The Weak PRP Files: This Study Showed Good Clinical Results, But No Biomarker Changes

These past few weeks, we’ve seen what happens when academic physicians try to perform PRP studies. Their biggest mistake is often using very weakly concentrated blood that doesn’t meet the definition of PRP. This morning we’ll review a similar study that looked at knee arthritis biomarkers.
Prior Weak or Fake PRP Studies
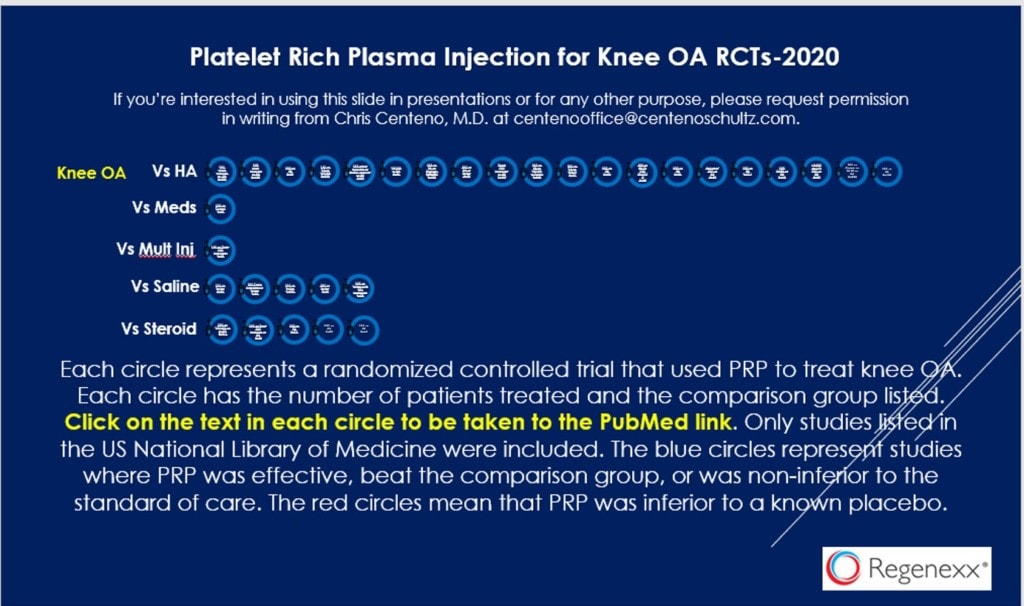
As you now know if you read this blog, we have some serious research horsepower behind PRP. For example, we have dozens of PRP randomized controlled trials that show that this is an effective knee arthritis treatment (each circle below is another study and has a hyperlink to that article):
Despite that, several studies were just published in the medical journal JAMA that showed negative results but used PRP that was so weak and diluted, it didn’t meet the minimum requirements for being PRP. This morning we’ll go over another interesting study that did use actual PRP, but just weak stuff.
The New Research
This new study was on 125 knee arthritis patients who were broken into a PRP and saline injection group (5). The good news is that the PRP group showed decreased knee pain and increased function out to one year. The interesting part was that the researchers found no change in biomarkers in the knee. What does that mean?
What the Heck Is a Biomarker?
In this context, a biomarker is a chemical that we can detect in the synovial fluid of the knee that shows the level of inflammation or the status of the cartilage. Meaning, one school of thought is that PRP works by reducing inflammation or cartilage destruction. Hence, we would expect that some of these biomarkers would change as a result of the PRP injection.
What Have Other PRP Biomarker Studies Shown?
What’s interesting about this new research is that it appears to be the “odd man out”. Meaning we have several studies that show that PRP helps knee arthritis biomarkers.
For example, a systematic review of animal models showed that more than 2/3rds of PRP studies improved the quality of cartilage and also improved biomarkers (1). A recent small ankle fracture study showed that injections of PRP improved the biomarkers associated with cartilage degradation (2). Another small RCT on knee arthritis patients also showed changes in knee inflammatory biomarkers (A2M) (3). A larger study showed that arthritic knees injected with PRP had a reduction in a cartilage breakdown marker (S.Coll2-1) (4).
Could There Be a Reason Why this Study Underperformed?
Given that we’ve seen a rash of studies using really bad PRP, the first thing I looked for was for any data on what was injected. I wasn’t disappointed. Basically, the authors claimed that their leukocyte poor PRP was 3.8 times concentrated, so pretty weak. However, the platelet count was on average 430,000. Given that the normal platelet range is 150-450,000, that’s not impressive. However, looking at volume reduction and recovery, their estimate of concentration is close enough.
While 3.8X may not be as bad as the recent JAMA studies (that were under 2X), remember that in using PRP the age of the patient matters. Here, that age was OLD. The average patient age was 67! That’s old for a knee OA study, where the average patient age is usually in the 50s. As I have already blogged, our internal data shows that 3.8X is way too low for this age group, meaning we would routinely use 14X.
There’s another problem with this data. The proportion of patients with severe KL 3/4 arthritis was very high at 78%! Other studies have shown that patients with this level of severe arthritis don’t do as well as patients with less severe OA. In addition, they have very little, if any cartilage left to impact.
Finally, which biomarkers were measured is important! The two that have been shown to be impacted by PRP in knee arthritis were A2M and S.Coll2-1. Was either of these biomarkers measured in the new study? Nope.
The upshot? While it’s great that yet another study shows that PRP is effective in the treatment of knee arthritis, we again see a study that used weak PRP. In addition, its conclusions that “biomarkers” don’t change is likely because the authors measured the wrong biomarkers, used PRP that was too weak, in patients that were too old, with arthritis that was too severe!
____________________________________________
(1) Boffa A, Salerno M, Merli G, De Girolamo L, Laver L, Magalon J, Sánchez M, Tischer T, Filardo G. Platelet-rich plasma injections induce disease-modifying effects in the treatment of osteoarthritis in animal models. Knee Surg Sports Traumatol Arthrosc. 2021 Dec;29(12):4100-4121. doi: 10.1007/s00167-021-06659-9. Epub 2021 Aug 2. PMID: 34341845.
(2) Zitsch BP, James CR, Crist BD, Stoker AM, Della Rocca GJ, Cook JL. A prospective randomized double-blind clinical trial to assess the effects of leukocyte-reduced platelet-rich plasma on pro-inflammatory, degradative, and anabolic biomarkers after closed pilon fractures. J Orthop Res. 2021 Jun 29. doi: 10.1002/jor.25123. Epub ahead of print. PMID: 34185333.
(3) Tucker JD, Goetz LL, Duncan MB, Gilman JB, Elmore LW, Sell SA, McClure MJ, Quagliano PV, Martin CC. Randomized, Placebo-Controlled Analysis of the Knee Synovial Environment Following Platelet-Rich Plasma Treatment for Knee Osteoarthritis. PM R. 2021 Jul;13(7):707-719. doi: 10.1002/pmrj.12561. PMID: 33492733.
(4) Fawzy RM, Hashaad NI, Mansour AI. Decrease of serum biomarker of type II Collagen degradation (Coll2-1) by intra-articular injection of an autologous plasma-rich-platelet in patients with unilateral primary knee osteoarthritis. Eur J Rheumatol. 2017 Jun;4(2):93-97. doi: 10.5152/eurjrheum.2017.160076. Epub 2017 Jun 1. PMID: 28638679; PMCID: PMC5473462.
(5) Ngarmukos, S., Tanavalee, C., Amarase, C. et al. Two or four injections of platelet-rich plasma for osteoarthritic knee did not change synovial biomarkers but similarly improved clinical outcomes. Sci Rep 11, 23603 (2021). https://doi.org/10.1038/s41598-021-03081-6

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.