RFA Is Contraindicated in Cases of Spinal Instability
RFA is a technology that destroys nerves that carry pain signals from damaged joints in the back or neck. Despite its widespread use, there’s been an ongoing controversy regarding how it impacts muscular stability in the spine. Hence, it’s reasonable to ask whether RFA should be used when spinal instability is present. Let’s dive into that topic.
What Is RFA?
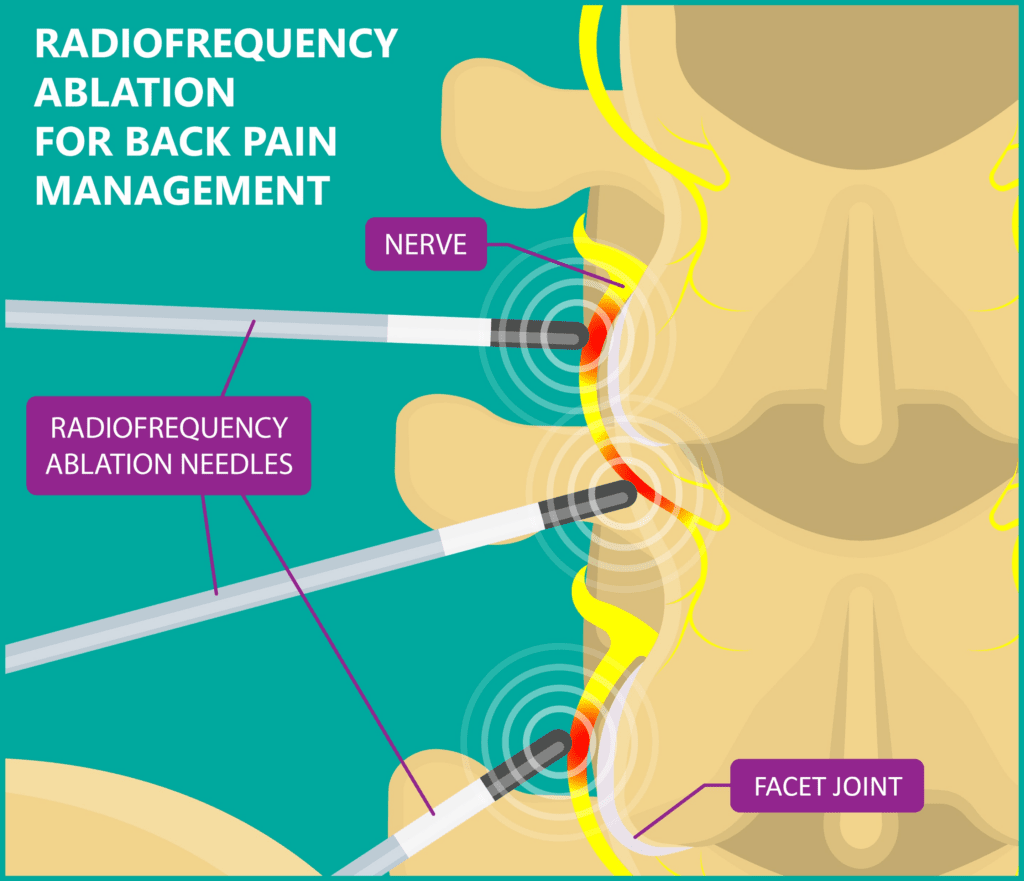
RFA involves inserting a large needle near the nerve that takes pain signals from a painful or damaged facet joint (“medial branch” of the sinuvertebral nerve). These small joints are found throughout the spine and can become damaged and painful due to arthritis or injury. The tip of the needle heats up, usually hot enough to cook tissue, and the doctor uses that energy to destroy the medial branch, which results in a block of those pain signals.
The good news is that this procedure has been shown to reduce neck and back pain caused by these painful facet joints. The bad news is that the ablated nerve also carries signals to control the small muscles that help stabilize the spine. These spinal stabilizers are called multifidi. Hence, nuking the nerve to these muscles likely results in muscular instability.
If we know that damaging the nerve that innervates critical spinal stabilizers is probably bad, then why is RFA so popular? It’s a great business plan. First, it reimburses more per unit time than simple spinal injections. Second, RFA wears off. Hence, it creates patients needing an RFA once every 6-18 months, which creates massive repeat business for the practice.
What Is Spinal Instability?
Your spine is like a stack of kids’ blocks stacked very high and is inherently unstable. Hence, there are two systems that keep it from falling apart: ligaments and muscles. The ligaments are passive stabilizers that prevent motion, like duct-taping the blocks together. The muscles are an active system that helps align the vertebrae with precision while moving. When either system fails, the spine becomes unstable, which can cause damage or long-term wear and tear on the facet joints, disc, and nerves, leading to pain.
What Is the Multifidus?
The multifidus muscles are small but crucial deep stabilizers within the spine that control one spinal level on another. These muscles are responsible for keeping the facet joints, discs, nerves, and other structures in the spine aligned with submillimeter precision as the body moves. For instance, when you reach for something, the multifidus muscles precontract by 100 milliseconds to prevent any displacement of the spinal structures.
Functioning multifidus muscles are critical for spinal health. When these muscles atrophy, back and leg pain can ensue (1-3). This is because atrophy of the multifidus muscles leads to increased wear and tear on the critical spine structures when the person moves, lifts, or twists. Unfortunately, most radiologists may not be aware of this connection, resulting in a lack of diagnosis for many patients with multifidus atrophy. For example, every day, I see patients who have severe multifidus atrophy who are told that their MRI results are normal.
To learn more about multifidus, please see my video below:
What Do We Know about RFA and Multifidus Atrophy?
Research on multifidus problems after RFA has been published (7). For example, we know that RFA reduces the ability of the multifidus to contract. For example, Dreyfus et al published a small 2009 case series that showed diffuse multifidus atrophy in patients after RFA with the radiologists reading the low back MRIs unable to discern which exact levels had been treated (5). Wu et al. also observed widespread multifidus atrophy following RFA and discussed the anatomical reason behind the more diffuse atrophy: the same medial branch innervated many multifidus levels (6). For more information, see my deep dive on RFA and multifidus atrophy.
The Spinal Intervention Society recently published a new analysis of this literature, which I read last week. It highlighted both findings, but it concluded that the literature wasn’t conclusive enough to know if multifidus atrophy was happening due to RFA. This educational white paper has since been pulled from SIS servers.
What Do We Know About RFA and Multifidus Function?
We know that, as expected, RFA reduces multifidus contraction (4). That’s because the medial branch, which is the target of the RFA, innervates the multifidus (8). We also know that multifidus dysfunction causes spinal instability and is a likely cause of low back pain (9-11).
Should Instability Be a Contraindication for RFA?
Regrettably, there isn’t much research on how RFA impacts spinal instability. I found only one study on this topic that involved just 15 patients who had slipped vertebrae (spondylolisthesis) followed for about two years (12). This research claimed no additional advancement of the slippage in these 15 patients beyond what would be expected, but the study had no control group that didn’t get RFA.
What should physicians recommend if there isn’t much research on RFA and spinal stability? Given that it’s clear that nuking the nerves that drive the multifidus spinal stabilizers reduces lumbar stability, why would we want to do this to a patient with an unstable spine? Hence, without more data, it’s pretty clear that RFA in a patient with known spinal instability would be contraindicated biomechanically.
Please Rule Out Spinal Instability BEFORE Offering a Patient RFA
Many years ago, we dropped RFA at our Colorado HQ clinic as a treatment offering. Why? While RFA did help patients with chronic neck and back pain, it also created lifetime patients who would endlessly return for more RFA. In addition, we also knew then that we were damaging spinal stability and likely making our patients worse over the long term. Since then, I have seen RFA be offered to patients with clear evidence of spinal instability. Many of these patients get worse due to RFA and then only later get a diagnosis of spinal instability through their own research. Sometimes this happens because the treating physician never took the time to work the patient up for instability and sometimes because of the hammer and nail effect. When all you have is a hammer (RFA), everything looks like a nail (RFA candidate).
The upshot? RFA can help patients with short to medium-term pain relief, but that relief likely comes at a cost. In the meantime, it’s pretty clear that biomechanically, it makes little sense to further destabilize a patient with instability by denervating the spinal stabilizers. Hence, if you’re a patient, please ask for a spinal instability work-up before anyone performs RFA on your spine. If you’re a physician, please take the time to rule out spinal stability before offering a patient RFA.
___________________________________________________________
References:
(1) Seyedhoseinpoor T, Taghipour M, Dadgoo M, Sanjari MA, Takamjani IE, Kazemnejad A, Khoshamooz Y, Hides J. Alteration of lumbar muscle morphology and composition in relation to low back pain: a systematic review and meta-analysis. Spine J. 2022 Apr;22(4):660-676. doi: 10.1016/j.spinee.2021.10.018. Epub 2021 Oct 27. PMID: 34718177.
(2) Kader DF, Wardlaw D, Smith FW. Correlation between the MRI changes in the lumbar multifidus muscles and leg pain. Clin Radiol. 2000 Feb;55(2):145-9. doi: 10.1053/crad.1999.0340. PMID: 10657162.
(3) Goubert D, De Pauw R, Meeus M, Willems T, Cagnie B, Schouppe S, Van Oosterwijck J, Dhondt E, Danneels L. Lumbar muscle structure and function in chronic versus recurrent low back pain: a cross-sectional study. Spine J. 2017 Sep;17(9):1285-1296. doi: 10.1016/j.spinee.2017.04.025. Epub 2017 Apr 26. PMID: 28456669.
(4) Kanchiku T, Imajo Y, Suzuki H, Yoshida Y, Nishida N, Taguchi T. Percutaneous radiofrequency facet joint denervation with monitoring of compound muscle action potential of the multifidus muscle group for treating chronic low back pain: a preliminary report. J Spinal Disord Tech. 2014 Oct;27(7):E262-7. doi: 10.1097/BSD.0000000000000107. PMID: 25137144.
(5) Dreyfuss P, Stout A, Aprill C, Pollei S, Johnson B, Bogduk N. The significance of multifidus atrophy after successful radiofrequency neurotomy for low back pain. PM R. 2009 Aug;1(8):719-22. doi: 10.1016/j.pmrj.2009.05.014. PMID: 19695523.
(6) Wu PB, Date ES, Kingery WS. The lumbar multifidus muscle in polysegmentally innervated. Electromyogr Clin Neurophysiol. 2000 Dec;40(8):483-5. PMID: 11155540.
(7) Smuck M, Crisostomo RA, Demirjian R, Fitch DS, Kennedy DJ, Geisser ME. Morphologic changes in the lumbar spine after lumbar medial branch radiofrequency neurotomy: a quantitative radiological study. Spine J. 2015 Jun 1;15(6):1415-21. doi: 10.1016/j.spinee.2013.06.096. Epub 2013 Nov 14. PMID: 24239488.
(8) Cawley DT, Alexander M, Morris S. Multifidus innervation and muscle assessment post-spinal surgery. Eur Spine J. 2014;23(2):320-327. doi:10.1007/s00586-013-2962-7
(9) Elfving B, Dedering A, Nemeth G. Lumbar muscle fatigue and recovery in patients with long-term low back trouble: Electromyography and health related factors. Clin Biomech. 2003;18:619–630.
(10) Gedalia U, Solomonow M, Zhou B, Baratta R, Lu Y, Harris M. Biomechanics of increased exposure to lumbar injury caused by cyclic loading. Part 2. Recovery of reflexive muscular stability with rest. Spine. 1999;24:2461–2467.
(11) Hodges P, Richardson C. Altered trunk muscle recruitment in people with low back pain with upper limb movement at different speeds. Arch Phys Med Rehabil. 1999;80:1005–1012.
(12) Patel T, Watterson C, McKenzie-Brown AM, Spektor B, Egan K, Boorman D. Lumbar Spondylolisthesis Progression: What is the Effect of Lumbar Medial Branch Nerve Radiofrequency Ablation on Lumbar Spondylolisthesis Progression? A Single-Center, Observational Study. J Pain Res. 2021 May 3;14:1193-1200. doi: 10.2147/JPR.S310238. PMID: 33976569; PMCID: PMC8104986.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
