Riordan Medical Institute Review: Regrowing Lots of New Knee Cartilage?
A colleague just sent me a link to yet another amazing claim about treating knee arthritis, this time from the Riordan Medical Institute (RMI Clinic). In this case, the site claims to regrow up to 75% more knee cartilage. Is this real or hype? Let’s dive in.
The Cartilage Thickness Claim that Began this Review
A colleague this weekend sent me this statement from an RMI Clinic webpage:
“If you suffer from chronic knee pain due to arthritis or an old injury, or you’ve recently injured your knee meniscus, cartilage or ligaments (ACL, MCL) you may benefit from Stemnexa stem cell therapy.
Digging into What RMI Has Online
First, not too long ago, RMI was Riordan-McKenna Institute. Using the Internet Archive, the clinic begins around 2014, so they have been around for four years. At that point, it’s clearly the “Riordan-McKenna Institute.” In fact, as of about two weeks ago, orthopedic surgeon Wade Mckenna’s name and headshot were still on the website. However, the website now has a different name. It’s now called “Riordan Medical Clinic.” Hence, I will have to assume that Dr. McKenna is no longer involved.
From reviewing the website, the clinic uses bone marrow concentrate plus amniotic membrane. Hmmm…Unlike RMI, who has been using bone marrow stem cells for four years, we’ve used them longer than anyone else on earth to treat knee arthritis via injecting into joints (13 years). We’ve also used culture-expanded mesenchymal stem cells, fat stem cells, fat grafts, amnion, and many different types of platelet-derived and cytokine therapies. Have we ever observed anything that would allow us to back up the claim that most or even some patients should expect up to 75% cartilage regrowth? NO. That claim is misleading at best. Let me explain.
What’s Feasible in Stem Cell-Related Cartilage Repair and What’s Hype?
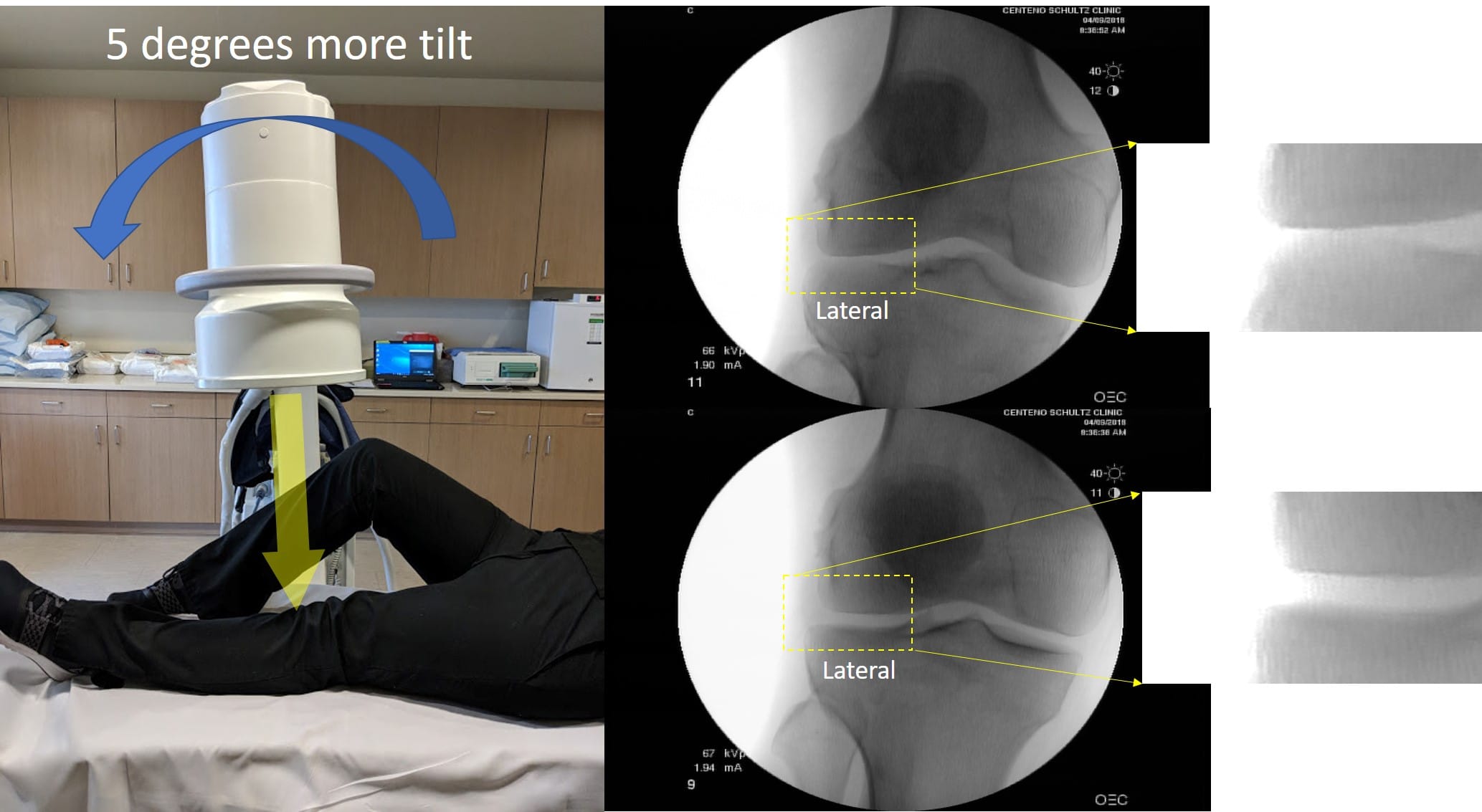
If you follow this blog, you know that we have many chiro clinics that are playing a game of hope and hype and preying on elderly people by promising to regrow new cartilage in severely arthritic knees. These clinics merely tilt the X-ray beam a bit to make it look like cartilage has grown, a simple-to-expose scam. See my pics below:
All I did here was to tilt the X-ray beam a few degrees, and, like magic, I can create and get rid of arthritis in seconds! Not really; it’s simply an X-ray trick.
However, the RMI claim also involves MRI? So what have we seen that’s possible in cartilage regeneration in the last almost decade and a half of doing this work? If you check out the video below, at around four minutes, you’ll see examples of MRI evidence of stem cell-mediated cartilage repair:
While we have seen some impressive results in filling in potholes and maybe a 25% increase in cartilage thickness in a very few patients, nothing would really fit with a patient with severe arthritis who reads the RMI statement about “up to 75% increase in cartilage thickness.” So to see if it’s possible to support that claim, we’ll have to dig deeper.
Maybe There Is Something Special About “Stemnexa”?
Could it be that RMI has developed something new and revolutionary? They call their stem cell treatment “Stemnexa.” Is this something that is able to regrow large stretches of new cartilage? Let’s explore that option.
Based on the website, “Stemnexa” is bone marrow concentrate (BMC) plus amniotic tissue. BMC is created by drawing bone marrow and then using a centrifuge to create various layers of cells. The middle layer (buffy coat) is then removed as this contains the stem cells. This is then called BMC.
So the first question we should ask is how the BMC is created. The RMI Clinic site says that it uses a “vertical axis centrifuge.” This is curious language, and given the statement about this on the RMI website exactly matches that on the Genius BMC system website, I can state with high confidence that RMI is advertising the use of a commercially available bedside system to create BMC.
If you read this site and blog, you know that I’m not a big fan of the little bedside machines, like the one being used here. By their very nature, we have seen that they are not the best way to isolate the stem cells from bone marrow. Why? Bone marrow samples differ from patient to patient; hence, no machine can deal with all of that variability. Hence, you tend to get a “one size fits all” product when compared to a physician who uses an onsite lab and scientifically validated protocols lab to pull out the stem cells by hand.
Could it be the amniotic membrane? The RMI Clinic website claims that by adding amniotic tissue to the stem cells, the patient’s cells dramatically improve. They show this image as proof (all RMI images used in this blog were obtained via fair use from their website):
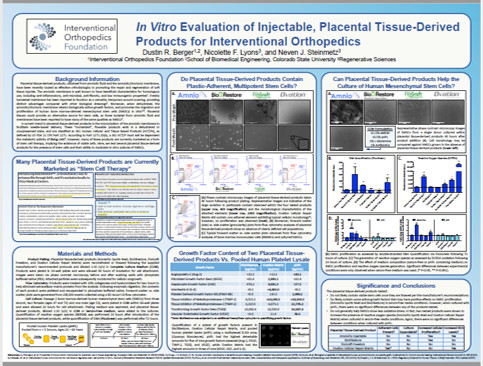
As a stem cell expert who has seen many different mesenchymal stem cells in culture, I can’t tell the difference. In addition, IOF and our lab team spent months working on a project of adding amniotic products to older stem cells to see if they could detect a difference across multiple different metrics. There was no improvement in the behavior or health of the cells (see the thumbnail of the research results below, and then click on it to see that full report):
Hence, our much more detailed tests demonstrated that adding in young amniotic and placental tissues didn’t help older stem cells.
Could It Be Something Else That’s Different?
Other variables to explore could be how the cells are placed. The RMI Clinic says that it uses a local orthopedic surgeon who uses fluoroscopy. I can’t see anything about using ultrasound. Given both would be required to perform high-level interventional orthopedics, this doesn’t seem to be the thing that’s likely to cause a knee to regrow large amounts of cartilage. In addition, as I have stated elsewhere, the average orthopedic surgeon would be far less skilled at image-guided injection therapy compared to someone trained in interventional orthopedics.
Is There Anything on the Website that Explains This 75% Cartilage Number?
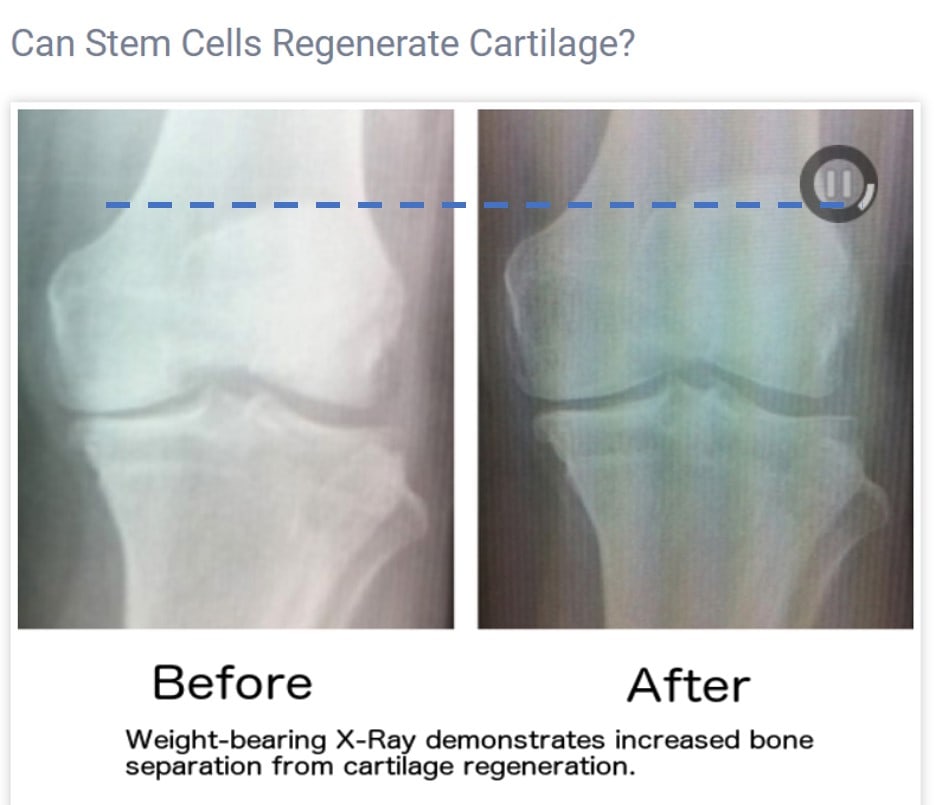
Under the knee page, there are two different image series shown. The first is an X-ray, see my discussion above. Like many X-rays placed on stem cell websites, this one claims that the increase in width of the knee joint is due to cartilage growth. I have copy/pasted this image from their website as it shows that joint space is different, but not for the reason suggested.
The position of the kneecap in the up-down position tells you about the angle of the X-ray beam relative to the knee. As I was able to show above, a small change in this angle can increase or decrease the joint-space width on the image. In this case, in order to see if the angles used for this picture were the same or different, I drew a dotted line from the top of the kneecap in one view (the left) and extended it to the right image. Regrettably, the position of the patella on the two X-ray images doesn’t match; hence, the angle of the beam here is obviously different between these before and after films. Hence, this image isn’t proof of any change in the joint-space width caused by cartilage regeneration, just proof of a poorly done X-ray.
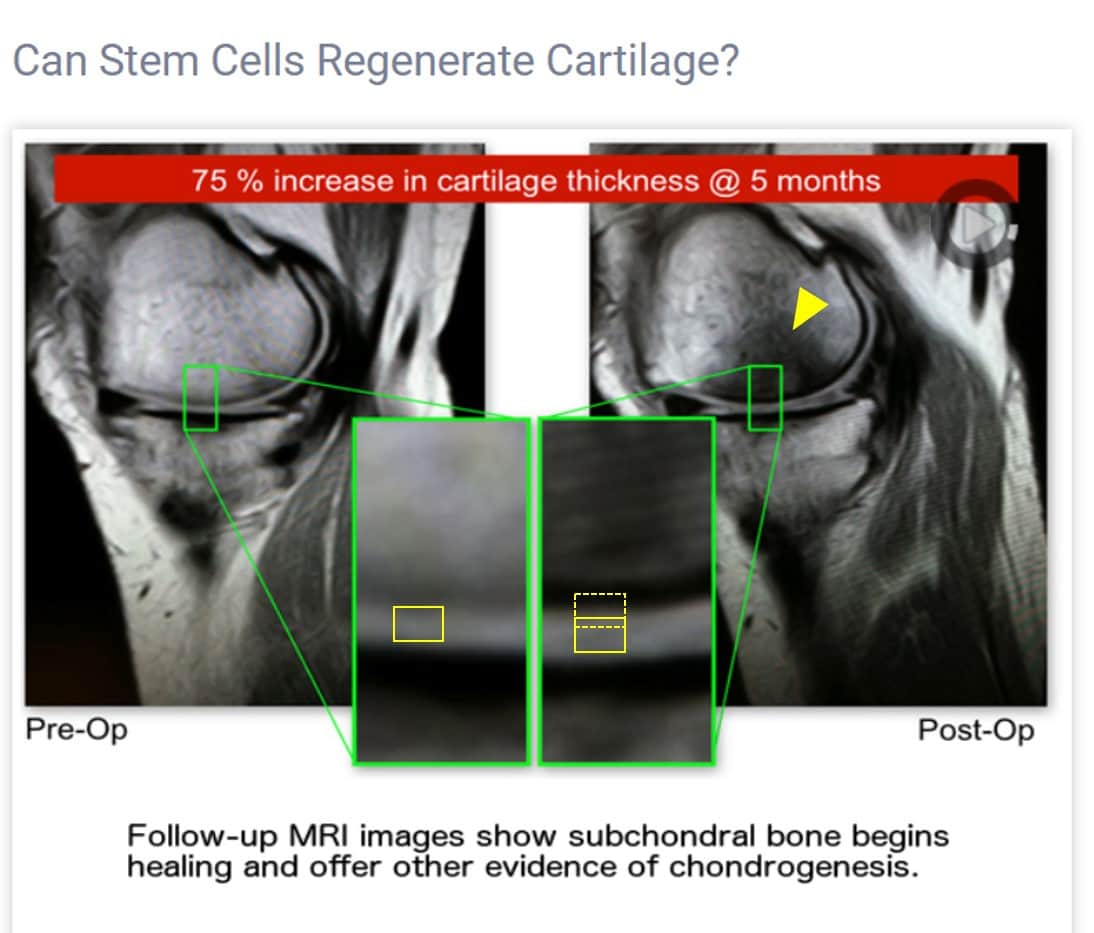
Next up is the MRI image on the website that seems to have started this 75% claim. It’s below:
First, this is an MRI side view (sagittal) of the knee. The bone is white, and the cartilage is gray. Second, regrettably, the before and after MRI are in different imaging planes. You can tell that based on the musculature of the calf, which is sliced differently between the before and after MRI. This can happen when the patient is loaded into the machine slightly askew or if the knee is a bit more rotated from one image to the other. Hence, this alone could change the apparent thickness of the cartilage without any cartilage regrowing. How is that possible?
Think about slicing a stick of butter and then measuring the height of each slice. If you sliced all of the butter at the exact same angle, your measurement of the height of each slice would match up. If not, then one slice may be taller. For example, check out the diagram I created below. The first slice (blue dashed lines) is straight up and down. The second slice (red dashed lines) is at an angle. The first blue slice is not going to be as tall as the red slice at an angle, despite the fact that the overall thickness of the stick of butter is the same for both slices.
Second, I then placed a yellow rectangle equivalent to the thickness of the cartilage on the left and copy/pasted that to the image to the right. As you can see, the thickness is pretty similar. I could maybe say that the thickness on the right is about 20–25% more, but the second box (dashed lines) on the right placed on top of the first box shows you how thick it would have to be if it were 75% more. In addition and perhaps most concerning is the appearance of new dark bone on the after image. I have this marked by the yellow arrowhead pointing at this area. Dark bone generally means dying bone; however, I would need to see more slices to be sure.
In summary, the two images shown don’t back up the 75% more cartilage claim. In fact, I must say that I’m a bit disappointed. I had hoped to at least see something that was more convincing to trained eyes.
The upshot? The claim of cartilage regeneration here is not well founded. In addition, the claim that BMC plus amnion is a game changer based on a simple look under the microscope is also not firmly anchored in science. In fact, we couldn’t prove that to ourselves with much more sophisticated testing. Hence, as I always say, it’s crazy out there folks…

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.