Cervical Multifidus Muscle Atrophy: A Literature Update
Most patients and many physicians don’t know that we have mounting research that the muscles that stabilize your neck can weaken and this can be easily seen on MRI. Today we’ll go over that research and show patients what this atrophy looks like on their images. Let’s dig in.
Spinal Stabilizer Atrophy
We’ve known for a long time that the small muscles that stabilize your low back vertebrae atrophy in patients with back and leg pain. What’s bizarre, is that few radiologists decide to place this information in radiology reports. Hence, most patients don’t know that they have this issue. What’s even more bizarre is that this also happens in the neck, but even fewer people know about this research.
Upper Neck Muscle Atrophy
This body of research begins with an old colleague, Jim Elliott. Here’s what Dr. Elliott has found and published about neck stabilizer atrophy:
- In patients with chronic headaches, the rectus capitis posterior major and minor muscles were significantly smaller on MRI (1).
- Patients with chronic whiplash-caused neck pain and general neck pain have both deep spinal muscle atrophy (smaller muscles) as well as denervation pseudohypertrophy where the muscles get weaker, but overall larger due to being infiltrated with fat (2). The fatty infiltration of muscles doesn’t appear to happen in patients with atraumatic neck pain.
- Older women with cervicogenic headaches also have atrophied and fat infiltrated upper neck stabilizer muscles (3).
- Whiplash injured patients have a poorer network brain structure on fMRI (evidence of brain disorganization) and that is associated with fatty neck muscle atrophy (4).
- Patients with degenerative cervical myelopathy (pressure on their spinal cord) had more deep neck muscle fatty atrophy and this atrophy was associated with more disability and a worse surgical outcome (5).
- Cervical deep muscle fatty atrophy happens soon after a whiplash injury, but only in patients with poor recovery and this problem progresses rapidly (6).
- The deep neck flexor muscles also have more fatty atrophy in whiplash patients (7).
- In asymptomatic women aged 18-45, the fatty infiltration of the deep upper neck muscles is not related to age (8).
What are the Implications of this Fatty Atrophy?
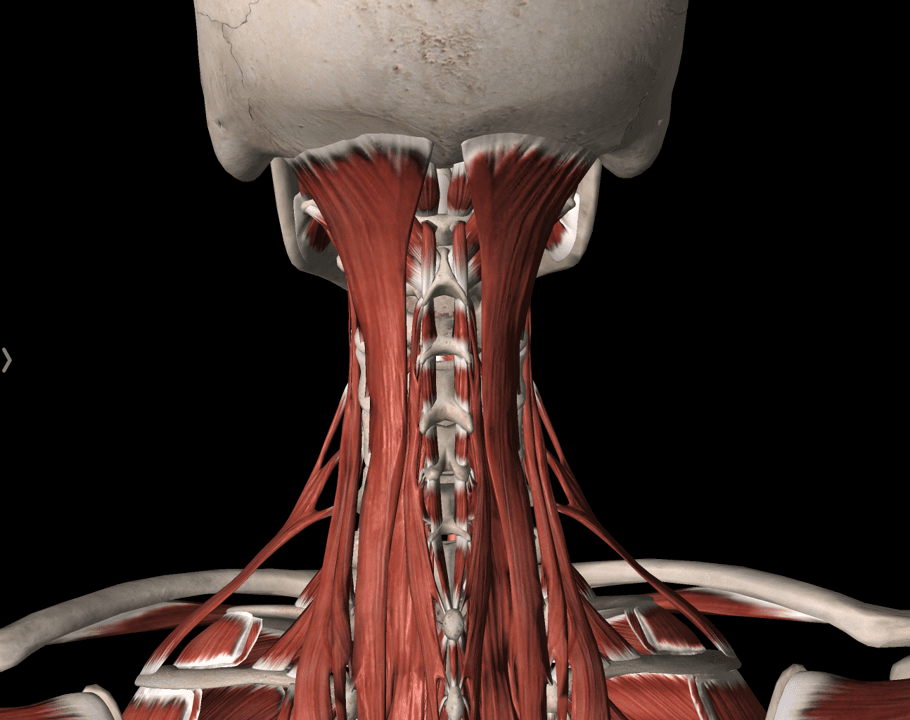
The entire spine has small and deep muscles that help to keep your vertebrae perfectly aligned as you move. These protect all the structures that can potentially be damaged or tweaked if the bones become misaligned. In general, while some of these neck muscles have specific names, as a group they are called multifidus.
These muscles are weaker and are responsible for stabilizing one vertebra on another. Hence, the levels that have this fatty atrophy are unstable. In traumatic neck pain (like chronic neck pain caused by a car crash), this atrophy can be usually seen in the upper neck. In other problems like chronic nerve or spinal cord irritation, this problem can be seen in the mid to lower neck. Either way, this problem can cause the spinal nerves to be continuously tweaked, disc injury events, and arthritic facet joints.
Can You Easily See this Problem on Your MRI?
This fatty atrophy isn’t hard to spot. Here are the steps to check for this problem:
1. Find the axial MRI images. These are the views that look like a steak at the grocery store because they represent a cross-section. There may be several series of these images. You’re looking for the one that looks like the picture below on the right. Water should be white (the area around the spinal cord where there is cerebral spinal fluid (CSF)), and fat is white (the area just under the skin or subcutaneous, and muscle is dark. This is called the “T2” image and it may be labeled “Ax T2”. While 80% of neck MRIs will have this image sequence, regrettably a few don’t include it. If you can’t find this T2 image sequence, then you may not be able to get further. 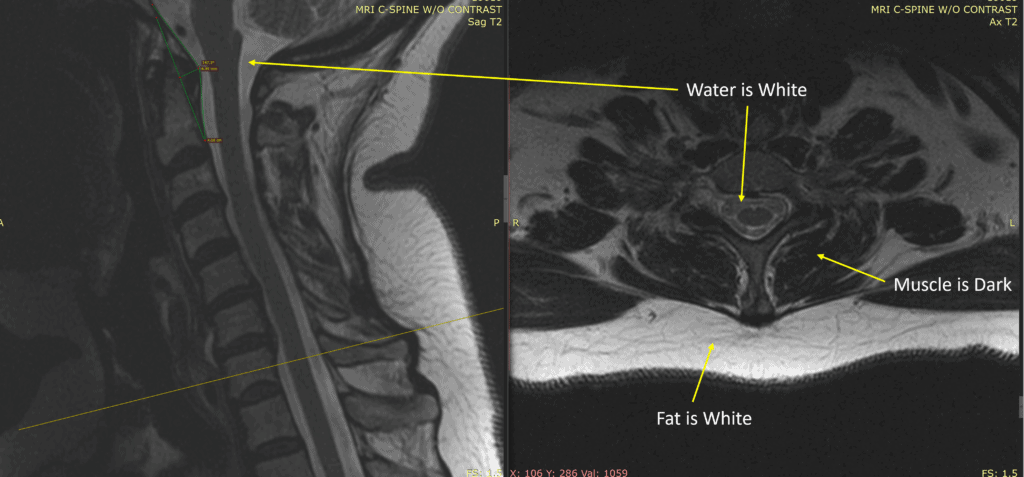
2. Identify the muscles you should be paying attention to which are shown below as the deepest muscle group, labeled as “Multifidus” below.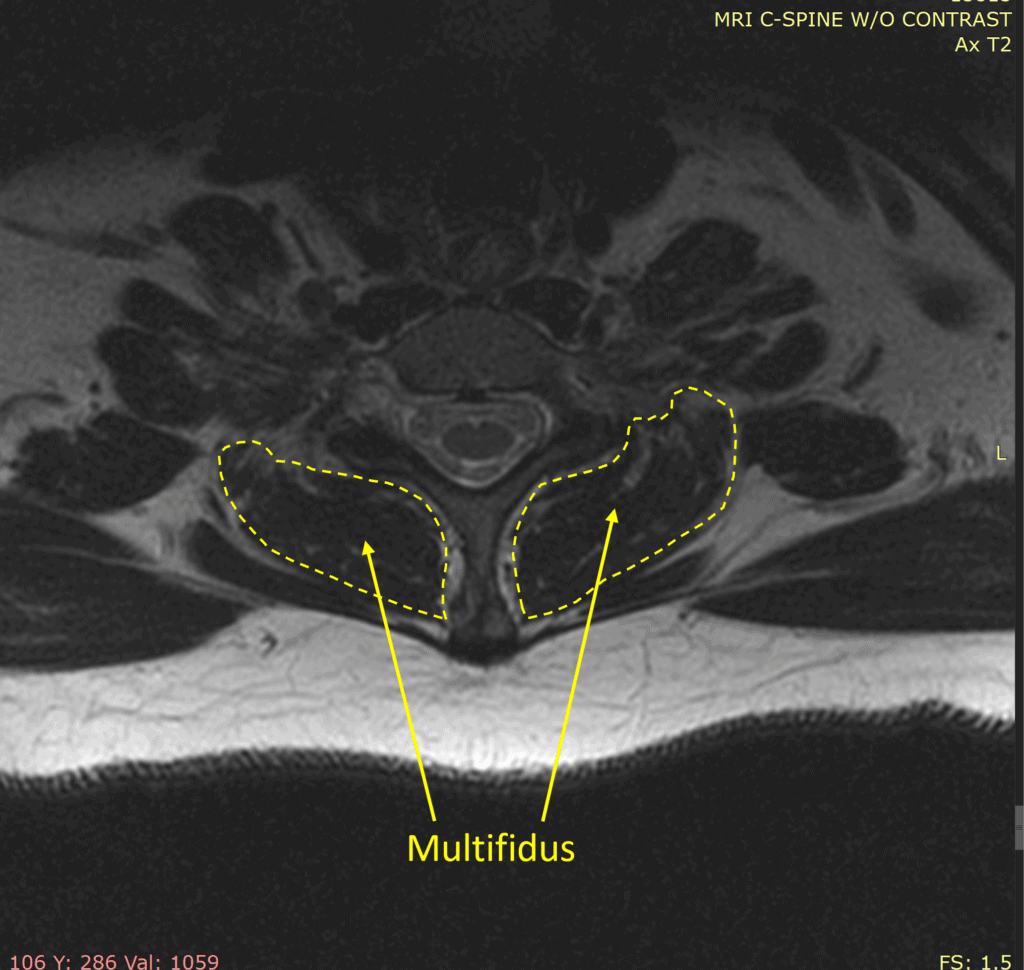
3. Scroll up or down looking for more white than dark muscle in this compartment, as shown below: 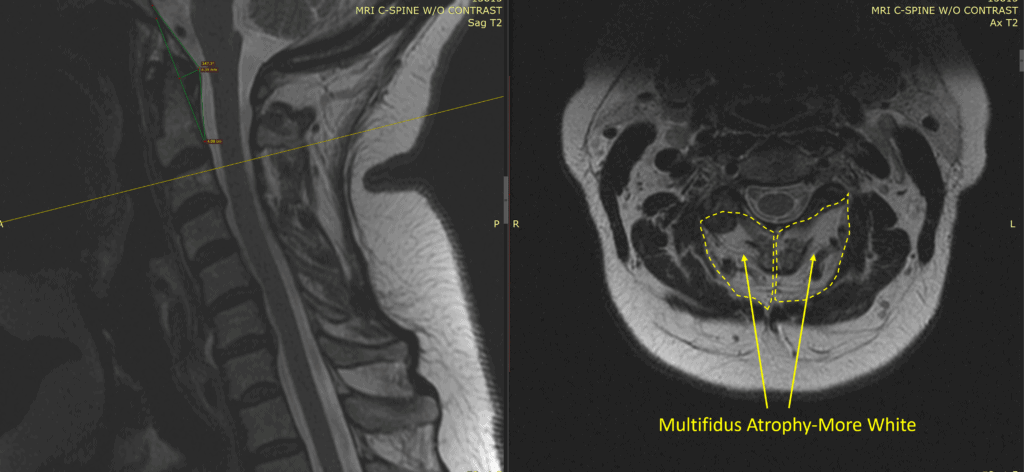
Multifidus atrophy is when you see a substantial amount of white within the dark muscle or more white than dark (as shown). In the image above, since I have the sagittal on the left (side view), I know that this axial slice is about C2-C3.
What Can You Do If You Have Cervical Multifidus Atrophy?
If you have cervical multifidus atrophy, then there are really two steps to getting out of pain or feeling better. First, try physical therapy. Some patients will only need that step and can begin strengthening these muscles. If that doesn’t work, then the protocol is often:
- Find and treat the source of pain or nerve irritation that’s causing the atrophy. Usually, this means treating the facet joint, lax ligaments causing instability, or irritated nerves with precise fluoroscopically guided platelet injections.
- Once the causes are treated, then you can begin strengthening these muscles.
What NOT To Do
Cervical radiofrequency ablation (RFA) is a common treatment for painful neck facet joints. However, this treatment kills the nerves that supply these muscles, so it would be CONTRAINDICATED in a patient with cervical multifidus atrophy.
The upshot? Cervical multifidus atrophy is common in patients with chronic neck pain. Despite the mounting research on this issue, radiologists rarely pay attention to this finding. Hence, that means that patients and savvy doctors must check for this issue!
___________________________________________________________
References:
(1) Fernández-de-Las-Peñas C, Bueno A, Ferrando J, Elliott JM, Cuadrado ML, Pareja JA. Magnetic resonance imaging study of the morphometry of cervical extensor muscles in chronic tension-type headache. Cephalalgia. 2007 Apr;27(4):355-62. doi: 10.1111/j.1468-2982.2007.01293.x. PMID: 17376113.
(2) Elliott JM, Pedler AR, Jull GA, Van Wyk L, Galloway GG, OʼLeary SP. Differential changes in muscle composition exist in traumatic and nontraumatic neck pain. Spine (Phila Pa 1976). 2014 Jan 1;39(1):39-47. doi: 10.1097/BRS.0000000000000033. PMID: 24270932.
(3) Uthaikhup S, Assapun J, Kothan S, Watcharasaksilp K, Elliott JM. Structural changes of the cervical muscles in elder women with cervicogenic headache. Musculoskelet Sci Pract. 2017 Jun;29:1-6. doi: 10.1016/j.msksp.2017.02.002. Epub 2017 Feb 22. PMID: 28259769.
(4) Higgins JP, Elliott JM, Parrish TB. Brain Network Disruption in Whiplash. AJNR Am J Neuroradiol. 2020 Jun;41(6):994-1000. doi: 10.3174/ajnr.A6569. Epub 2020 Jun 4. PMID: 32499250; PMCID: PMC7342774.
(5) Paliwal M, Weber KA 2nd, Smith AC, Elliott JM, Muhammad F, Dahdaleh NS, Bodurka J, Dhaher Y, Parrish TB, Mackey S, Smith ZA. Fatty infiltration in cervical flexors and extensors in patients with degenerative cervical myelopathy using a multi-muscle segmentation model. PLoS One. 2021 Jun 25;16(6):e0253863. doi: 10.1371/journal.pone.0253863. PMID: 34170961; PMCID: PMC8232539.
(6) Elliott JM, Courtney DM, Rademaker A, Pinto D, Sterling MM, Parrish TB. The Rapid and Progressive Degeneration of the Cervical Multifidus in Whiplash: An MRI Study of Fatty Infiltration. Spine (Phila Pa 1976). 2015 Jun 15;40(12):E694-700. doi: 10.1097/BRS.0000000000000891. PMID: 25785961; PMCID: PMC4466088.
(7) Elliott JM, O’Leary S, Sterling M, Hendrikz J, Pedler A, Jull G. Magnetic resonance imaging findings of fatty infiltrate in the cervical flexors in chronic whiplash. Spine (Phila Pa 1976). 2010 Apr 20;35(9):948-54. doi: 10.1097/BRS.0b013e3181bb0e55. PMID: 20118837.
(8) Elliott JM, Galloway GJ, Jull GA, Noteboom JT, Centeno CJ, Gibbon WW. Magnetic resonance imaging analysis of the upper cervical spine extensor musculature in an asymptomatic cohort: an index of fat within muscle. Clin Radiol. 2005 Mar;60(3):355-63. doi: 10.1016/j.crad.2004.08.013. PMID: 15710139.

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
