Sitting and Sciatica Pain: How I Solved It With a Walk
On this page:
I’ve been at a medical conference lecturing all week, basically a sit fest. Despite trying to exercise every day and get up and move as much as feasible, my intermittent sciatica was singing last night at crazy new high levels. Thankfully I knew how to solve that problem, and as I walked it off, it hit me that most patients might not know that this can help or why it worked. Let me explain more about sitting and sciatica pain.
What Is Sciatica?
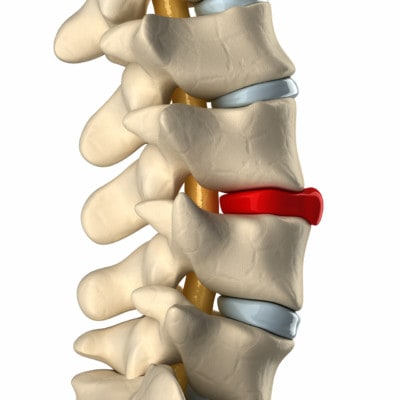
CLIPAREA/Custom Media/Shutterstock
You have discs in your back and nerves that exit each spinal level. When the spinal nerves get irritated by chemicals or pressure, they can get overly active, leading to a zinging pain down the leg (1). Where that nerve pain travels depends on which nerve is getting pinched or ramped up.
How Are Sitting and Sciatica Pain Related?
Sitting and sciatica pain are directly related through a mechanism that can best be described through a kids toy. The discs in your spine act as spacers and cushions between the spine bones. They are “viscoelastic,” meaning that they have the same properties as Silly Putty. Let’s explore that a bit.
Silly Putty can both act like rubber and be its opposite. Fling a piece of it at the wall and Silly Putty will bounce back like a rubber ball. However, place a book on a chunk of the stuff and leave it there for an hour and it flattens out. This is called viscoelastic. Your discs in the back are the same.
Unlike Silly Putty, your discs have water inside them and specialized natural chemicals called glycosaminoglycans (GAGs). Sitting a long time pushes the water out of the discs, causing them to flatten a bit. This effect is magnified as we age because the cells in damaged or degenerated discs don’t produce as much GAG.
This results in less water in the disc, so when you sit, that lower amount of water is easily pushed out and the disc flattens (2). When this happens it bulges a bit and can place pressure on a spinal nerve, causing that zinging feeling down a leg.
How Does Walking Help Sciatica Pain?
Yesterday afternoon, as I stood in the lecture hall speaking with physicians, the outside of my left leg was zinging in a pulsing fashion that felt like a new electrical heartbeat in the outside and back of my left leg. As a physician, I knew that this was caused by my left S1 spinal nerve. My first natural instinct was to lay down, but I instantly knew what I should do—go for a walk. Why?
Sitting and sciatica pain can be solved by understanding that a degenerated disc gets its nutrition by soaking up water through a process called “imbibition.” The disc literally “imbibes” water by repetitive pressure. Each time you step, a little water gets pushed out of the disc, but as the disc rebounds from the pressure, it soaks up a bit more water than it sheds. Hence this pumping action rehydrates the disc and reduces the flattening effect that causes the bulge and nerve pressure.
Did it work? Yep, within a few minutes of taking a brisk walk, my left-leg zinging pain went completely away! It was really amazingly effective. On the other hand, had I lain down, the disc would not have fully recovered its water nearly as quickly. I would have been stuck in a vicious cycle of the disc losing more and more water with additional sitting that day.
The upshot? The discs in your back need to imbibe water by the pumping action of walking. So when sitting causes that nerve zinging down one or both legs, resist your natural instinct to lie down, and walk it off instead (3)!
__________________________________________________
References
(1) Koes BW, van Tulder MW, Peul WC. Diagnosis and treatment of sciatica. BMJ. 2007;334(7607):1313-1317. doi:10.1136/bmj.39223.428495.BE
(2) Lis AM, Black KM, Korn H, Nordin M. Association between sitting and occupational LBP. Eur Spine J. 2007;16(2):283-298. doi:10.1007/s00586-006-0143-7
(3) Shiri R, Euro U, Heliövaara M, et al. Lifestyle Risk Factors Increase the Risk of Hospitalization for Sciatica: Findings of Four Prospective Cohort Studies. Am J Med. 2017;130(12):1408-1414.e6. doi:10.1016/j.amjmed.2017.06.027

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
