The Morality Test of Platelet-Rich Plasma vs Corticosteroids

Credit: Shutterstock
IMHO corticosteroid use in knee arthritis has become a giant medical morality test. We know the stuff is toxic, but physicians can’t help themselves from injecting it because it’s covered by insurance companies. Now that PRP is here and known to be effective, this sets up an interesting duality as there is now a better alternative that isn’t yet covered by insurance. So let’s review the data showing that PRP is superior to steroid shots and why this sets up an interesting test of your doctor’s ethics.
At Least Do No Harm
“If you can do no good, at least do no harm.” This statement is often attributed to the Hippocratic Oath and the Latin phrase “Primum non nocere” or “first do no harm”. While the idea was not in the actual oath, it was in other writings by Hippocrates. It also appeared in a book that was published in the mid-1800s about medical education (1). The idea is simple, it’s the doctor’s job to help protect the patient.
All medical care carries risk and managing that risk is essential. Hopefully, the benefits outweigh the risks, or at least the patient understands and accepts the risks and makes the choice to accept them. However, steroid shots present an interesting challenge to this sacred tenant of medicine.
Steroid Shots to Treat Pain are Really Bad for Patients
Doctors use steroids in medical treatment like priests use holy water. While there are clinical situations where they can be life-saving, their use to treat pain has grown increasingly controversial as our understanding of the nasty side effects has mounted:
- 3 days of oral steroid use results in an 80% increase in GI bleeds and a doubling of the heart failure and sepsis risk (2).
- More than 30 days of oral use results in a 5X risk for sepsis, 3X increase in the risk of blood clots, and 20X for fractures (3).
- These drugs both injure stem cells and cartilage cells, including documented loss of cartilage in the knee joint (4-6).
- There is an increased risk of infection in a knee or hip replacement or meniscectomy surgery when steroids are injected into that joint before the procedure (7-10).
- Inhaled steroid use in asthma is now associated with brain atrophy (11).
- Steroid injections in tendons reduce blood supply, injure tendon cells, and increase rotator cuff repair failure rates (12-14).
- Injections of steroids for pain worsen osteoporosis, cortisol levels, and blood sugar (15-17).
The Ethical Calculus Behind PRP
If all you had to offer the patient was a steroid shot and this usually worked to decrease the patient’s pain, as long as the patient understood the risks and accepted those, then a physician would be medically justified in providing this treatment. However, there are two problems with that statement:
- There is a better alternative
- Patients are almost never told the risks of getting the steroid shot
So let’s begin with the first concept, that PRP beats corticosteroids for a common problem like knee osteoarthritis.
PRP vs Corticosteroid for Knee Arthritis
There are a huge number of randomized controlled trials that have been performed with the final conclusion being that properly concentrated PRP works to help knee arthritis symptoms. This diagram is from the last analysis I did showing that the amount of data in the “Pro” PRP camp swamped any negative trial results due to low concentration fake “PRP”:
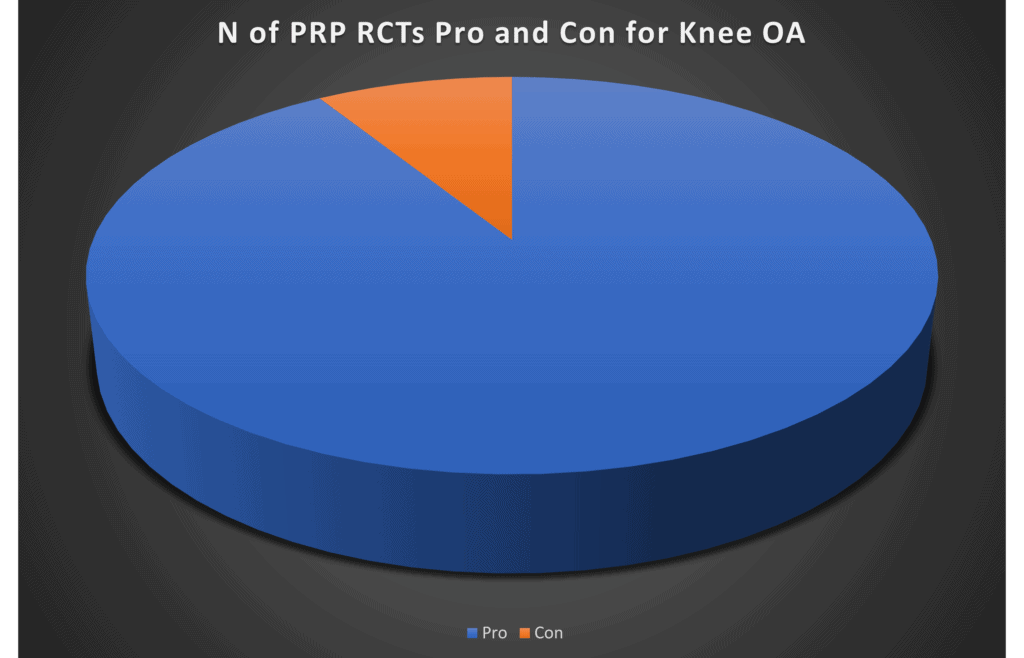
In addition, PRP has been compared head-to-head to steroid shots in the treatment of knee arthritis (18-23). In 4 of the 6 randomized controlled trials, PRP was superior to steroid at 6 months or more. In two RCTs it was equivalent. In addition, to date, no study has shown the same type of negative side effects for PRP that we know steroids exhibit.
Is Using a Steroid Injection Over PRP a Violation of “First Do No Harm”?
If we stay on the use case of knee arthritis, here’s what we know:
- Steroids have serious and wide-reaching negative side effects
- PRP is superior to or at least as good as a steroid shot without any of these known side effects
Hence, IMHO offering a patient a steroid shot for knee arthritis and not offering PRP without a discussion of the possible side effects of the steroid violates the “first do no harm” rule. If that’s true, why does this happen thousands of times each day in the United States?
The Insurance Morality Test
Right now, outside of the Regenexx network and the companies that have decided to offer their employees PRP, there is no insurance coverage for PRP to treat knee arthritis. There is coverage to use a steroid injection. Hence, this becomes a morality test of sorts. Will a doctor take the time to offer the superior non-covered option? Will they explain the benefits and risks of both? If the patient chooses the steroid, will the doctor explain the risks of that choice?
Why are physicians still offering steroids? The biggest excuse I hear is “because it’s covered”. Or “my patients don’t want to hear about things their insurance won’t cover”. However, is that really true? With the average co-pay and deductible hitting thousands of dollars, they are in fact, paying cash for either the steroid injection or a PRP shot.
The upshot? IMHO data on steroids and PRP is such that we either need to have physicians stop offering steroid shots or at least use expanded informed consent when they do. It’s also time to stop using the excuse, “because it’s covered” and begin paying attention to “Primum non nocere”.
_________________________________________________
References:
(1) Primum non nocere. (2021, October 30). In Wikipedia. https://en.wikipedia.org/wiki/Primum_non_nocere
(2) Yao TC, Huang YW, Chang SM, Tsai SY, Wu AC, Tsai HJ. Association Between Oral Corticosteroid Bursts and Severe Adverse Events: A Nationwide Population-Based Cohort Study [published online ahead of print, 2020 Jul 7]. Ann Intern Med. 2020;10.7326/M20-0432. doi:10.7326/M20-0432
(3) Waljee AK, Rogers MA, Lin P, et al. Short term use of oral corticosteroids and related harms among adults in the United States: population based cohort study. BMJ. 2017;357:j1415. Published 2017 Apr 12. doi:10.1136/bmj.j1415
(4) Wyles CC, Houdek MT, Wyles SP, Wagner ER, Behfar A, Sierra RJ. Differential cytotoxicity of corticosteroids on human mesenchymal stem cells. Clin Orthop Relat Res. 2015 Mar;473(3):1155-64. doi: 10.1007/s11999-014-3925-y. Epub 2014 Sep 4. PMID: 25187334; PMCID: PMC4317436.
(5) Dragoo JL, Danial CM, Braun HJ, Pouliot MA, Kim HJ. The chondrotoxicity of single-dose corticosteroids. Knee Surg Sports Traumatol Arthrosc. 2012 Sep;20(9):1809-14. doi: 10.1007/s00167-011-1820-6. Epub 2011 Dec 21. PMID: 22186921.
(6) McAlindon TE, LaValley MP, Harvey WF, et al. Effect of Intra-articular Triamcinolone vs Saline on Knee Cartilage Volume and Pain in Patients With Knee Osteoarthritis: A Randomized Clinical Trial. JAMA.2017;317(19):1967–1975. doi: 10.1001/jama.2017.5283
(7) Wijn SRW, Rovers MM, van Tienen TG, Hannink G. Intra-articular corticosteroid injections increase the risk of requiring knee arthroplasty. Bone Joint J. 2020 May;102-B(5):586-592. doi: 10.1302/0301-620X.
(8) Richardson SS, Schairer WW, Sculco TP, Sculco PK. Comparison of Infection Risk with Corticosteroid or Hyaluronic Acid Injection Prior to Total Knee Arthroplasty. J Bone Joint Surg Am. 2019 Jan 16;101(2):112-118. doi: 10.2106/JBJS.18.00454.
(9) Ravi B, Escott BG, Wasserstein D, Croxford R, Hollands S, Paterson JM, Kreder HJ, Hawker GA. Intraarticular hip injection and early revision surgery following total hip arthroplasty: a retrospective cohort study. Arthritis Rheumatol. 2015 Jan;67(1):162-8. doi: 10.1002/art.38886.
(10) Forsythe B, Forlenza EM, Agarwalla A, Cohn MR, Lavoie-Gagne O, Lu Y, Mascarenhas R. Corticosteroid Injections One Month Before Arthroscopic Meniscectomy Increase the Risk of Surgical Site Infection. Arthroscopy. 2021 Mar 31:S0749-8063(21)00289-9. doi: 10.1016/j.arthro.2021.02.047. Epub ahead of print. PMID: 33812029.
(11) van der Meulen M, Amaya JM, Dekkers OM, et alAssociation between use of systemic and inhaled glucocorticoids and changes in brain volume and white matter microstructure: a cross-sectional study using data from the UK BiobankBMJ Open 2022;12:e062446. doi: 10.1136/bmjopen-2022-062446
(12) Bonnevialle N, Bayle X, Projetti F, Wargny M, Gomez-Brouchet A, Mansat P. Variations of the micro-vascularization of the greater tuberosity in patients with rotator cuff tears. Int Orthop. 2015;39(2):371‐376. doi:10.1007/s00264-014-2628-z
(13) Dean BJ, Franklin SL, Murphy RJ, Javaid MK, Carr AJ. Glucocorticoids induce specific ion-channel-mediated toxicity in human rotator cuff tendon: a mechanism underpinning the ultimately deleterious effect of steroid injection in tendinopathy?. Br J Sports Med. 2014;48(22):1620‐1626. doi:10.1136/bjsports-2013-093178
(14) Cimino AM, Veazey GC, McMurtrie JT, et al. The Effect of Corticosteroid Injections on Clinical Outcomes and Failure Rates after Rotator Cuff Repair: A Systematic Review [published online ahead of print, 2020 May 7]. Arthroscopy. 2020;S0749-8063(20)30379-0. doi:10.1016/j.arthro.2020.04.044
(15) Kang SS, Hwang BM, Son H, Cheong IY, Lee SJ, Chung TY. Changes in bone mineral density in postmenopausal women treated with epidural steroid injections for lower back pain. Pain Physician. 2012 May-Jun;15(3):229-36.
(16) Chon JY, Moon HS. Salivary cortisol concentration changes after epidural steroid injection. Pain Physician. 2012 Nov-Dec;15(6):461-6.
(17) Habib GS. Systemic effects of intra-articular corticosteroids. Clin Rheumatol. 2009;28(7):749‐756. doi:10.1007/s10067-009-1135-x
(18) Camurcu Y, Sofu H, Ucpunar H, Kockara N, Cobden A, Duman S. Single-dose intra-articular corticosteroid injection prior to platelet-rich plasma injection resulted in better clinical outcomes in patients with knee osteoarthritis: A pilot study. J Back Musculoskelet Rehabil. 2018;31(4):603-610. doi: 10.3233/BMR-171066. PMID: 29710676.
(19) Uslu Güvendi E, Aşkin A, Güvendi G, Koçyiğit H. Comparison of Efficiency Between Corticosteroid and Platelet Rich Plasma Injection Therapies in Patients With Knee Osteoarthritis. Arch Rheumatol. 2017 Nov 2;33(3):273-281. doi: 10.5606/ArchRheumatol.2018.6608. PMID: 30632533; PMCID: PMC6328223.
(20) Joshi Jubert N, Rodríguez L, Reverté-Vinaixa MM, Navarro A. Platelet-Rich Plasma Injections for Advanced Knee Osteoarthritis: A Prospective, Randomized, Double-Blinded Clinical Trial. Orthop J Sports Med. 2017 Feb 13;5(2):2325967116689386. doi: 10.1177/2325967116689386. PMID: 28255569; PMCID: PMC5315239.
(21) Freire MRM, da Silva PMC, Azevedo AR, Silva DS, da Silva RBB, Cardoso JC. Comparative Effect between Infiltration of Platelet-rich Plasma and the Use of Corticosteroids in the Treatment of Knee Osteoarthritis: A Prospective and Randomized Clinical Trial. Rev Bras Ortop (Sao Paulo). 2020 Oct;55(5):551-556. doi: 10.1016/j.rbo.2018.01.001. Epub 2020 Feb 3. PMID: 33093718; PMCID: PMC7575359.
(22) Elksniņš-Finogejevs A, Vidal L, Peredistijs A. Intra-articular platelet-rich plasma vs corticosteroids in the treatment of moderate knee osteoarthritis: a single-center prospective randomized controlled study with a 1-year follow up. J Orthop Surg Res. 2020 Jul 10;15(1):257. doi: 10.1186/s13018-020-01753-z. PMID: 32650801; PMCID: PMC7353717.
(23) Pretorius J, Nemat N, Alsayed A, Mustafa A, Hammad Y, Shaju T, Nadeem S. Double-Blind Randomized Controlled Trial Comparing Platelet-Rich Plasma With Intra-Articular Corticosteroid Injections in Patients With Bilateral Knee Osteoarthritis. Cureus. 2022 Sep 29;14(9):e29744. doi: 10.7759/cureus.29744. PMID: 36324362; PMCID: PMC9617571.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
