PRP Concentration vs. Dose: Why Concentration Is as Important as Dose
If you read this blog, you know I often write about what I experience daily. This past weekend an orthopedic surgeon on Linkedin promoted test tube PRP at 3-4X concentration. Like others I have seen, his focus was on the total dose delivered to a knee and not on the concentration. Meaning he posited that injecting a high volume of low-dose PRP in a knee was as good as injecting a low volume of high-dose PRP. So, let’s explore this idea today to see why focusing on total dose may cause problems. Let’s dig in.
PRP Concentration 101
If you had to come up with one way patients who get platelet-rich plasma to treat their joint pain, tendon tears, or spinal pain get ripped off, it’s by getting a PRP shot, which is too low in concentration. I have blogged on this issue many times because the problem is so rampant that it even infects the medical research in this area.
To understand why this happens, we need to review how platelets can impact healing. Platelets have loads of growth factors and exosomes. They release these over the first week to initiate and then help coordinate a repair response. As we age, our response to these growth factors changes. The bad news is that we have fewer circulating natural growth factors in our blood plasma as we age. The good news is that our research team has confirmed through many experiments that this causes your aged cells to be more sensitive to higher growth factor concentrations. For example, if we use two times concentrated PRP (2X) with twice the platelet count of whole blood, twenty-something-year-old cells will show some stimulation to grow better (proliferation). A 50-something person’s cells will show a similar but more muted response. However, as we move to a 10X PRP, while the young person’s cells won’t show much extra stimulation, an older person’s cells will have a major bump in proliferation. This difference is probably due to differences in cellular receptor density between old and young people.
This means to the average patient that if you are middle-aged or older, the clinic needs to draw a huge amount of blood to get a higher concentration PRP. If they draw just a few blood tubes, the PRP you’ll receive will be far too low a concentration to have a big clinical impact.
More Clinical Research that Platelet Dose Is the Key to Clinical Outcomes
A recent randomized controlled trial of a lower versus higher dose PRP was published, showing that patients with higher platelet doses had better clinical results than patients with lower doses (1). Because this study was ex-US, the only way they had to increase the dose was by injecting 8 ml of a 3.5X PRP versus 4 ml. This paper fits with another clinical study showing that higher dose PRP is more effective than lower dose and our in-vitro study that showed the same thing (2,3). It also fits my analysis, showing that a platelet concentration under 2X was associated with a much higher risk of clinical trial failure.
Hence, we have a simple message here:
- High Dose=Good
- Low Dose=Bad
The Fine Print on the Platelet Dose
Our understanding of life, the universe, and everything often comes down to understanding the fine print or, in other words, those details that can make things we thought were true turn out to be false and vice versa. In the case of PRP dose, that likely comes down to a factor called “final growth factor concentration.” What do I mean? I’m a visual thinker, so I drew several diagrams below. Each knee joint has the same dose of 60 platelets, with each red dot representing one platelet. However, just eyeballing the concentration of the dots tells an interesting story:
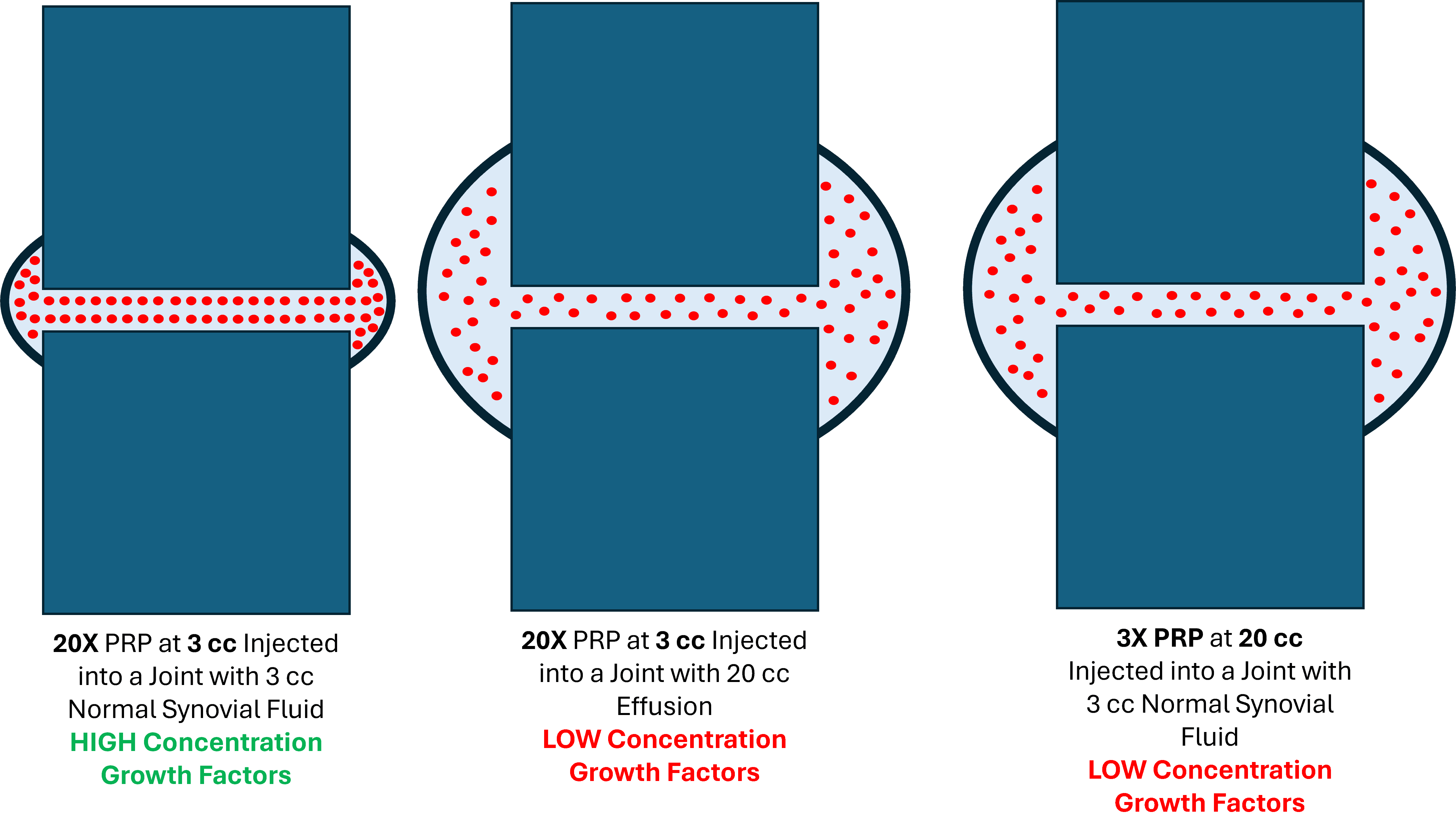
To simplify the math, my 60 platelets can be represented in several real-world ways. For example, they could be generated by injecting super-high concentrate PRP at 20X baseline in 3 ccs (20 X 3=60). Or the 60 platelets could be generated by injecting 3x PRP at 20 cc (3 X 20=60). In both cases, we end up with the same platelet dose in the joint. However, our diagram shows that these two clinical scenarios are quite different.
The knee joint on the far left, with the 20X PRP at 3 cc injected into a joint without an effusion, shows a high concentration of platelets. The knee joint on the far right, on the other hand, has the same 60 platelet dose, but the concentration of platelets is quite low because we used 3X at 20 ccs injection.
Why would platelet concentration in the joint matter?
Concentration Drives Cellular Activity
Several authors, including our research group, have shown that platelet concentration directly drives cellular activity like proliferation and repair (3-5). I did a deep dive into this published literature a few years back, as shown in this video:
Why does this happen? The response of the cells you’re trying to repair is directly related to the growth factor concentration in the solution. More concentrated growth factors cause a better proliferation response. Hence, this is why injecting 3cc of 20X PRP into a joint is NOT the same as injecting 20 cc of 3X PRP.
Now for more fine print. As discussed above, if you run these experiments of concentration versus proliferation with young cells (common since universities have a huge pool of young students), you get different results than running them with middle-aged or older cells. The good news is that the clinical diagnosis we’re discussing is osteoarthritis, which almost always happens in middle-aged and older people.
The Impact of Draining an Effusion
If you want to find one glaring and serious problem with the entire knee osteoarthritis orthobiologics literature it’s that no clinical trials adjust for knee effusions. Why is this important? Look at the middle knee joint in the above diagram. Despite injecting high-dose PRP, you get the same low concentration of growth factors in the knee with a moderate to large effusion. So, not draining away the effusion before you inject the PRP creates a concentration problem. How common are joint effusions? VERY! Knee effusions are present in 90% of patients with knee OA, with 55% having a moderate or large effusion (6).
What does this mean for the existing published literature? We likely have clinical trials that have failed solely because of the lack of control over this one critical effusion variable.
The upshot? So, is injecting a low volume of highly concentrated PRP the same as injecting a larger volume of poorly concentrated PRP? NOPE. So, while the idea of a total platelet dose in a knee may have merit, we must be careful if that idea is taken to its extreme. At some point, the concentration of growth factors in that knee synovial fluid will drop below critical levels, and the clinical results will suffer.
_______________________________________________________________
References:
(1) Patel S, Gahlaut S, Thami T, Chouhan DK, Jain A, Dhillon MS. Comparison of Conventional Dose Versus Superdose Platelet-Rich Plasma for Knee Osteoarthritis: A Prospective, Triple-Blind, Randomized Clinical Trial. Orthop J Sports Med. 2024 Feb 26;12(2):23259671241227863. doi: 10.1177/23259671241227863. PMID: 38410168; PMCID: PMC10896053.
(2) Bansal, H., Leon, J., Pont, J.L. et al. Platelet-rich plasma (PRP) in osteoarthritis (OA) knee: Correct dose critical for long term clinical efficacy. Sci Rep 11, 3971 (2021). https://doi.org/10.1038/s41598-021-83025-2
(3) Berger DR, Centeno CJ, Steinmetz NJ. Platelet lysates from aged donors promote human tenocyte proliferation and migration in a concentration-dependent manner. Bone Joint Res. 2019 Feb 2;8(1):32-40. doi: 10.1302/2046-3758.81.BJR-2018-0164.R1. PMID: 30800297; PMCID: PMC6359887.
(4) Anitua E, Sánchez M, Zalduendo MM, de la Fuente M, Prado R, Orive G, Andía I. Fibroblastic response to treatment with different preparations rich in growth factors. Cell Prolif. 2009 Apr;42(2):162-70. doi: 10.1111/j.1365-2184.2009.00583.x. Epub 2009 Feb 24. PMID: 19250293; PMCID: PMC6496288.
(5) Jo CH, Kim JE, Yoon KS, Shin S. Platelet-rich plasma stimulates cell proliferation and enhances matrix gene expression and synthesis in tenocytes from human rotator cuff tendons with degenerative tears. Am J Sports Med. 2012 May;40(5):1035-45. doi: 10.1177/0363546512437525. Epub 2012 Feb 23. PMID: 22366517.
(6) Hill C.L., Gale D.G., Chaisson C.E., Skinner K., Kazis L., Gale M.E. Knee effusions, popliteal cysts, and synovial thickening: association with knee pain in osteoarthritis. J Rheumatol. 2001;28:1330–1337.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
