New Study of Many Cell Therapies Versus Steroid Yields Interesting Results
We’re entering a time where we will continue to see large, high-quality studies published in orthobiologics. This has been happening in the PRP world for the last half-decade or more, but it is also about to happen in the world of bone marrow, adipose stromal vascular fraction, and umbilical cord stem cells. Another entry in this new study class was published just this past month, and its results are unexpected and confusing. So, let’s dive into it today and try to learn as much as possible.
What Are the Different Orthobiologics We Will Be Discussing?
The orthobiologics tested in this study include BMC or Bone Marrow Concentrate, SVF or Stromal Vascular Fraction, and Culture Expanded Umbilical Cord MSCs. Let’s go through each one:
- Bone Marrow Concentrate (aka BMAC): This is made by taking bone marrow aspirate and concentrating the cell-containing fraction in a centrifuge. This is permitted by the US FDA right now.
- SVF (Stromal Vascular Fraction): Adipose tissue is taken by liposuction and then digested using an enzyme to access the cells, which are then centrifuged. This is a drug that requires FDA approval.
- Culture Expanded Umbilical Cord MSCs– This biologic is created by harvesting umbilical cord Wharton’s Jelly, digesting it with an enzyme, centrifuging, and then placing it in culture to isolate and grow more mesenchymal stem cells. This is another drug requiring FDA approval.
In this study, a corticosteroid injection was also used. This is the standard anti-inflammatory injection given in doctor’s offices worldwide. This is a mega dose of steroid, usually about 100,000-1,000,000 times the dose that your body would use on a day-to-day basis.
The Money Shot
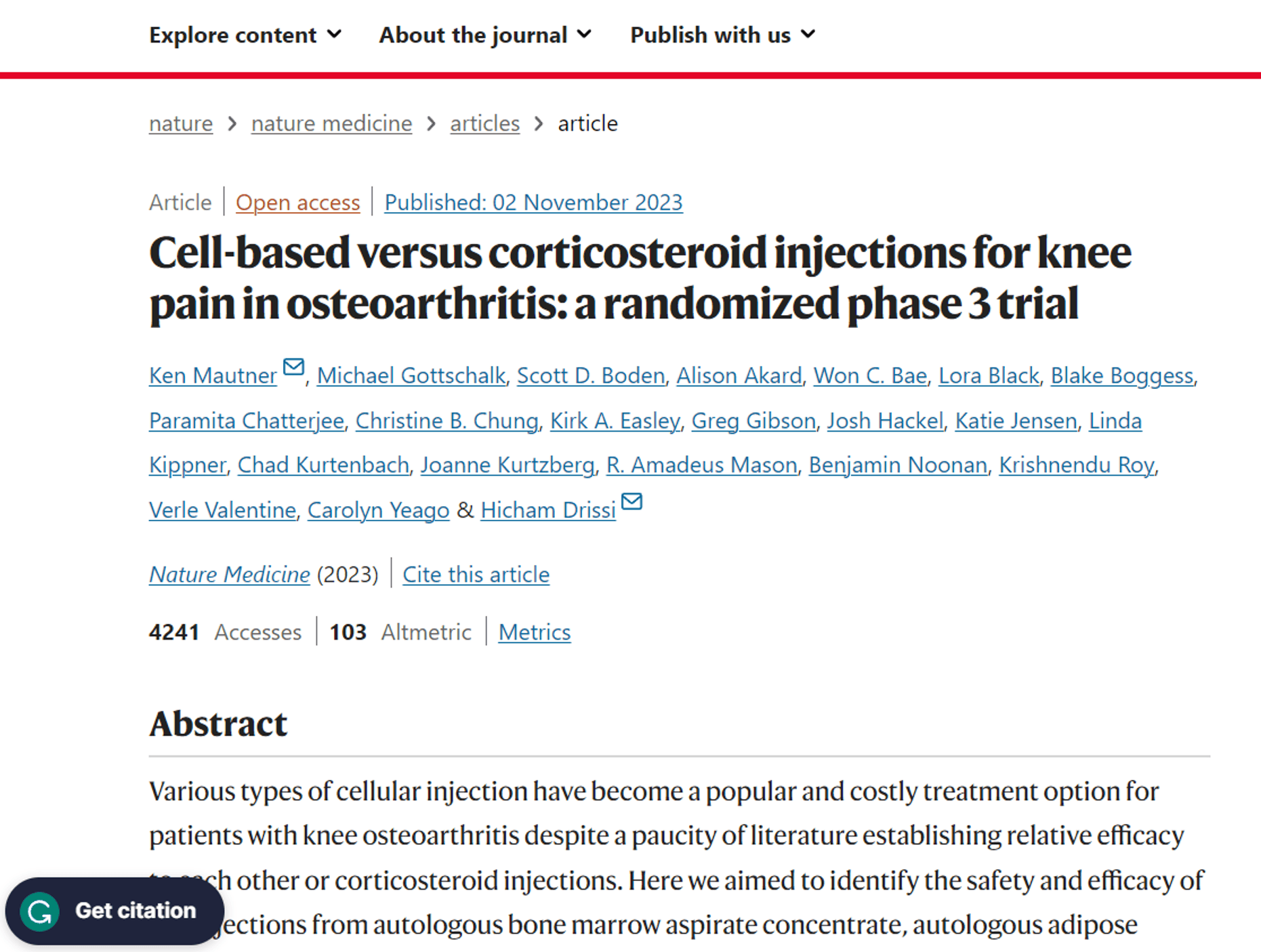
Most studies have one or two graphs that tell you in a simple way what the authors found, and this one is no different:
Here, we see the four interventions graphed on a functional scale (KOOS) where more is better. What can we see? The two interventions that seem to have done the best at all of the time points up to one year are the BMAC and the steroid. The intervention that appears to have done the worst at all time points up to one year is the expanded umbilical cord stem cells. For all months after the first, the SVF falls between those two (BMAC/Steroid and SVF). It should be noted that none of these differences were statistically different at any time point. Hence, it’s better to call these “trends” and not differences.
The First Unusual Finding of This Study
In this study, a corticosteroid shot worked very well for a year. That’s a little atypical, depending on the severity of the arthritis. For example, based on my clinical experience, a steroid shot can last a long time in moderate arthritis, but in severe knee arthritis, it usually provides shorter-lasting relief.
Based on high-level RCTs, do corticosteroids work to treat knee arthritis pain? The most extensive and most accomplished study was done in 2017 and published in the New England Journal of Medicine. It showed that at two years, there was no difference between a steroid shot and saline (2). It also showed that the steroid shot damaged knee cartilage over those two years, eroding about double the cartilage that normal wear and tear accomplished over that period. Realize that the two-year results of this study have yet to be published.
More Steroid Side Effects
There’s a reason the doctors who have adopted orthobiologics have ditched steroid injections, even beyond the fact that they destroy joint cartilage:
- A knee steroid shot increases the likelihood of a subsequent knee replacement failure or infection (11).
- A steroid injection also has systemic side effects like decreasing bone density, disrupting your cortisol endocrine system, and spiking your blood sugar (12-14).
Orthobiologics vs Steroid
What can we learn about the new study by comparing it to other RCTs that have tested orthobiologics against a steroid shot? Maybe quite a bit.
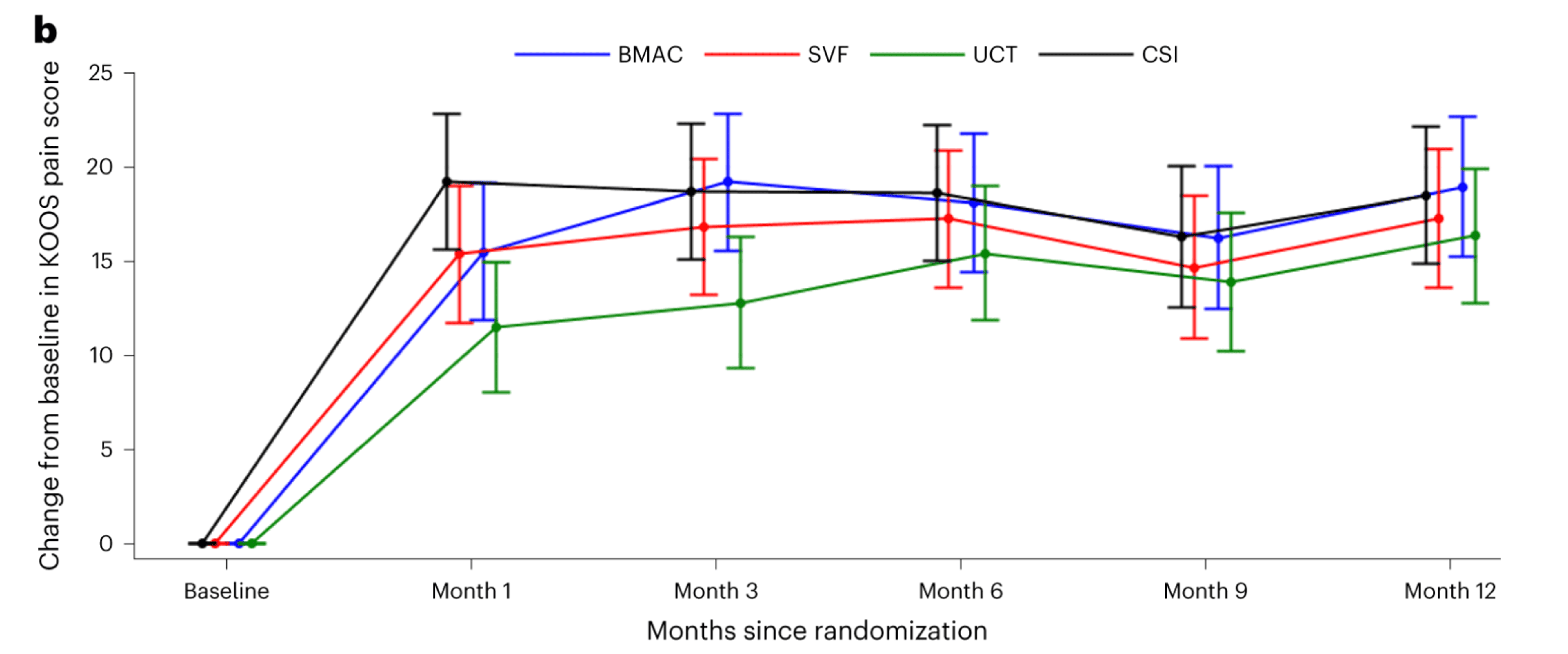
Platelet-rich plasma has been tested in at least a half dozen randomized controlled trials against steroids (3-8). In general, the graphs from three of these positive studies are emblematic of what’s usually seen:
If you look above, you can see that as time goes on, there is a separation between the steroid and the PRP, with the PRP performing better.
This is how these six studies turned out:
- Three studies showed that PRP was superior compared to steroids (3, 5, 6). All three studies exceeded the minimum 2X PRP definition.
- One study showed that a steroid injection before a PRP injection seemed to work better (4).
- One study showed that “PRP” was non-inferior to steroids, but that study didn’t meet the 2X PRP threshold (8).
- One study showed that “PRP” was no better than saline placebo (regrettably, this study also never used a product that met the minimum 2X definition for PRP) (7).
Who Was Treated in Each Group?
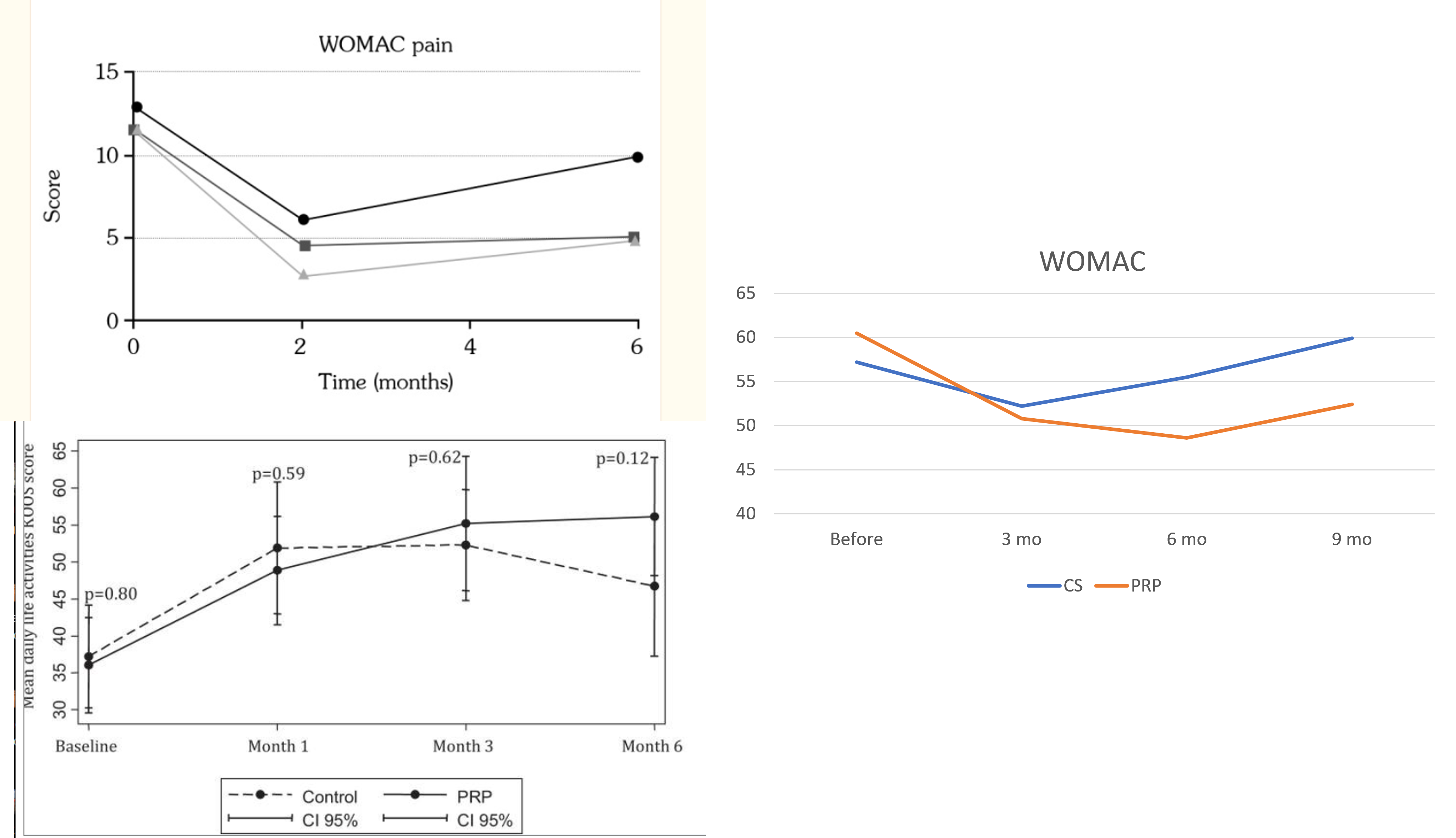
The first critical piece of information we need to interpret a study like this is how old these patients were and how severe the arthritis was in these groups. First on age, here’s the breakdown of the under and over 60 for the whole study:
So, this is a primarily elderly group with a younger mean age of 58.
How did the distribution of moderate and severe arthritis look in each group? Meaning, was this an identical distribution?
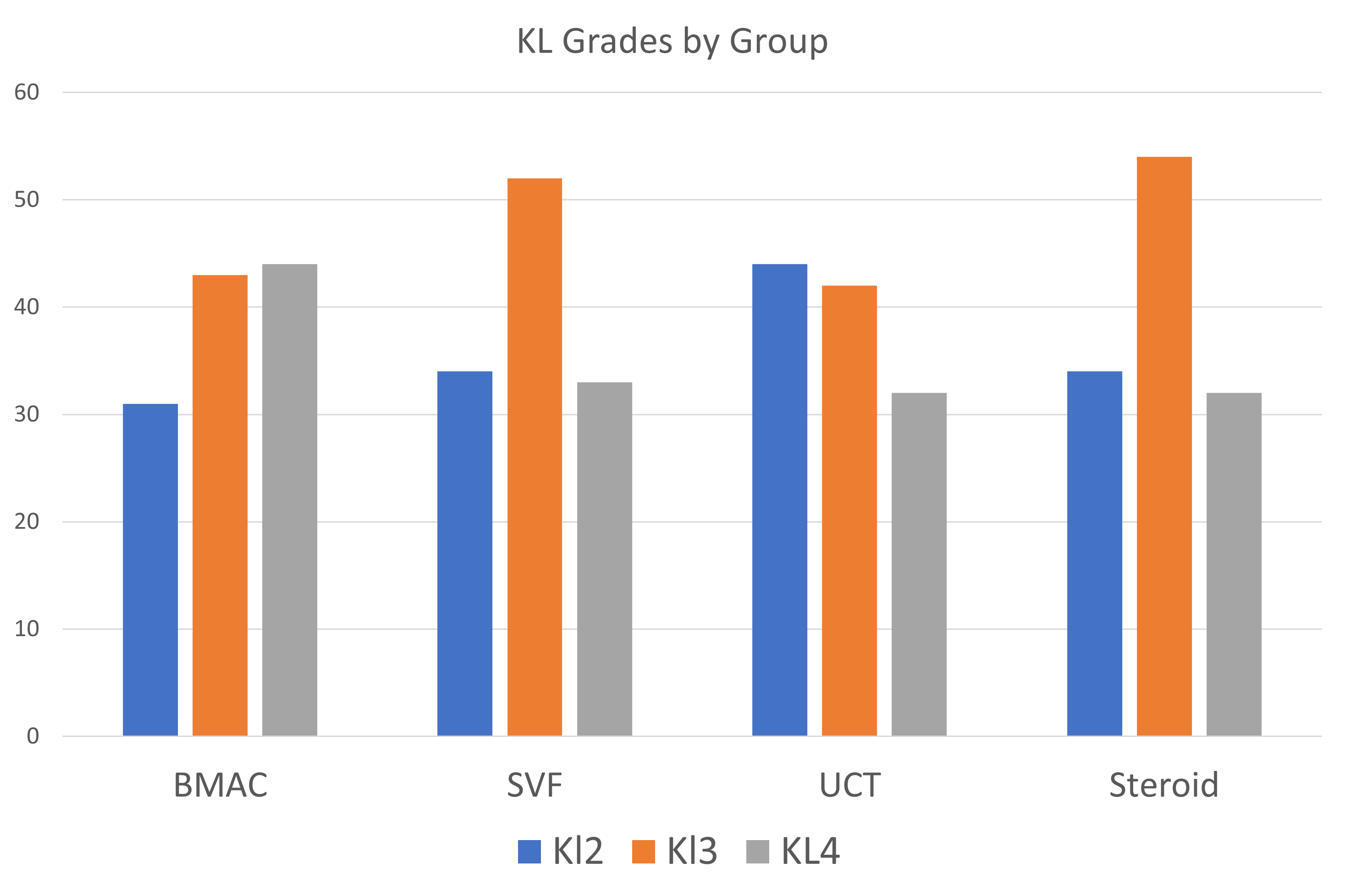
To understand the graph above, you need to know that the Kellgren-Lawrence (KL) Grading scale is from 0-4. KL2 is moderate arthritis, KL3 is moderate-severe, and KL4 is severe.
The BMAC group had the highest proportion of severe arthritis cases (KL4). The UCT group had the highest proportion of moderate arthritis. The steroid group had a low proportion of severe cases.
We can see this discrepancy better if we compare the severe KL4 cases to the more moderate KL2/KL3 cases:
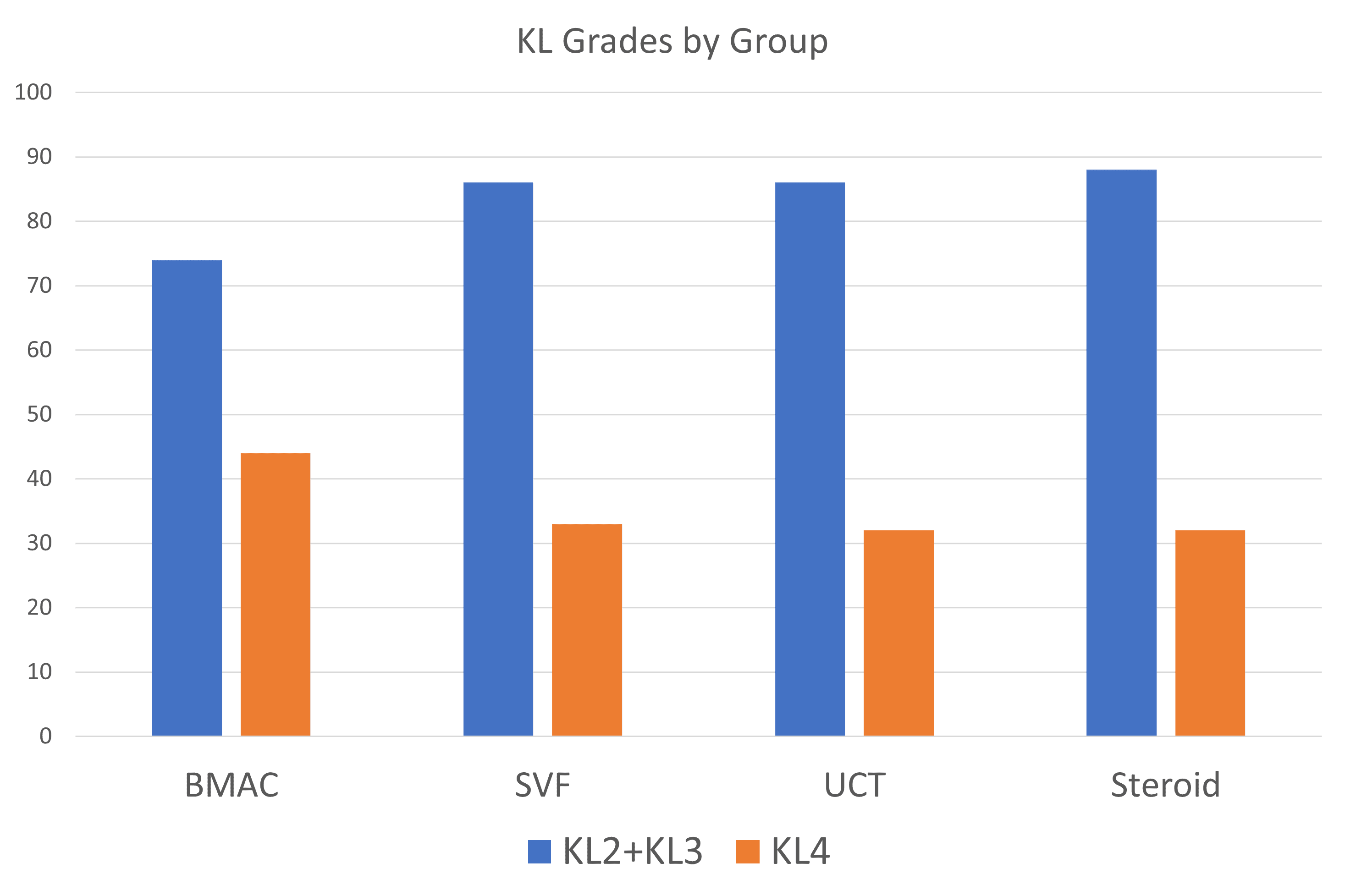
The BMC group looks quite different here, with a much higher proportion of severe versus moderate cases. Again, the steroid group has the most significant proportion of moderate versus severe cases. To understand that divide, the proportion of moderate to severe cases in the BMAC group is 1.7, while that same proportion in the steroid group is a whopping 2.75!
This may help explain why this study’s steroid shots lasted so long. There were almost three moderate knee arthritis cases in that group for every severe case.
Umbilical Cord MSCs Better?
One of the interesting things to note here is that the “young” umbilical cord cells didn’t beat the autologous bone marrow and fat therapies. That’s likely because these cells were allogeneic (from a donor). I have often reported on research showing that allogeneic stem cells are not invisible to the host’s immune system. They are detected and eliminated.
What Does Year Two Hold?
At this point, we don’t know what year 2 of this study tells us. First, it’s improbable that the steroid, given the New England Journal paper reviewed above, will still produce great results by 24 months, but with a less severe arthritis group, who knows? It’s also probable that some of these cell therapies will begin to separate themselves from the massive steroid anti-inflammatory and, ultimately, catabolic effect.
Inadequate BMC Treatment?
One of the differences between what’s done in this study and what’s now more commonly done in advanced orthobiologics practices is the use of intraosseous injections. Since Hernigou’s RCTs were published, showing the superiority of IO (Intraosseous) over intra-articular injections alone, many high-level clinics have made the switch (9,10). This study didn’t use the IO+IA treatment.
In addition, we’ve been treating ligamentous laxity in knee OA cases for over a decade. Many of these patients have a lax MCL, LCL, or ACL that needs to be targeted to maximize results. These are classified as “degenerative instability” and are not surgical issues, but in my clinical experience, treating these areas makes a big difference in the final outcome. This was not done in this study.
We also have no idea how good or bad the bone marrow aspirates were in this study. A good harvest technique is described, but only 60 ml was taken, which is low by today’s knee OA treatment standards. For example, the current Regenexx knee OA protocol for knee IA+IO is a 120 ml draw. The authors have promised to publish that data eventually.
To Review the Issues
As the authors of this study admit, there is no perfect study. Here are the issues I can find:
- No placebo control-These cell based treatments are compared to a known treatment. That’s not a critical error, as this is still valuable data.
- Steroids can be very effective in treating the inflammation generated by knee arthritis, but they destroy the joint, increase the likelihood of knee replacement infection and failure, and have adverse systemic side effects.
- The robust steroid results don’t agree with several other RCTs performed on PRP. That could be because there were far more moderate and fewer severe OA cases in the steroid group.
- There is a much higher proportion of severe arthritis cases in the BMC group than in the steroid control group!
- The culture-expanded Umbilical Cord group didn’t perform better, likely due to a seminal and unavoidable donor rejection problem with allogeneic cell products.
- The study tested an older and less effective IA BMC treatment, not the gold standard IA+IO used in 2023. It also neglected to address degenerative ligamentous instability.
The upshot? Interesting study, and I am thankful for all of the hard work put in by the authors, including Ken Mautner of Emory and his team. I look forward to more of this dataset getting published! In the meantime, I’m not sure it changes much for us.
____________________________________________
References:
(1) Mautner, K., Gottschalk, M., Boden, S. D., Akard, A., Bae, W. C., Black, L., Boggess, B., Chatterjee, P., Chung, C. B., Easley, K. A., Gibson, G., Hackel, J., Jensen, K., Kippner, L., Kurtenbach, C., Kurtzberg, J., Mason, R. A., Noonan, B., Roy, K., . . . Drissi, H. (2023). Cell-based versus corticosteroid injections for knee pain in osteoarthritis: A randomized phase 3 trial. Nature Medicine, 1-7. https://doi.org/10.1038/s41591-023-02632-w
(2) McAlindon TE, LaValley MP, Harvey WF, et al. Effect of Intra-articular Triamcinolone vs Saline on Knee Cartilage Volume and Pain in Patients With Knee Osteoarthritis: A Randomized Clinical Trial. JAMA.2017;317(19):1967–1975. doi: 10.1001/jama.2017.5283
(3) Uslu Güvendi E, Aşkin A, Güvendi G, Koçyiğit H. Comparison of Efficiency Between Corticosteroid and Platelet Rich Plasma Injection Therapies in Patients With Knee Osteoarthritis. Arch Rheumatol. 2017 Nov 2;33(3):273-281. doi: 10.5606/ArchRheumatol.2018.6608. PMID: 30632533; PMCID: PMC6328223.
(4) Camurcu Y, Sofu H, Ucpunar H, Kockara N, Cobden A, Duman S. Single-dose intra-articular corticosteroid injection prior to platelet-rich plasma injection resulted in better clinical outcomes in patients with knee osteoarthritis: A pilot study. J Back Musculoskelet Rehabil. 2018;31(4):603-610. doi: 10.3233/BMR-171066. PMID: 29710676.
(5) Arora V, Sharma M, Bishnoi S, Mahipal V, Sandhu AS, Khanna R, Aggarwal T, Yadav KS, Jain G, Sharma SM. Clinical and Biochemical Correlation of Intra-articular Platelet-Rich Plasma and Corticosteroid Using Serum Matrix Metalloproteinase 3 (MMP-3) Levels in Osteoarthritis of Knee. Cureus. 2023 May 29;15(5):e39625. doi: 10.7759/cureus.39625. PMID: 37388595; PMCID: PMC10301850.
(6) Joshi Jubert N, Rodríguez L, Reverté-Vinaixa MM, Navarro A. Platelet-Rich Plasma Injections for Advanced Knee Osteoarthritis: A Prospective, Randomized, Double-Blinded Clinical Trial. Orthop J Sports Med. 2017 Feb 13;5(2):2325967116689386. doi: 10.1177/2325967116689386. PMID: 28255569; PMCID: PMC5315239.
(7) Tschopp M, Pfirrmann CWA, Fucentese SF, Brunner F, Catanzaro S, Kühne N, Zwyssig I, Sutter R, Götschi T, Tanadini M, Rosskopf AB. A Randomized Trial of Intra-articular Injection Therapy for Knee Osteoarthritis. Invest Radiol. 2023 May 1;58(5):355-362. doi: 10.1097/RLI.0000000000000942. Epub 2022 Dec 27. PMID: 36728848; PMCID: PMC10090303.
(8) Pretorius J, Nemat N, Alsayed A, Mustafa A, Hammad Y, Shaju T, Nadeem S. Double-Blind Randomized Controlled Trial Comparing Platelet-Rich Plasma With Intra-Articular Corticosteroid Injections in Patients With Bilateral Knee Osteoarthritis. Cureus. 2022 Sep 29;14(9):e29744. doi: 10.7759/cureus.29744. PMID: 36324362; PMCID: PMC9617571.
(9) Hernigou P, Bouthors C, Bastard C, Flouzat Lachaniette CH, Rouard H, Dubory A. Subchondral bone or intra-articular injection of bone marrow concentrate mesenchymal stem cells in bilateral knee osteoarthritis: what better postpone knee arthroplasty at fifteen years? A randomized study. Int Orthop. 2020 Jul 2. doi: 10.1007/s00264-020-04687-7. Epub ahead of print. PMID: 32617651.
(10) Hernigou P, Delambre J, Quiennec S, Poignard A. Human bone marrow mesenchymal stem cell injection in subchondral lesions of knee osteoarthritis: a prospective randomized study versus contralateral arthroplasty at a mean fifteen year follow-up. Int Orthop. 2020 Apr 23. doi: 10.1007/s00264-020-04571-4. Epub ahead of print. PMID: 32322943.
(11) Richardson SS, Schairer WW, Sculco TP, Sculco PK. Comparison of Infection Risk with Corticosteroid or Hyaluronic Acid Injection Prior to Total Knee Arthroplasty. J Bone Joint Surg Am. 2019 Jan 16;101(2):112-118. doi: 10.2106/JBJS.18.00454.
(12) Kang SS, Hwang BM, Son H, Cheong IY, Lee SJ, Chung TY. Changes in bone mineral density in postmenopausal women treated with epidural steroid injections for lower back pain. Pain Physician. 2012 May-Jun;15(3):229-36.
(13) Chon JY, Moon HS. Salivary cortisol concentration changes after epidural steroid injection. Pain Physician. 2012 Nov-Dec;15(6):461-6.
(14) Habib GS. Systemic effects of intra-articular corticosteroids. Clin Rheumatol. 2009;28(7):749‐756. doi:10.1007/s10067-009-1135-x

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
