Why It’s Time to Rethink Arthroscopy Shoulder Surgery
On this page:
- Arthroscopy shoulder surgery
- Shoulder decompression surgery
- Labrum repair or biceps tenodesis
- Rotator cuff repair
- Avoiding rotator cuff surgery
Arthroscopy shoulder surgery is a common way shoulder injuries are treated. However, since there are significant side effects, do you really need this surgery? These days, precise injections of your own platelets or stem cells are likely to be able to help without surgery. So let’s review.
Arthroscopy Shoulder Surgery
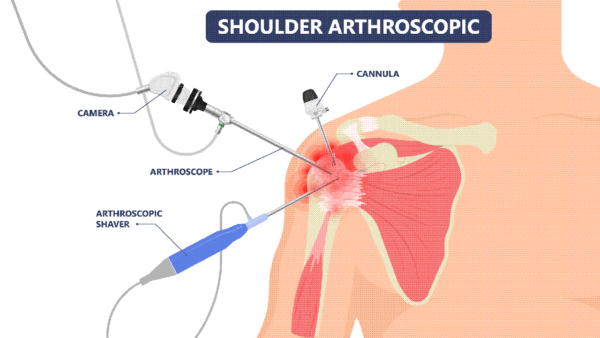
Arthroscopy shoulder surgery is pushed as a less invasive alternative to open shoulder surgery. The approach to the surgery involves creating anywhere from two to four incisions with portals leading to the damaged shoulder structure.
Rumruay/Shutterstock
Through one portal, the arthroscope (an instrument with a camera on the end that is linked to a video screen so the surgeon can visualize the surgical site) is passed through to the site. The other portals are used for whatever surgical instruments are necessary to accomplish a specific procedure.
Let’s take a look at some types of arthroscopy shoulder surgery and the reasons they might be performed.
Shoulder Decompression Surgery
With shoulder impingement, shoulder decompression surgery (aka acromioplasty) is a common surgical solution. The idea is that bone spurs can form, causing impingement of the rotator cuff, and the bone spurs must be cut off and the ligaments or acromioclavicular (AC) joint cut away to release the pressure on the rotator cuff.
This surface idea, however, doesn’t take into account that those ligaments and the AC joint are major shoulder stabilizers, and typically the bone spurs form to protect the joint from instability.
When the structures that stabilize the shoulder are cut away during decompression surgery, understandably, this creates another problem: shoulder instability (1). So while the impingement may be addressed, over time, more trauma is experienced by the shoulder as a result of the decompression surgery. Learn more about this surgery in my short video below.
Labrum Repair or Biceps Tenodesis
Arthroscopy shoulder surgery is often recommended for shoulder labrum tears. The labrum is a protective lip positioned around the socket part of the shoulder joint.
Depending on the type of labrum tear, a surgeon may perform a labrum repair or a biceps tenodesis. In the former, the torn part of the labrum is removed or stitched back together. In the latter, the biceps tendon is detached from the shoulder socket and reattached at the humerus (the upper arm bone) (2).
The problem with these surgeries is that retearing of the labrum is unavoidable as the cause of the tear in the first place — typically hidden shoulder instability — is rarely discovered or addressed. If hidden shoulder instability isn’t addressed, more tears are inevitable. Like many orthopedic surgeries, this is another one I label a surgery that is damage to accomplish a goal.
For a visual of hidden shoulder instability and labrum tears, take a look at the GIF below:
In addition, labrum surgery is riddled with side effects, such as, for starters, infections, failure, chronic pain, loss of biceps strength, and in the case of the biceps tenodesis, even cosmetic deformity of the biceps (2,3,4).
Rotator Cuff Repair
The rotator cuff is the complex of muscles and tendons that support the shoulder. When a rotator cuff tear is found in MRI, a rotator cuff surgery involves stitching the tear back together, is often recommended. On an MRI report, these tears would be classified by degree: partial (involving only part of the tendon) or full-thickness (the tendon is torn completely through).
Further if the tear is full-thickness, terminology will include either retracted (snapped back, like a rubber band) or nonretracted (not snapped back). To learn more about your shoulder and reading your own MRI shoulder report, watch my video below:
Like any other arthroscopy shoulder surgery, the lack of effective outcomes of rotator cuff repair are also concerning. Below I have listed a handful:
- A great deal of research has shown that for many types of tears, rotator cuff surgery is largely ineffective (5).
- Even the full-thickness rotator cuff tears have been shown to improve just as well with physical therapy (6). In other words, surgery improved the rotator cuff tear no better than PT.
- Rotator cuff tear surgery, unfortunately, doesn’t seem to result in less pain, regardless of the severity of the tear (7).
- The large rotator cuff tears have been shown to not heal correctly—as many as 6 in 10 following surgery (8).
- 60 or older! The news is bad here too, as one October 2011 study suggests 1 in 3 rotator cuff tears don’t heal following surgery in this age group (9).
Avoiding Rotator Cuff Surgery
These days, about 7 in 10 patients who are told they need arthroscopy shoulder surgery can avoid these procedures. How? Precise X-ray- or ultrasound-guided injections of your own platelets or stem cells can help with healing or reduce pain and increase function.
However, these are difficult procedures to perform correctly, so you need a physician super-specialist who is often not an orthopedic surgeon to perform these procedures. Specifically, they can not be performed at a high level by a nurse or physician assistant in a chiropractic office. To see what one of these procedures looks like, see my video below:
The upshot? Arthroscopy shoulder surgery can often be avoided, which is a good thing considering the side effects and the lack of evidence that we have that these invasive procedures are effective. So take some time to dive deep into your research on this procedure before pulling the trigger on surgery.
————————————–
References
(1) Denard PJ, Bahney TJ, Kirby SB, Orfaly RM. Contact pressure and glenohumeral translation following subacromial decompression: how much is enough?. Orthopedics. 2010;33(11):805. Published 2010 Nov 2. doi:10.3928/01477447-20100924-02
(2) Virk MS, Nicholson GP. Complications of Proximal Biceps Tenotomy and Tenodesis. Clin Sports Med. 2016;35(1):181-188. doi:10.1016/j.csm.2015.08.011
(3) Provencher MT, McCormick F, Dewing C, McIntire S, Solomon D. A prospective analysis of 179 type 2 superior labrum anterior and posterior repairs: outcomes and factors associated with success and failure. Am J Sports Med. 2013;41(4):880-886. doi:10.1177/0363546513477363
(4) Weber SC, Martin DF, Seiler JG 3rd, Harrast JJ. Superior labrum anterior and posterior lesions of the shoulder: incidence rates, complications, and outcomes as reported by American Board of Orthopedic Surgery. Part II candidates. Am J Sports Med. 2012;40(7):1538-1543. doi:10.1177/0363546512447785
(5) Seida JC, LeBlanc C, Schouten JR, et al. Systematic review: nonoperative and operative treatments for rotator cuff tears. Ann Intern Med. 2010;153(4):246-255. doi:10.7326/0003-4819-153-4-201008170-00263
(6) Khatri C, Ahmed I, Parsons H, et al. The Natural History of Full-Thickness Rotator Cuff Tears in Randomized Controlled Trials: A Systematic Review and Meta-analysis. Am J Sports Med. 2019;47(7):1734-1743. doi:10.1177/0363546518780694
(7) Okamura K, Kobayashi T, Yamamoto A, et al. Shoulder pain and intra-articular interleukin-8 levels in patients with rotator cuff tears. Int J Rheum Dis. 2017;20(2):177-181. doi:10.1111/1756-185X.12581
(8) Abtahi AM, Granger EK, Tashjian RZ. Factors affecting healing after arthroscopic rotator cuff repair. World J Orthop. 2015;6(2):211-220. Published 2015 Mar 18. doi:10.5312/wjo.v6.i2.211
(9) Dezaly C, Sirveaux F, Philippe R, et al. Arthroscopic treatment of rotator cuff tear in the over-60s: repair is preferable to isolated acromioplasty-tenotomy in the short term. Orthop Traumatol Surg Res. 2011;97(6 Suppl):S125-S130. doi:10.1016/j.otsr.2011.06.006

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
