Why You Don’t Need Shoulder Separation Surgery
On this page:
- What is the AC joint?
- What happens in an AC joint separation?
- What does an AC joint separation feel like?
- Is shoulder separation surgery necessary?
- New research on surgery for AC joint dislocation
When I was in medical school, I crashed a motorcycle and separated my shoulder. I was told back then that I could get surgery, but I didn’t do it. Why? I was concerned about shoulder separation surgery recovery time. Now, 30 years later, I’m glad I didn’t have the surgery. Now I feel vindicated that the latest research backs up my decision.
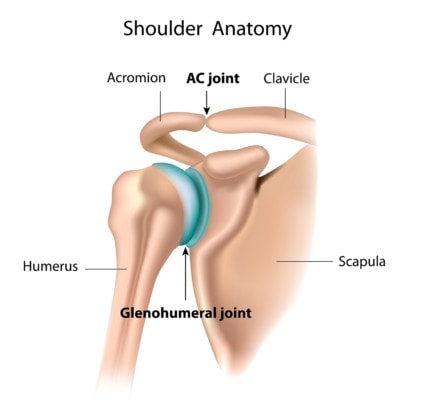
What Is the AC Joint?
The acromioclavicular (AC) joint is in the shoulder region. If you follow your collarbone (the clavicle) on the top of your shoulder, you’ll come to a prominence in the bone just before you reach the shoulder. This is your AC joint. As you pass over the AC joint, you will reach a shoulder bone called the acromion. So the joint is situated between the clavicle and acromion; hence, the acromioclavicular joint.
Alila Medical Media/Shutterstock
What Happens in an AC Joint Separation?
An AC joint separation is often referred to as a shoulder separation in casual conversation. This type of injury occurs when the clavicle is dislocated from the acromion. It’s a common injury for contact sports like football. It’s also important to note that there are different types of AC shoulder separations. Let’s take a look at the types.
- Grade I: slight joint displacement. This is where the acromioclavicular ligament may become partially torn or merely stretched. When you think of the typical shoulder separation injury, this is likely what first comes to mind.
- Grade II: partial joint dislocation. This injury results in the acromioclavicular ligament being torn completely, though the coracoclavicular ligament is still in good shape.
- Grade III: the joint is completely separated. Both ligaments (acromioclavicular and coracoclavicular) are torn. There’s usually visual evidence of a grade III separation with a bump suddenly appearing on the shoulder.
- Higher grades: grades IV-VI do exist, but they’re usually a result of a serious vehicle accident, so they’re not as common as the lower grades.
What Does an AC Joint Separation Feel Like?
Each grade of shoulder separation will have its own set of symptoms to look out for. In terms of the lowest grade, you would likely feel tenderness when your shoulder is touched. You’d also feel some minor pain when you moved your arm. At the same time, you can expect bruising around the shoulder.
Grade II ups the ante by introducing some moderate to severe pain around the shoulder. You may even experience some swelling in the area. Don’t be surprised if you can actually move your clavicle if you push on it (this isn’t recommended, by the way).
For a grade III injury, the symptoms become more serious. Pain will be severe even if you don’t move your arm. You may hear a popping sound if you do move the joint. You’ll see a noticeable shoulder deformity. And much of the time, the injured person will need to support the arm by the elbow, preventing further movement.
Diagnosing an AC joint separation is relatively straightforward. After reviewing the patient’s medical history, the doctor will ask the patient questions such as when the pain began, what they were doing at the time, what leads to more pain, and other important questions.
Then the doctor will examine the shoulder while assessing factors like range of motion, tenderness, strength, swelling, and more. Expect the doctor to perform tests around the joint, examining the structure of the bones and ligaments. The patient may even be asked to perform some routine activities that lead to the pain. The doctor will also take a closer look at the neck and back to see if those areas might play a role. This type of examination is usually done for lower grade shoulder separations since those of a higher grade are likely pretty obvious.
In many cases, the patient will likely get an x-ray to confirm the diagnosis. An x-ray can also help determine if you’re looking at a shoulder separation or a bone fracture.
Is Shoulder Separation Surgery Necessary?
As we can see, the AC joint can become dislocated or separated when it is injured, and while a dislocation sounds ominous, conservative measures and a lot of time are usually sufficient for healing. However, when high-grade dislocations occur, those that involve not just the bone but also tears in the ligaments, surgery is usually recommended.
The surgery for this condition usually involves bolting together the unstable joint. There are two problems with this approach. First, the joint is designed to give as you move and bolting it together gets rid of that normal joint flexibility. In addition, the shoulder separation surgery recovery time is not insignificant.
Another type of AC joint surgery is decompression. When the joint has arthritis, it can place pressure on the rotator cuff tendons underneath. To try and help this issue, surgeons will try to take off the bone spur. Take a look at my brief video below to see what an AC joint decompression surgery looks like:
So is AC joint surgery for a separated shoulder the right solution? One study suggests that even for the high-grade (levels III–V) dislocations, surgery may be no better than doing nothing. Let’s take a look.
New Research on Surgery for AC Joint Dislocation
The purpose of the new study was to investigate the outcomes for patients with high-grade acromioclavicular joint dislocation, comparing those who had surgery to those who did not (1). This means that they studied the worst patients. The ones who usually get offered surgery.
The new research paper was a meta-analysis consisting of 954 patients across 19 different studies. The results? Researchers found no clinically significant positive difference in the group that underwent surgery for their AC joint dislocation, and no differences were found in function between the two groups.
However, the group that opted for conservative management with no surgery were able to get back to work faster and had fewer complications and infections. This means that shoulder separation surgery recovery lagged behind, and included complications not experienced by the patients that did not have the surgery!
We can add this to the growing mound of orthopedic surgeries in which we have to ask, Why in the world are we doing this surgery? Other studies have also suggested surgery for AC joint dislocation is no better than no surgery, so this study adds further confirmation and adds to the burgeoning body of literature showing that so many orthopedic surgeries are unnecessary.
The Orthopedic Surgery Slide Continues
If you read this blog, you know that I’ve highlighted so many common orthopedic procedures that have been shown to be no better than fake surgery. Why? These surgeries never made much common sense in the first place.
For example, cutting out a piece of the knee meniscus shock absorber means that there is less cushion for the joint. Or fusing the spine just means that the levels above and below this area will sustain more force and cause these areas to break down more quickly.
The upshot? You don’t need surgery for even a high-grade AC joint separation. I’m a living testament to that fact, as 30+ years later I have no issues with heavy weight lifting. I’m so glad I didn’t have somebody bolt my shoulder joint together. Looks like if I did, I wouldn’t have benefitted and might have had some awful surgical complication!
__________________________________________________
References
(1) Chang N, Furey A, Kurdin A. Operative Versus Nonoperative Management of Acute High-Grade Acromioclavicular Dislocations: A Systematic Review and Meta-Analysis. J Orthop Trauma. 2018;32(1):1-9. doi:10.1097/BOT.0000000000001004

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
