Sternoclavicular Joint Pain And Its Possible Causes

Medically Reviewed By:
Pain in the sternoclavicular (SC) joint can disrupt everyday movements and limit upper body function. This joint plays a key role in shoulder motion and helps stabilize the upper body. Discomfort in this area may make it harder to lift, reach, or rotate the arm, especially during overhead movements or when carrying weight.
This article examines the structure and function of the SC joint, explores potential sources of pain, and outlines diagnostic approaches. It also reviews available strategies, including procedures using Regenexx lab processes, that may help address symptoms and support improved mobility.
The Sternoclavicular Joint And Its Role In Arm And Shoulder Mobility
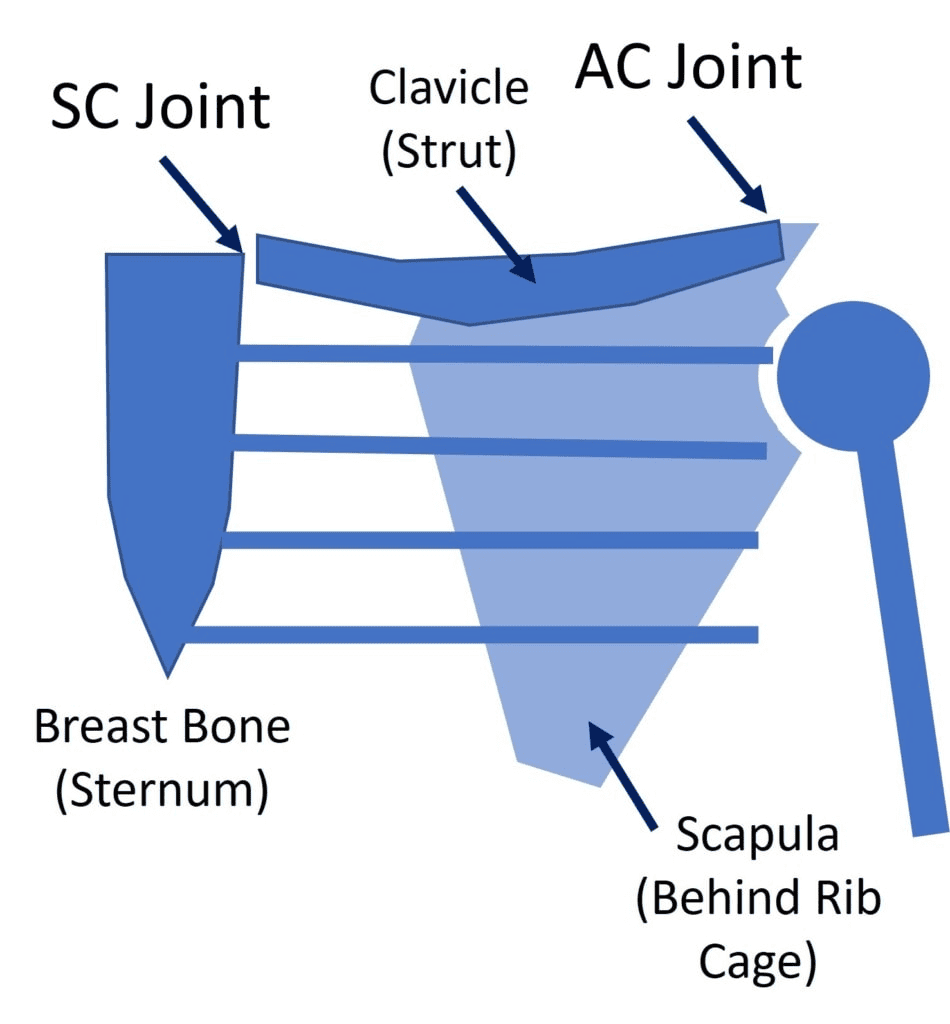
The SC joint forms the connection between the upper chest and the shoulder. This small joint, where the collarbone (clavicle) meets the breastbone (sternum), plays a vital role in linking the arm to the rest of the body. Although it’s roughly the size of a large thumb joint, it contributes significantly to upper body movement and stability.
Credit: Wikipedia
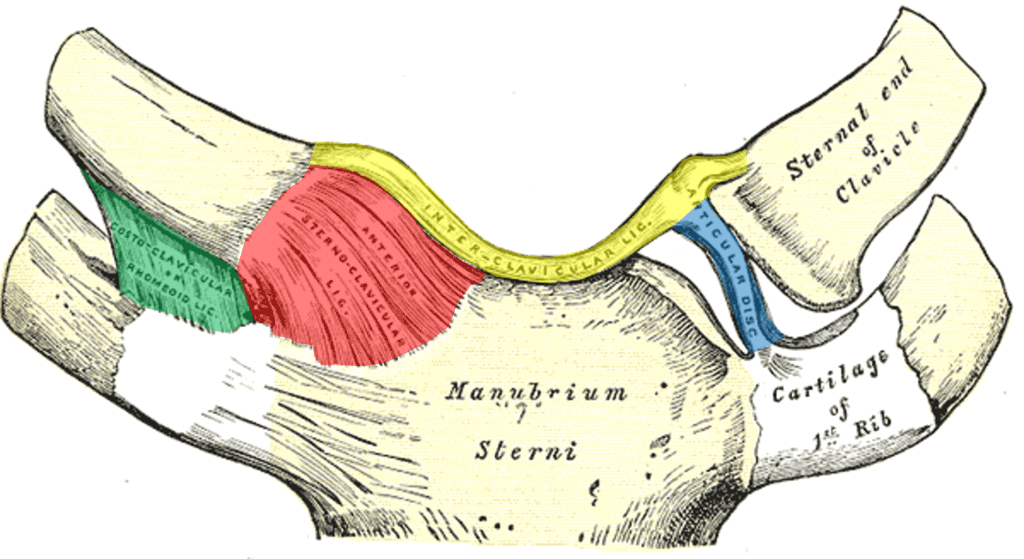
Layers of cartilage and strong ligaments support the SC joint. Cartilage at the ends of the clavicle and sternum helps cushion movement, while a fibrous disc within the joint adds support and absorbs shock. Together, these structures help the joint manage both movement and the transfer of force between the arm and the upper body.
Several key ligaments help stabilize and guide movement in the SC joint:
- Interclavicular ligament (yellow): Connects the two clavicles across the top of the joint and helps stabilize the upper chest.
- Anterior sternoclavicular ligament (red): Helps prevent the clavicle from shifting forward.
- Costoclavicular (rhomboid) ligament (green): Anchors the clavicle to the first rib and helps regulate its motion.
The SC joint serves as the foundational link in a chain that includes the acromioclavicular (AC) joint and the scapula. Together, these structures create a mechanical system that coordinates movement across the chest, shoulder, and arm. This system supports common actions like reaching, pushing, and lifting.
When inflammation, injury, or joint instability disrupts this area, it can affect the entire shoulder complex. A clear understanding of the SC joint’s structure helps explain why pain may develop here and how it may impact upper body function.
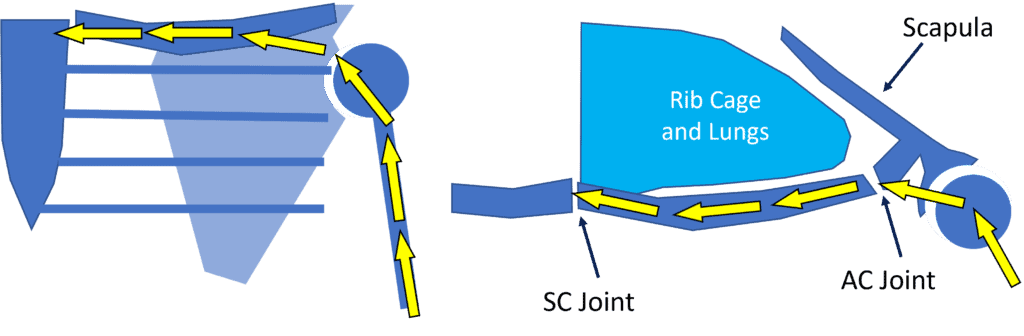
The SC and AC joints work together to transfer forces from the arm through the shoulder and into the sternum. This joint system acts like a structural support, guiding and stabilizing movement, similar to how a suspension system distributes force in a vehicle. When functioning properly, it helps manage physical stress during activities such as lifting, reaching, or pushing.
Pain in the SC joint often becomes noticeable during these same movements, especially when picking up or carrying objects.
Understanding The Pain In The Sternoclavicular Joint
Pain in the SC joint may develop after trauma to the shoulder or upper chest. In other cases, it can emerge gradually as the joint wears down, potentially leading to degenerative changes such as arthritis. Discomfort often appears near the base of the neck, directly over the joint—but symptoms don’t always stay in that area.
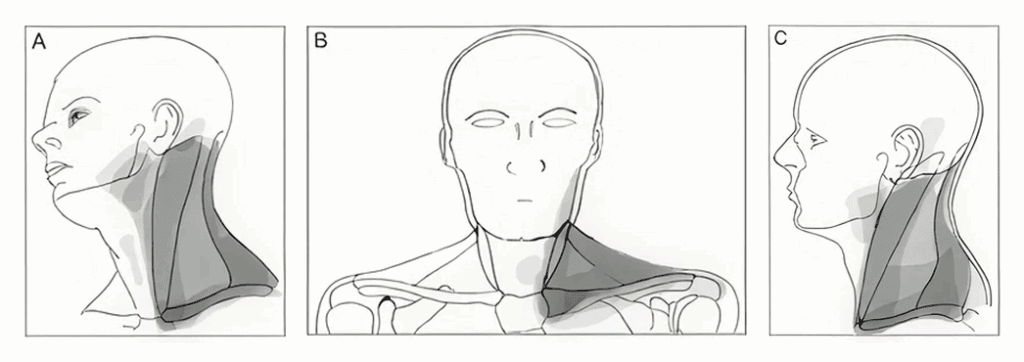
In some individuals, SC joint pain may refer to nearby regions such as the side of the neck or the upper trapezius muscle. These referred pain patterns can make it harder to pinpoint the source of discomfort without a thorough evaluation by a physician.
Movements involving lifting, pulling, or pushing often trigger or worsen symptoms. Some individuals may also notice swelling, tenderness, or a sense of instability in the joint during activity.
Recognizing The Associated Signs And Symptoms
Issues in the SC joint often involve more than just localized pain. A range of signs and symptoms may appear, particularly when inflammation or instability affects the joint. These symptoms typically emerge during arm movement or after physical activity.
- Sharp or aching pain: May begin suddenly or develop over time, usually felt near the collarbone or the base of the neck.
- Swelling and tenderness: The joint may look slightly enlarged or feel sore when touched.
- Warmth around the joint: In some cases, the skin over the joint may feel warm, which can indicate inflammation.
- Limited shoulder or arm movement: Irritation in the joint may make it harder to lift, reach, or rotate the arm without discomfort.
Symptom intensity may vary based on activity level, the underlying cause, or the progression of joint changes.
Potential Causes Of Pain In The SC Joints
Pain in the SC joint can stem from a variety of mechanical or inflammatory factors. Because this joint helps transfer force between the arm and the trunk, it remains vulnerable to sudden injury and ongoing stress. In some individuals, underlying conditions may also affect symptom development.
Common potential causes include:
Trauma And Injuries
A direct impact to the shoulder or chest can place significant stress on the SC joint. Falls, contact sports, or collisions—such as those that occur during motor vehicle accidents—often contribute to these injuries. Such trauma may lead to ligament sprains, joint dislocations, or minor fractures involving the clavicle or sternum.
Infections
Although uncommon, infections can affect the SC joint. An infection may lead to rapid swelling, warmth, and pronounced tenderness over the joint. Redness and fever may also develop. In most cases, bacteria reach the joint through the bloodstream or enter following a medical procedure or injury.
Repetitive Stress Or Overuse
Frequent or prolonged use of the upper limbs—especially during overhead lifting, pushing, or pulling—can place ongoing strain on the SC joint. Repetitive loading may irritate the joint surfaces and surrounding ligaments, leading to discomfort that builds gradually over time.
Ehlers-Danlos Syndrome (EDS): EDS is a group of connective tissue disorders that affect skin, joints, and blood vessels. It may cause joint hypermobility, skin fragility, and chronic pain, increasing the risk of injuries and joint instability. Symptoms vary based on the type of EDS. Read more About Ehlers-Danlos Syndrome.
Diagnosing Sternoclavicular Joint Discomfort
Identifying the source of pain in the SC joint requires a detailed clinical evaluation. Because symptoms can resemble those of other shoulder or neck conditions, a comprehensive assessment helps ensure the appropriate area receives attention. Physicians often use multiple methods to examine the joint and nearby structures.
Common diagnostic steps include:
- Hands-on evaluation: A physical exam plays a key role in assessing SC joint discomfort. This includes:
- Palpation: Applying gentle pressure to the joint helps detect tenderness, swelling, or localized pain.
- Movement assessment: Physicians observe how the joint functions during shoulder and arm motion to identify any limitations or irregularities.
- Stability testing: Specific maneuvers apply pressure to test for excessive joint movement, which may indicate ligament injury or laxity.
- Imaging tests: Diagnostic imaging can help confirm structural concerns, although certain types of instability may not appear on static scans.
- X-ray: X-ray may show changes in joint spacing or bone injury but offers limited detail for small joints like the SC joint.
- CT scan: CT scans provide clear images of bone structure and joint alignment, useful for detecting fractures or dislocations.
- MRI: MRI helps visualize soft tissues such as cartilage, ligaments, or signs of inflammation.
- Ultrasound: Allows real-time imaging during joint movement and may reveal instability or swelling not captured by other imaging methods.
Conventional Treatment Options For Discomfort In The SC Joint
Treatment for SC joint discomfort often starts with conservative approaches designed to reduce symptoms and support improved mobility. These methods are commonly used when symptoms appear mild to moderate or during the early stages of joint irritation.
Physical Therapy
Physical therapy may help manage SC joint discomfort, particularly when movement patterns or joint mechanics contribute to symptoms. A trained physical therapist can assess how the SC joint functions in coordination with the shoulder and upper body, identifying imbalances or areas of dysfunction.
Treatment strategies may include gentle joint mobilization, posture training, and targeted exercises to strengthen the rotator cuff and scapular stabilizers. These techniques aim to support the joint, reduce mechanical stress, and improve shoulder function over time.
Steroid Injections
Corticosteroid injections may help manage inflammation in the SC joint. This approach can temporarily reduce symptoms, particularly when swelling is a prominent concern.
However, studies have shown that repeated or high-dose steroid use may accelerate cartilage breakdown and contribute to joint degeneration. Because of these potential risks, physicians typically reserve this option for cases where other conservative treatments have not provided symptom relief.
Sternoclavicular Joint Reconstruction
Surgical reconstruction of the SC joint may be considered in rare cases when symptoms remain severe, and other treatments have not provided relief. This option is typically reserved for individuals with marked instability or structural damage that affects joint function.
During the procedure, a surgeon creates small tunnels in the bones near the joint and threads a tendon graft through them. The graft helps replicate the function of injured ligaments, restoring joint stability and reducing abnormal movement.
Although surgery can address specific mechanical problems, most individuals with SC joint discomfort respond well to less invasive treatment strategies and do not require surgical reconstruction.
How Procedures Using Regenexx Injectates May Help Address SC Joint Pain
When physical therapy and other conservative options do not provide relief from SC joint discomfort, image-guided interventional orthobiologic procedures may offer a next-step option. These procedures use the body’s own biological materials to help support joint health and improve function.
Ultrasound guidance plays a key role in accurately placing injectates into the SC joint and surrounding ligaments. This targeted approach allows physicians in the licensed Regenexx network to address the structures responsible for joint stability and motion control.
Procedures using Regenexx injectates may involve:
- Platelet-rich plasma (PRP) injections: A concentrated preparation of platelets derived from the individual’s own blood. These platelets release growth factors that may support tissue repair and reduce joint-related symptoms.
- Platelet lysate (PL): A growth factor-rich formulation created from PRP. This injectate may be selected when a more focused anti-inflammatory effect is desired.
These image-guided procedures aim to reduce discomfort and improve joint stability—particularly when ligament-related instability contributes to abnormal mechanics in the SC joint.
Regenexx lab processing supports customized doses that are more concentrated than bedside systems, and routinely achieves 20x concentration of stem cell-containing bone marrow, far above what non-Regenexx providers achieve. Each treatment is prepared for the specific joint and tissue involved.
Tips To Prevent Sternoclavicular Joint Pain From Worsening
Simple adjustments to posture and movement can help prevent further irritation or injury to the SC joint. These strategies may reduce mechanical stress and support joint health over time:
- Maintain proper posture: Promote joint alignment during sitting, standing, and daily activities.
- Avoid repetitive overhead or heavy lifting motions: Reduce strain by modifying tasks that place a high mechanical load on the shoulder.
- Use ergonomic equipment: Support joint positioning during work or household tasks with well-designed tools and setups.
- Engage in regular stretching and strengthening: Focus on shoulder mobility and muscle control to help stabilize the SC joint.
- Warm up before physical activity: Prepare muscles and joints to reduce the chance of strain or irritation.
- Modify activity if discomfort develops: Temporary changes in routine may help limit further joint stress.
- Address shoulder or neck issues early: Managing nearby joint dysfunction may prevent compensation and added stress at the SC joint.
- Use proper lifting techniques: Engage core muscles and move in a controlled manner during strenuous activity.
Explore Non-Surgical Options For SC Joint Pain Management With Regenexx
SC joint pain is often overlooked during clinical evaluations, yet it can significantly affect shoulder function and daily activity. Non-surgical strategies—including targeted physical therapy and image-guided interventional orthobiologic procedures—may offer effective options for managing symptoms.
Procedures using Regenexx injectates rely on customized platelet-based formulations designed to support joint stability and improve function. These approaches aim to reduce discomfort and promote better movement control, without the need for surgery or long-term medication use.
Surgical reconstruction is rarely required and typically reserved for the most complex cases. For many individuals, conservative care combined with the non-surgical procedures available through the Regenexx network may offer meaningful relief and help joint function.
Get started to see if you are a Regenexx candidate
To talk one-on-one with one of our team members about how the Regenexx approach may be able to help your orthopedic pain or injury, please complete the form below and we will be in touch with you within the next business day.

Medically Reviewed By:
