Upper Back Stomach Pain: Saving a Life
In treating patients in pain all day every day, every once in a while, you can save a life. So today’s patient story is about just that, a patient with a pinched nerve in his upper back who had “upper back stomach pain” that was so severe that he was contemplating suicide. I just saw him back today and now he’s down to a 2/10 “I can live with this”. How he got there, the medical mistakes along the way, and how he got better is a story that can hopefully save other patients.
Thoracic Radiculopathy
A common cause of upper back stomach pain or when you have pain in the upper back that seems to radiate around to the stomach is a pinched nerve. In this case, that often means a lower thoracic nerve. The term “thoracic” simply means the upper back. Radiculopathy is a medical term that refers to a pinched or irritated nerve. This can happen when there is a disc bulge or herniation at the level where the spinal nerve exits.
Abdominal Pain is Common with this Problem
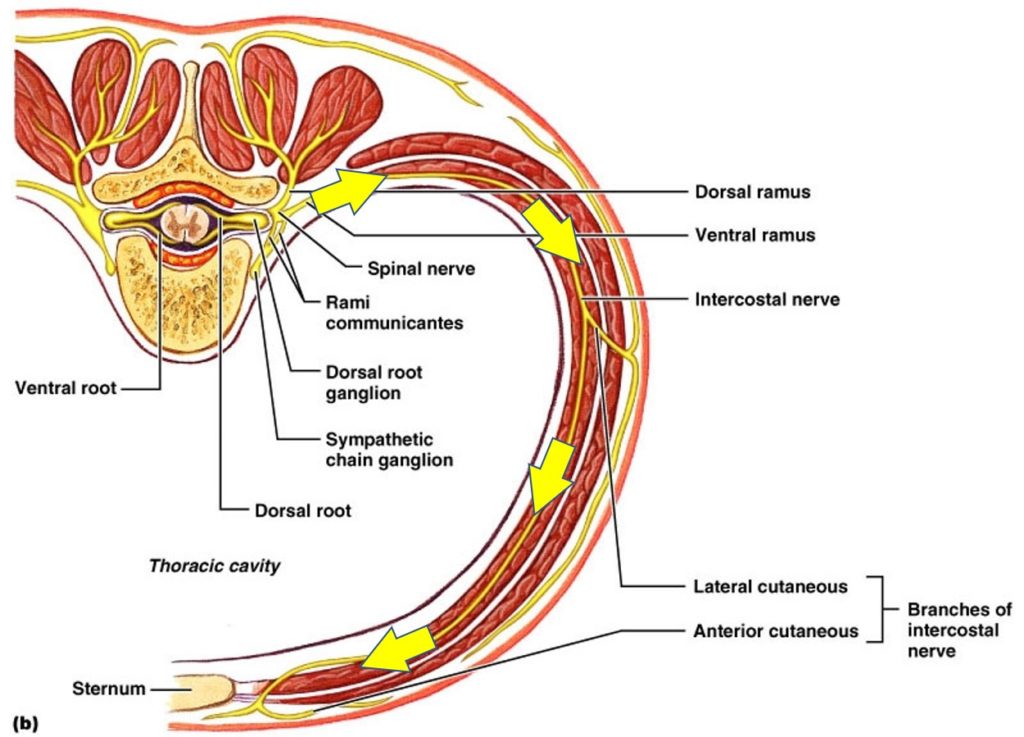
The stomach pain part of the upper back problem is caused by the spinal nerve turning into an intercostal nerve that travels all the way around and under the ribs to the stomach area. In the diagram below, note that the spinal nerve exits the upper backbone at the top of the image and then follows the yellow arrows all the way around the rib to the front where the ribs meet the upper stomach.
Ron’s Thoracic Pain Story
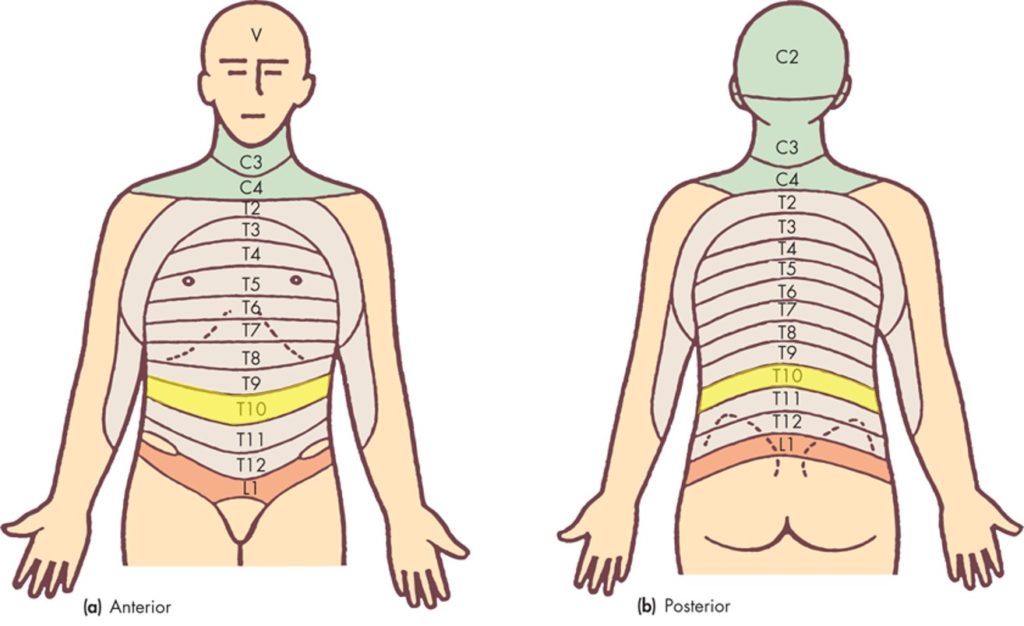
Ron works for a local radio station and has a history of multiple back surgeries. As such, he’s been on a steady dose of narcotics for years and managed by another clinic. About 6 months ago, he began having wrap around abdominal pain in the front. This was severe 9-10/10 pain. His doctors first put him through the “million dollar” work-up that involved 27 tests on various abdominal structures. This included a colonoscopy, endoscopy, a HIDA scan, you name it, he had it. All came back stone cold normal. Then one day he was seeing his pain management doctor, who got an upper back MRI that demonstrated a T10-T11 disc bulge. If you take a look at the thoracic dermatome map below, I have highlighted (yellow) where the T10 nerve that was pinched by the bulging disc travels. Note that it’s right in the upper stomach area:
The problem from there was that the doctor obviously didn’t have much experience with injecting the area around the T10 nerve (To-T11 transforaminal epidural), so he kept injecting the high lumbar nerves, which didn’t help the T10 level. In addition, he was injecting high-dose steroids, which also didn’t help Ron. So when I saw him, he was contemplating suicide because of months of severe unrelenting pain.
The Thoracic Spine is Often “No Man’s Land”
One of the issues we see on a day to day basis is that most pain management doctors ignore the thoracic spine. Why? Injecting this area is more technically demanding, hence residency and fellowship programs tend to avoid it. In addition, there is much overlap between the neck and the thoracic spine. For example, lower neck joints and irritated nerves can refer pain into the shoulder blade areas. However, ignoring this part of the spine is not wise. Let me explain.
What can go wrong in the upper back? As discussed above, you can have a bulging or herniated disc pressing on a nerve. You can have a facet joint problem here, just like you can in the neck or low back. You can also have a rib facet problem or an issue where the rib meets the spine. Finally, the ribs themselves can develop problems that can lead to pain that can wrap around to the front. Hence, there is much that can go wrong here, so ignoring a whole section of the spine is not a good idea.
Ron’s Treatment
Ron was seen for a platelet lysate epidural at T10-T11. This is an injection of the patient’s own healing growth factors around the disc bulge and inflamed nerves. I also injected the nerves under the ribs and the painful ribs themselves, as the fascial covering those ribs were lax and allowing too much rib motion. What is platelet lysate? See my video below:
Ron came back in today and told me I saved his life. It’s now a very manageable 2/10. I also told him he needed a second treatment, which we will get done in the next few weeks.
The upshot? There are doctors like those who work in trauma and cancer care that get to save lives every day. Those of us that work in orthopedics and pain management don’t get as much opportunity to lay claim to that honor. However, this case was a great example where that can happen!

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.