New Article on Your Multifidus and Cytokines
If you read this blog regularly, you’ve heard about the most important back muscle many physicians have never heard about called the Multifidus. Now new research lends an interesting twist to the story of this critical muscle. Let’s dig into cytokines and your Multifidus.
What Is the Multifidus?
Multifidus is a deep spinal muscle that’s the red-headed stepchild of causes of low back pain. It just doesn’t get the attention from doctors that it deserves. To learn more about why this muscle could be causing your back pain without you knowing about it, watch my video below from 2017:
What Are Cytokines?
Cytokines are chemical messengers between cells. They can signal all sorts of things like to recruit more cells to break down and heal injured tissue (acute inflammation), to stay idle without healing (chronic or bad inflammation), or to create more blood vessels. Hence, the amounts, types, and ratios of various cytokines in your tissues can have an immense impact on the health of those parts of your body.
The New Research
Surgeons took Multifidus muscle and epidural fat samples from the spines of individuals who were undergoing surgery for a herniated disc. The epidural fat was taken to see what was happening at the interface between the herniated disc and the nerve. What did they find after analyzing these tissues for cytokine content (gene expression)?
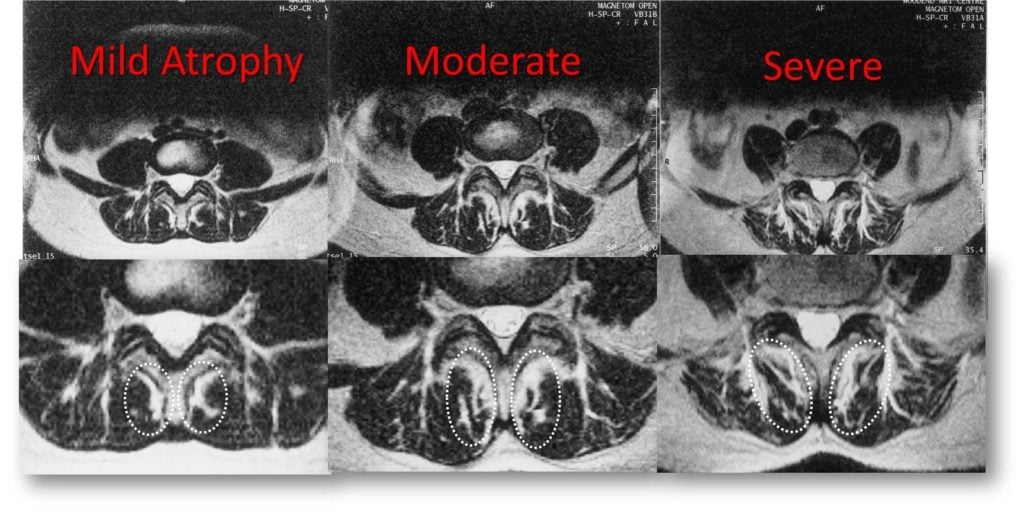
Inflammatory cytokine levels (TNF expression) in the Multifidus muscle were greater in participants with greater Multifidus atrophy. This group also had a greater expression of leptin, a hormone associated with metabolic syndrome. In the epidural fat, they found cytokines that were associated with inflammatory macrophages (the garbage men of the body who are trying to clean up the herniated disc material (TNF, adiponectin and nitric oxide synthase 2). They also found anti-inflammatory macrophages elsewhere.
What Does All of This Mean?
The researchers felt that there was something called “inflammatory dysregulation” happening. Basically, that the normal inflammatory process that happens to try to heal damaged tissue was spinning out of control. I interpret this as chronic inflammation where the body can’t complete the job of healing. One explanation is that for patients with metabolic syndrome (low activity, high blood pressure, pre-diabetes, and high triglycerides) there is an injury to the disc that can’t heal itself because of the patient’s tendency toward chronic inflammation. It’s partly because of this that the Multifidus begins to atrophy. In addition, there is less nerve input on the muscle because of the effects on the exiting spinal nerve, which also adds to the atrophy. Meaning a pissed-off nerve can’t fire the Multifidus well, hence it atrophies.
For example, we know that patients with more whole-body inflammation are more likely to have a longer course of back pain after a herniated disc (2). What can you do to clean up that bad inflammation? Diet is key and Dr. Pitts has a great free download book called Nutrition 2.0 on that topic here. Another thing to do is to take anti-inflammatory supplements.
What Are the Implications for Orthobiologics?
The implications to me are clear. Because of the effect of metabolic syndrome on Multifidus, the patient needs to clean up their diet and exercise routine. However, exercising can be super challenging with back pain. Hence, another strategy is helping to clean up the local chronic inflammation by injecting things like PRP to kick the area into acute and healing inflammation. We’ve been using PPP (platelet-poor plasma) and PRP (Platelet-rich Plasma) in the atrophied Multifidus for many years now.
The upshot? While we’ve known that Multifidus atrophy is associated with low back pain and irritated low back nerves, this new study makes us think about what’s happening chemically as well. It also outlines why injecting orthobiologics into the atrophied muscle may help.
________________________________________________
References:
(1) James, G., Chen, X., Diwan, A. et al. Fat infiltration in the multifidus muscle is related to inflammatory cytokine expression in the muscle and epidural adipose tissue in individuals undergoing surgery for intervertebral disc herniation. Eur Spine J 30, 837–845 (2021). https://doi.org/10.1007/s00586-020-06514-4
(2) Schistad EI, Espeland A, Pedersen LM, Sandvik L, Gjerstad J, Røe C. Association between baseline IL-6 and 1-year recovery in lumbar radicular pain. Eur J Pain. 2014 Nov;18(10):1394-401. doi: 10.1002/j.1532-2149.2014.502.x. Epub 2014 Apr 2. PMID: 24692238.

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
