenosis Treatment Without Surgery
One of the more amazing changes in our spine practice over the last several years has been on how we look at lumbar stenosis. I’ve gone from referring almost all of these patients to surgery to referring very few. Why? We reimagined what was going on with these patients. Lumbar stenosis treatment without surgery is possible. Let me explain through a recent patient result.
What is Central Canal Stenosis?
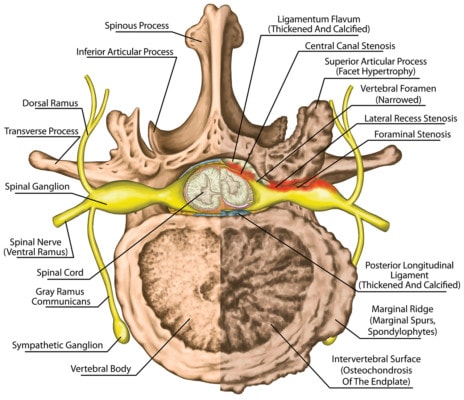
The right side of the illustration shows central canal stenosis. Stihii/Shutterstock
The spinal cord travels through a hole in the spine bones (central canal of the vertebrae) and it ends just above the start of your low back (usually T12 or so). From there on down, it’s actually a bunch of nerves that’s been called the cauda equina because it looks like a horse’s tail. The central canal where the spinal cord and nerves live has a ligament in the back called the “ligmentum flavum”. With degenerative disc disease, this ligament can get swollen and hypertrophied (bigger). As shown to the left with the ligament in red, when the ligament gets bigger it can place pressure on the spinal cord or nerve roots running through the central canal. When this happens, it’s called spinal stenosis. In addition, the facet joints can get bigger putting pressure on the canal from the sides, or the disc can bulge making the canal smaller from the front. If all of that occurs at once, the normally oval spinal canal can look more like a triangle.
Spinal stenosis symptoms include numbness or tingling in the legs, back pain, and/or a lack of power in the legs. This is almost universally worse when the patient stands or extends and it gets better when the patient sits. Why? The ligamentum flavum buckles further into the canal when the person stands, placing more pressure on the spinal cord or cauda equina. When the patient is bent forward, this opens up the spinal canal.
Spinal Stenosis Surgery and Other Options
The traditional way to treat spinal stenosis is surgery. The surgeon takes the bony roof off the spinal canal. While this does a great job of opening up the area and solving the immediate symptoms, it also strips the critical stabilizing muscles and ligaments and destabilizes the spine. With this part of the spine unstable, other problems like further degenerative disc disease occur over time. So traditional surgery solves one problem and creates another. To try and fix the instability issue, a lumbar fusion is also usually performed, which means bolting together the two vertebrae. However, this also fixes one problem and causes another as the lack of movement caused by the fusion surgery can lead to adjacent segment disease. To learn more about that issue, watch my video below:
Another option is called a Coflex device, which is a spacer that goes between the spinous processes after surgical decompression. The idea is supposed to be that the device preserves some motion, but getting it in destroys the normal fascial, muscular, and ligamentous architecture of the spine. Hence, there is no surgery free lunch, it all destroys something.
Recently there have been other ways to address the issue. One minimally invasive procedure called MILD cuts the ligamentum flavum, which snaps back like a broken rubber band. Again, this opens up the area, but again, destabilizes the spine as this ligament helps to provide stability. There are also newer solutions like interspinous spacers that are placed using x-ray guidance like the Superion device. The problem again here is that even though this is placed using fluoroscopy without surgery, the device still destroys the normal ligament architecture going in and then places more pressure on the front of the spinal column where the discs live.
Lumbar Stenosis Treatment Without Surgery – Regenexx DDD
With the Regenexx DDD procedure, we reconceptualized what was going wrong with spinal stenosis. To better understand how we treat this issue differently without surgery, you need to understand how stenosis develops. Let’s dig in.
The spinal level that ends up developing stenosis first gets sloppy and moves too much, that’s called degenerative instability. That extra motion then causes facet joint arthritis and oftentimes the ligamentum flavum will get bigger. This hypertrophy is really the same thing that we see in tendons that get weaker. How does that work?
Let’s focus on why tendons get bigger when they get weak. A normal tendon is small and dense. When a tendon has more wear and tear than it can repair, your body throws more tissue at the problem. However, it’s unable to repair the tendon like the original, so while the per unit area strength of the tendon is less, since the tendon is larger, it can still handle the total loads placed on it. We often fix this using regenerative medicine by injecting substances that will prompt more repair in the tendon than the wear and tear it’s experiencing. This causes the tendon to get smaller and stronger. Now let’s translate these concepts into the ligamentum flavum.
If the ligamentum flavum also gets more wear and tear than it can repair, it also gets larger or undergoes hypertrophy. Hence, it would make sense that injecting substances that can repair this ligament should make it smaller. A smaller ligament means less pressure on the nerves. However, nobody had ever intentionally injected anything into the ligamentum flavum before. Hence, we needed to develop new x-ray guided injection techniques for the DDD procedure.
We also focus on treating the whole functional spinal unit in this procedure. Meaning, we also perform precise image-guided injections to strengthen the ligaments and muscles that support this spinal segment, help arthritis in the joint, and reduce the swelling around the irritated spinal nerves. To learn more, see my video below:
Yoga and Stenosis Don’t Mix
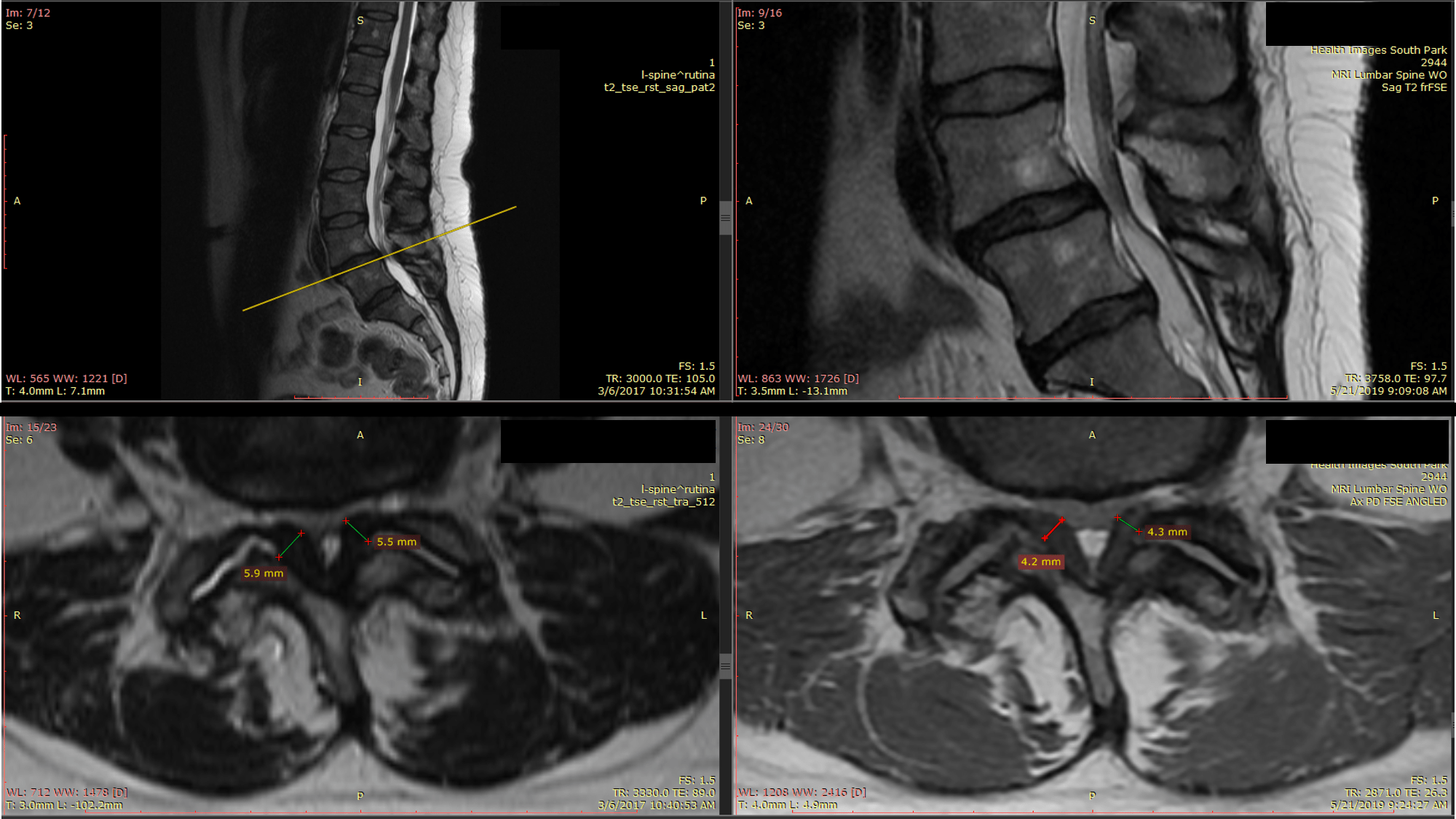
The MRIs above are from a patient who was big into Yoga, but could no longer stand for any length of time, hike, perform bridges, or sleep well. She had two Regenexx DDD procedures from Dr. Markle and now 1-2 years later she can do all of these things without having had any surgery. She will likely need one more treatment.
First, the MRI films above show the spinal canal upside down compared to my diagram. Meaning the ligamentum flavum is now on the bottom of the picture since the patient is lying face up in the machine. Her MRIs demonstrate that her ligamentum flavum hypertrophy has improved by about 25% (the width measurements you see on the before image on the left and the after image on the right). That’s all that’s usually needed to get rid of symptoms.
The upshot? We now routinely do lumbar stenosis treatment without surgery. In fact, good results with these patients have become so common that it’s been a while since I’ve sent one of these patients to get surgery. So hopefully you can avoid big destructive procedures or even small destructive procedures and leave your original anatomy intact.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
