Understanding Meniscus Tear MRI
An MRI, or magnetic resonance imaging, is a commonly used diagnostic tool that provides detailed images of soft tissues, including the meniscus in the knee.
While MRIs are useful in visualizing these injuries, they may not detect all types of tears or the complete severity of some injuries. This can sometimes lead to recommendations for surgery, which may not always be the most suitable treatment option.
Physicians in the licensed Regenexx network use the SANS evaluation method, which involves a detailed assessment of knee movement, sometimes combined with ultrasound, to evaluate meniscus injuries. Some individuals explore procedures using Regenexx injectates as a non-surgical option to support function and mobility.
The Anatomy Of The Meniscus Cartilage
The meniscus is a C-shaped piece of cartilage in the knee joint that acts as a cushion and provides stability during movement. Each knee has two menisci:
- Medial meniscus: Located on the inner side of the knee, the medial meniscus is larger and less mobile. This makes it more prone to injury, especially from twisting motions.
- Lateral meniscus: Found on the outer side of the knee, the lateral meniscus is smaller and more mobile. It allows for different movements and absorbs shock effectively.
Each meniscus can be subdivided into three distinct zones, based on the presence of blood flow:
- Red zone: The outer edge of the meniscus has a rich blood supply, allowing tears in this area to heal more easily.
- Red-white zone: The middle section has limited blood flow, so healing is more difficult but still possible.
- White zone: The inner portion has no blood supply, making tears in this area less likely to heal on their own.
A 2020 study with a sample of over 1,000 participants on the prevalence and location of meniscus tears reported that around 41% of injuries occur in the red zone, and a further 21% occur in the red-white zone.
How The Meniscus Functions
The meniscus serves several critical roles in knee function:
- Shock absorption: The meniscus acts as a cushion, absorbing impact from activities like walking, running, or jumping. Without this cushioning, the bones of the knee would rub against each other, causing pain and damaging the joint over time.
- Weight distribution: It evenly spreads the body’s weight across the knee joint, helping to prevent overloading certain areas. This reduces the risk of joint wear and tear, especially on the cartilage covering the bones.
- Joint stability: The meniscus helps stabilize the joint and prevents excessive movement that could lead to injury.
A damaged meniscus can compromise these functions, leading to pain, instability, and, over time, joint damage.
Meniscus Tear On MRI Explained
Magnetic resonance imaging (MRI) uses magnets and radio waves to create detailed pictures of soft tissues like cartilage in the knee. On an MRI, the meniscus appears as a “C-shaped” structure cushioning the bones in the knee. These imaging tests can show even small changes in the meniscus, which makes them helpful for finding injuries.
However, MRIs are not always accurate when it comes to determining the type or severity of the ear. When seen on MRIs, some meniscus tears may lead to recommendations for surgery, even though they might not be causing symptoms.
A 2008 study published in the New England Journal of Medicine found that in 61% of individuals over age 50, meniscus tears detected by MRI did not result in symptoms like pain or stiffness. These findings suggest that many meniscal tears are incidental and may not require immediate surgical intervention, highlighting the importance of cautious clinical evaluation when considering surgical treatment options.
The History Of MRI Findings And Knee Pain
It may seem logical to assume that finding a meniscus tear on an MRI would indicate that it is the cause of knee pain. However, the relationship between MRI findings and symptoms is more complex.
The 2008 study mentioned above found that most individuals over age 35 without knee pain had evidence of meniscus tears and cartilage loss on their MRI scans. This discovery led to serious questioning of whether meniscus tears on MRI were always significant or simply part of the natural aging process.
Building on this, a 2014 editorial by Scandinavian researchers suggested that degenerative meniscus tears should be viewed as signs of aging, much like wrinkles, and not automatically linked to knee pain or used as a sole justification for surgical treatment.
Do you want to learn more about how to read your knee MRI? See our video below:
New research examined 230 knees of patients without knee pain using a 3 Tesla MRI scanner. These scanners provide higher resolution—up to two or three times greater than many standard MRI machines—allowing for more detailed images of the knee. As a result, these advanced machines detect more potential abnormalities in the knee compared to standard MRI equipment.
The scans revealed abnormalities in 97% of patients without knee pain. Thirty percent showed meniscus tears, cartilage damage, and bone marrow lesions near the knee cap area (patellofemoral joint). Additionally, about one-third of the knees had cartilage lesions, and tendon issues were identified in about 20% of patients.
These findings suggest that many meniscus tears detected on MRI may not require treatment, depending on the clinical evaluation and symptoms present. This raises the question of whether meniscus tears seen on MRI scans in patients with knee pain should always be a cause for concern.
Analyzing A Torn Meniscus MRI
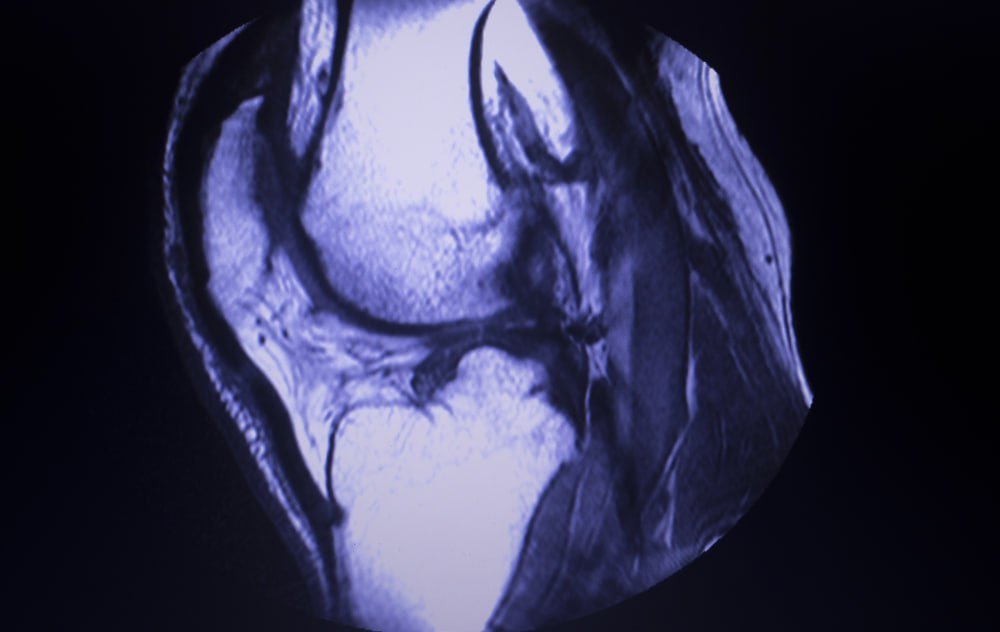
On MRI, a healthy meniscus appears as a dark, smooth C-shaped structure made of dense cartilage, of a consistent thickness and shape throughout and without any breaks or irregularities. When a tear is present, the MRI image shows irregular bright lines or gaps in the meniscus, indicating areas where the cartilage is damaged.
Tears can vary in size and location, with some showing minor fraying at the edges, while others may have significant separation or displacement of the meniscus tissue.
Physicians evaluate these images carefully, assessing the tear’s size, location, and its effect on surrounding tissues to determine the severity and appropriate treatment options.
Grading Of Tears
Meniscus tears are graded on a scale from 1 to 3 based on their severity, as seen on MRI. This helps guide treatment decisions.
Grade 1
Mild meniscus tears are categorized as grade 1. Grade 1 tears involve small internal damage that does not extend to the surface of the meniscus. Symptoms may include slight discomfort or stiffness, but pain is often minimal or absent.
On MRI, this tear appears as a small area of increased signal, or brightness, within the body of the meniscus.
Grade 2
A grade 2 meniscus tear is moderate in severity, sometimes causing more noticeable discomfort and stiffness. It still does not extend to the surface of the meniscus but affects a larger portion compared to grade 1. Patients may experience intermittent pain and limited mobility.
On MRI, a grade 2 tear appears as a larger bright area within the meniscus, but it still does not reach the surface. While the tear is larger than in grade 1, it generally does not require surgical treatment unless symptoms worsen.
Grade 3
A grade 3 meniscus tear is the most severe, often resulting in persistent pain, swelling, and impaired knee function. This type of tear extends through the meniscus and can cause significant discomfort. In a grade 3 tear, pieces of the meniscus can sometimes become stuck in the knee joint, causing the knee to lock or catch, making it difficult to straighten the leg.
On MRI, a grade 3 tear is visible as a bright signal that reaches the meniscus surface, indicating a complete tear, which is also known as full-thickness. This type of tear may require more complex treatment.
Types Of Torn Meniscus
Besides severity, meniscus tears may also be categorized on location and shape. These may be visible on an MRI:
- Radial tear: A radial tear is a common meniscus tear that extends from the center of the meniscus outward. It disrupts the ability of the meniscus to absorb shock, often causing pain, swelling, and joint instability. On MRI, a radial tear appears as a distinct line extending through the meniscus. This type of tear may worsen over time.
- Horizontal tear: A horizontal tear occurs along the length of the meniscus, separating the meniscus into an upper and lower section. This tear typically causes mild to moderate pain and may lead to knee catching or locking. On MRI, it appears as a line that runs parallel to the surface of the meniscus.
- Incomplete tear: An incomplete tear is a partial tear that does not fully extend through the meniscus. It often causes mild pain or discomfort, but symptoms may be minimal. On MRI, an incomplete tear shows as a slight difference in brightness within the meniscus.
- Complex tear: A complex tear involves multiple tear patterns, combining characteristics of radial, horizontal, and oblique tears. It typically results in notable knee pain, swelling, and limited mobility. On MRI, a complex tear appears as irregular signals with multiple brighter lines through the meniscus.
- Flap tear: A flap tear occurs when a portion of the meniscus becomes loose, creating a “flap” of tissue that can catch in the joint. This tear often leads to sharp pain, knee locking, and swelling. On MRI, a flap tear shows a piece of the meniscus that has become loose or detached, which may move within the joint.
- Bucket handle tear: A bucket handle tear is a severe type of longitudinal tear where a piece of the meniscus becomes displaced, creating a handle-like shape. This tear causes severe pain, swelling, and joint locking. On MRI, it appears as a displaced section of the meniscus, often moved into the joint space.
Benefits and Limitations of MRI For Detecting Meniscus Injuries
MRI is essential to visualize soft tissue injuries. Unlike X-rays, which only show bones, MRI provides images of cartilage, ligaments, and other soft tissues.
A 2020 study shows that MRI has an accuracy of 80% to 95% in diagnosing meniscus tears, depending on the location of the injury. This makes it a highly effective tool for detecting meniscus problems when combined with physical examinations performed by well-trained physicians.
The advantages of this diagnostic method include:
- Detailed images: MRI provides high-resolution images of the meniscus, allowing physicians to see even small tears that other imaging methods may miss.
- Non-invasive: Unlike diagnostic arthroscopy, which requires inserting a camera into the knee, MRI is completely non-invasive and typically pain-free.
- No radiation exposure: Unlike X-rays or CT scans, MRI uses magnetic fields instead of radiation, reducing potential health risks.
MRI may also have some limitations:
- Over-diagnosis of tears: Some meniscus tears seen on MRI are minor or age-related and may not require treatment, which can sometimes lead to unnecessary interventions.
- Difficulty differentiating tear types: MRI often cannot distinguish between degenerative and acute tears, potentially leading to misinterpretation of injury severity.
- False positives: MRI may show normal tissue variations that resemble tears, leading to unnecessary concern or surgery.
- Lack of functional information: MRI provides structural details but does not offer information on how the tear affects knee movement or overall function, which can sometimes lead to unnecessary treatments.
Coupled with other diagnostic methods, MRI can help address a torn meniscus promptly. In some cases, leaving severe tears untreated can lead to complications, including:
- Chronic pain: A meniscus tear can cause chronic pain, particularly when moving the knee.
- Joint instability: A torn meniscus can affect the knee’s stability, increasing the risk of further injury.
- Osteoarthritis development: Long-term damage to the meniscus can increase cartilage wear and tear, raising the risk of developing osteoarthritis over time.
Should Meniscus Tears Always Call For Surgery?
Common treatment options for meniscus tears include:
- At-home care: Rest, ice, compression, and elevation (RICE) may help alleviate pain and swelling. However, prolonged icing may slow down healing by reducing blood flow to the injury site.
- Physical therapy: Physical therapy can help strengthen the muscles surrounding the knee, improving joint support, flexibility, and stability.
- Medications: Non-steroidal anti-inflammatory drugs (NSAIDs) can help temporarily ease pain and inflammation. However, long-term use of NSAIDs can increase the risk of side effects such as heart attack, stroke, stomach ulcers, and kidney disease.
Surgery may be considered for severe, full-thickness tears, especially when they lead to symptoms like knee locking or instability. However, many degenerative meniscus tears respond well to non-surgical treatments.
Additionally, certain mild to moderate tears that occur in the red and red-white zones of the meniscus may sometimes heal on their own, thanks to the blood supply in these areas.
Research suggests surgery for meniscus tears may offer limited benefit compared to non-surgical treatments like physical therapy:
- Studies have shown that arthroscopic partial meniscectomy, a common surgery for meniscus tears, often provides limited benefit compared to non-surgical options like physical therapy.
- A 2022 study indicates that meniscus tears can cause the development of osteoarthritis or aggravate this condition. The study reports that 81% of knees showed signs of osteoarthritis after surgical removal of the meniscus, compared to 18% of healthy knees.
- A 2023 study on 605 patients found that meniscus removal did not show better outcomes than non-operative treatment for any group of patients.
Surgery may be considered for acute traumatic tears that cause knee locking, instability, or severe pain. However, for most degenerative tears, conservative treatments such as physical therapy are often effective, reducing the need for surgery.
Support Knee Function Without Surgery
A torn meniscus diagnosis doesn’t always mean surgery is required. Physicians in the licensed Regenexx network use interventional orthobiologics to support the body’s natural healing process. This approach may offer a less invasive alternative for individuals exploring options to surgery for meniscus tears.
While surgery may still be necessary in some cases, non-surgical procedures using Regenexx lab processes may help support joint function and manage symptoms. Explore how this approach may help you maintain mobility and address knee discomfort without surgery.
Originally published on

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
