The Use of Botox to Treat TMJ: Why This Is Yet Another Bad Idea

Credit: Shutterstock
A family member has TMJ and I learned recently that they were hit up by a dentist to inject Botox to cure the problem. I promised a blog deep dive into why this wasn’t a good idea and on whether the data exists to back up that claim. Let’s dig in.
What is Botox?
Botox is a commercial version of botulinum toxin. This is a poison that is created by the clostridium botulinum bacteria. From the World Health Organization (1):
Clostridium botulinum is a bacterium that produces dangerous toxins (botulinum toxins) under low-oxygen conditions. Botulinum toxins are one of the most lethal substances known. Botulinum toxins block nerve functions and can lead to respiratory and muscular paralysis.
Basically, botulinum toxin blocks the ability of the nerves to talk to muscles. When the doses are high as occurs in the disease botulism, you get paralysis and death. However, if you lower the dose, you can get reduced muscle tension for a few months. That’s why Botox and other botulinum toxin drugs have become so popular. They can reduce muscle tightness for a time.
Botox is on label right now for cosmetic purposes and for headaches. For the former, it relaxes muscles which can reduce wrinkles (and also make someone look expressionless), and for the later it can relax some of the tight muscles that irritate nerves and cause headaches. ALL OF THIS LASTS FOR ABOUT 3 MONTHS.
What are the Side Effects of Botox?
Can you inject a toxin that attacks the neuromuscular junction without any side effects? Here’s a short list of the problems caused by Botox:
- 40% reduction in muscle size and increased atrophy (2)
- Destroying senors for length-tension within the muscle (3)
- Changing genetic transcription within the injected muscle (4)
- Changes to muscle recruitment that don’t go back to normal (5)
- Weakening of the underlying bones that support the injected muscles (6)
Hence, Botox is NOT innocuous.
What is TMJ Syndrome?
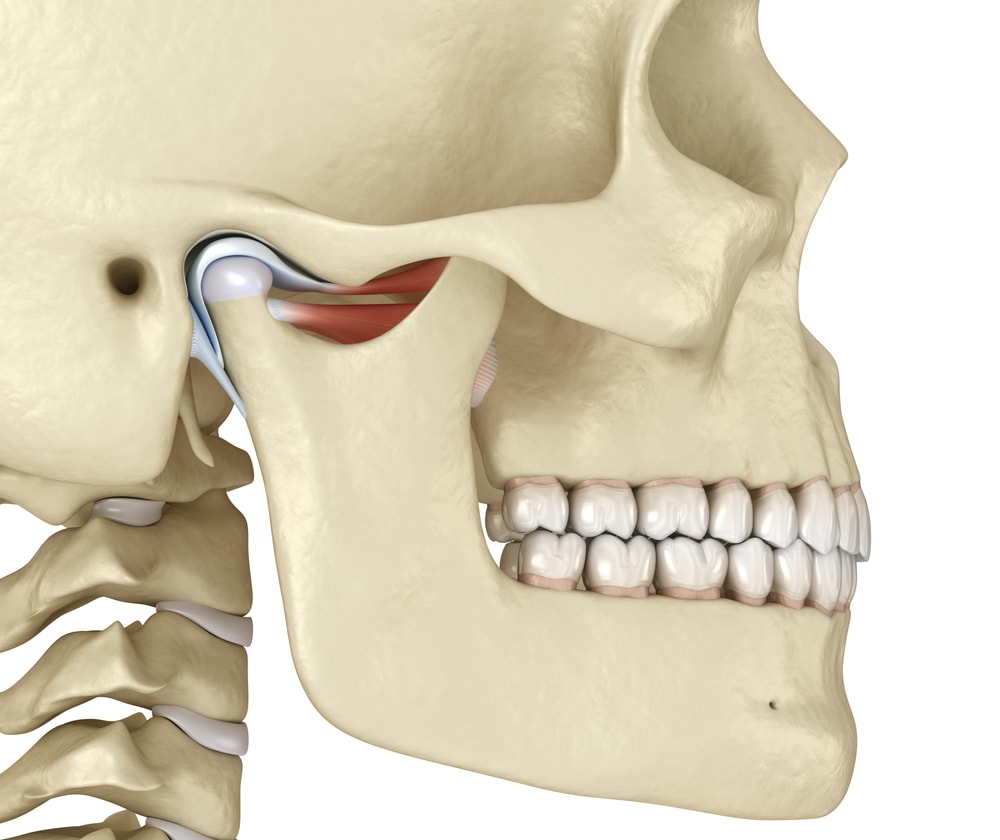
The TMJ (Temperomandibular) Joint is a hinge-like joint that has cartilage and also a meniscus-like structure:
Credit: Shutterstock
The joint can get injured just like any other in the body. That can be an injury to the cartilage, meniscus, or the ligaments that surround and help guide normal joint movement. The joint can also be chronically overloaded due to a poor head-forward posture. All of that wear and tear can lead to arthritis. When that happens, the muscles around the joint frequently spasm.
It’s this surrounding muscle spasm that is the target of Botox treatment for TMJ, so let’s delve into that idea, and then we’ll review what the research says.
TMJ Muscle Spasm
Why do muscles in the body spasm? Usually, this is a response to instability or joint injury. Instability means that the ligaments that are supposed to stabilize a joint are damaged, so the body locks down this area with muscle spasms. The same holds true for joint injury, the body is trying to lock down the joint to allow it to heal. Basically, in both instances, your body uses muscle spasms to help you lay off the area, and hopefully, this will allow enough time for the area to heal.
So if muscle spasm is protective, why would we want to get rid of it? First, it can be painful, so it would seem reasonable that patients would do anything to stop spasms. However, that strategy is likely penny-wise and pound-foolish. Meaning that short-term relief of the muscle spasm then allows the body to continue to load the unstable or injured joint leading to longer-term issues like arthritis.
Botox for TMJ
My family member was told that all she needed was 4 injections of Botox to cure her TMJ. Is there any research support to show that this statement is true? Here’s what I found:
- One study showed less bruxism at night (teeth grinding due to muscle spasms) when patients were injected with Botox (again up to 3 months) (7).
- Another study showed that Botox worked a bit less than a night splint for reducing TMJ pain thought due to bruxism (8). Botox did relax the jaw muscles for 3 months.
- A recent 2022 analysis of 24 TMJ Botox studies concluded that there is little evidence that Botox helps TMJ problems related to the joint (9).
Balancing The MOA, Risk, and Benefit for TMJ
MOA is the mechanism of action or how a drug or treatment works. Here, as already reviewed, the idea is that Botox will reduce muscle spasms, but since muscle spasm is likely protecting the joint, this MOA makes little sense. The risks for injecting Botox into muscles as shown above are not zero. Meaning we have some evidence of long-term damage to the muscle and nerves. As shown above, we don’t have any long-term randomized controlled trials that injecting Botox into jaw muscles will cure TMJ. Nor would this make any sense if the damage is inside the joint. Hence, the analysis of the dentist’s claim that there is a high likelihood that 4 Botox injections will cure TMJ shows this statement is not supported by the existing evidence.
PRP as a Treatment for TMJ
Conceptually, PRP or platelet-rich plasma would be a completely different approach to TMJ. Rather than targeting the temporary relaxation of tight jaw muscles, the target is the damage in the joint, meniscus, or ligaments surrounding the joint.
What does the existing research tell us? Here we actually have randomized controlled trials that focus on treating the joint:
- PRP was more effective than steroid injection in reducing joint pain for up to 12 months (10).
- A larger analysis of 6 randomized controlled trials for the use of PRP found that 4 reported superiority to hyaluronic acid (HA) or saline control with two negative trials (11). However, one of the negative and positive trials used arthroscopic surgery instead of the injections we’re discussing in this blog. So the actual score is 3 positive injection studies to one that showed similar results to HA.
How about PRP safety concerns? None have been documented to date.
So we have reasonable and early evidence that PRP injection targeting the joint helps for 12-24 months.
The upshot? Injecting the joint with PRP makes much more sense than injecting tight jaw muscles with Botox. In addition, there is no evidence to back up the claim that 4 Botox injections will reliably cure TMJ. Finally, with no serious long-term safety issues published for PRP injections and several studies detailing muscle damage due to Botox injections, this decision gets really easy to make.
_____________________________________________
(1) World Health Organization. Botulism. https://www.who.int/news-room/fact-sheets/detail/botulism Accessed 12/4/22
(2) Al-Al-Shaikh M, Michel F, Parratte B, Kastler B, Vidal C, Aubry S. An MRI evaluation of changes in piriformis muscle morphology induced by botulinum toxin injections in the treatment of piriformis syndrome. Diagn Interv Imaging. 2015 Jan;96(1):37-43. doi: 10.1016/j.diii.2014.02.015. Epub 2014 Apr 3. PMID: 24703886.
(3) Caron G, Rouzi T, Grelot L, Magalon G, Marqueste T, Decherchi P. Mechano- and metabosensitive alterations after injection of botulinum toxin into gastrocnemius muscle. J Neurosci Res. 2014 Jul;92(7):904-14. doi: 10.1002/jnr.23370. Epub 2014 Feb 25. PMID: 24615939.
(4) Mukund K, Mathewson M, Minamoto V, Ward SR, Subramaniam S, Lieber RL. Systems analysis of transcriptional data provides insights into muscle’s biological response to botulinum toxin. Muscle Nerve. 2014 Nov;50(5):744-58. doi: 10.1002/mus.24211. Epub 2014 Mar 17. PMID: 24536034; PMCID: PMC4136975.
(5) Fortuna R, Horisberger M, Vaz MA, Herzog W. Do skeletal muscle properties recover following repeat onabotulinum toxin A injections? J Biomech. 2013 Sep 27;46(14):2426-33. doi: 10.1016/j.jbiomech.2013.07.028. Epub 2013 Jul 26. PMID: 23953503.
(6) Warden SJ, Galley MR, Richard JS, George LA, Dirks RC, Guildenbecher EA, Judd AM, Robling AG, Fuchs RK. Reduced gravitational loading does not account for the skeletal effect of botulinum toxin-induced muscle inhibition suggesting a direct effect of muscle on bone. Bone. 2013 May;54(1):98-105. doi: 10.1016/j.bone.2013.01.043. Epub 2013 Feb 4. PMID: 23388417; PMCID: PMC3757093.
(7) Shim YJ, Lee HJ, Park KJ, Kim HT, Hong IH, Kim ST. Botulinum Toxin Therapy for Managing Sleep Bruxism: A Randomized and Placebo-Controlled Trial. Toxins (Basel). 2020 Mar 9;12(3):168. doi: 10.3390/toxins12030168. PMID: 32182879; PMCID: PMC7150956.
(8) Kaya DI, Ataoglu H. Botulinum toxin treatment of temporomandibular joint pain in patients with bruxism: A prospective and randomized clinical study. Niger J Clin Pract. 2021 Mar;24(3):412-417. doi: 10.4103/njcp.njcp_251_20. PMID: 33723117.
(9) Delcanho R, Val M, Guarda Nardini L, Manfredini D. Botulinum Toxin for Treating Temporomandibular Disorders: What is the Evidence? J Oral Facial Pain Headache. 2022 Winter;36(1):6-20. doi: 10.11607/ofph.3023. PMID: 35298571.
(10) Malahias MA, Roumeliotis L, Nikolaou VS, Chronopoulos E, Sourlas I, Babis GC. Platelet-Rich Plasma versus Corticosteroid Intra-Articular Injections for the Treatment of Trapeziometacarpal Arthritis: A Prospective Randomized Controlled Clinical Trial. Cartilage. 2021 Jan;12(1):51-61. doi: 10.1177/1947603518805230. Epub 2018 Oct 20. PMID: 30343590; PMCID: PMC7755966.
(11) Bousnaki M, Bakopoulou A, Koidis P. Platelet-rich plasma for the therapeutic management of temporomandibular joint disorders: a systematic review. Int J Oral Maxillofac Surg. 2018 Feb;47(2):188-198. doi: 10.1016/j.ijom.2017.09.014. Epub 2017 Oct 20. PMID: 29066000.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
