Multifidus Back Pain: Why Isn’t Your Doctor Talking About It?
Many people have multifidus back pain, but most have never been diagnosed with it. In fact, you’ve likely never even heard of multifidus back pain because you doctor probably has never talked about it. If he or she isn’t looking at your multifidus when looking for the cause of back pain, he or she is way behind the times and isn’t keeping up with the latest research, which we’ll talk about in a moment. First, what is the multifidus, and what does it have to do with your back?
The Multifidus: The Spinal Stability Muscle
So what is the multifidus? The multifidus is a spinal muscle located deep in the back (watch the brief video above to see a radiology image). Unlike the superficial back muscles that help you move your back around, the multifidus works at a much deeper level, functioning as the major stabilizer of the spine. The multifidus can atrophy, meaning it can shrink, or experience other problems that result in functional problems and pain in the low back. Interestingly, it’s not difficult to see multifidus atrophy on MRI, so what does this look like?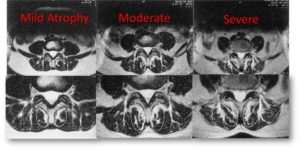
On the image to the right, you can see the multifidus muscle in the circled areas. The muscle is the dark part, and you can see how it shrinks away as the atrophy goes from mild to moderate to severe. (In the video, there is an image comparing a normal multifidus to an atrophied one). The white that is filling in as the muscle shrinks is fat atrophy, and that is the clear sign of an abnormal multifidus. Despite how easy it is to find on MRI, radiologists almost never read it and put it in their reports. Why?
Radiologists generally still read images to define whether surgery is needed or not, and there is really no surgery for multifidus back pain. Radiologists, who tend to only read what the surgeons want them to, are looking for bones or discs that might be pressing on nerves…anything that could justify or rule out surgery. It’s an antiquated behavior following a decades-old structural model of the spine, and it needs to change: surgeons and radiologists need to read the research and catch up to the times. Compounding the issue is that surgery, such as a spinal fusion, can result in very significant damage to the multifidus, and, therefore, the stability of the spine. The same holds true for radiofrequency lesioning (RFA-a common back pain injection based remedy), which destroys the nerve that supplies the multifidus.
You might be thinking, That’s good to know, Dr Centeno, but what is this research you speak of that shows that atrophy is a problem? I’m glad you asked.
The Research
At the time of this writing, a search of the US National Library of Medicine for research on low back multifidus and pain and how that correlates to MRI yields 119 studies. There’s really a lot of research on the topic.
The vast majority of these studies correlate multifidus atrophy with poorer outcomes and functional problems in the low back. Hence, your doctor should be reading your MRI images for this issue and showing it to you and designing therapies to alleviate the problem. Given that we’ve known about this problem for 24 years, since 1993 (Flicker et al), if your doctor isn’t discussing it, he or she hasn’t kept up with the research.
I can’t cover every study on this topic in the US National Library of Medicine (see studies link above), but here are the highlights of some of the latest research from just the last 12 months:
- The severity of multifidus atrophy on MRI is directly correlated with the decreased ability to bend forward and with back pain (Hildebrandt).
- Disc degeneration on MRI is associated with bone changes and multifidus atrophy indicating a “whole organ” pathology (Teichtahl).
- The fatty composition of the multifidus muscles in back pain was directly correlated to poor physical function in yet another study (Sions).
The upshot? If your back pain just won’t stop, it could be multifidus back pain, which your doctor likely isn’t considering. The truth is, the multifidus is probably the most important muscle you’ve never heard of, and as the growing stack of research shows (119 studies to date), when this muscle isn’t properly functioning, it can create chaos all through your spine—in the vertebra, discs, joints, nerves, and other muscles. Multifidus back pain due to atrophy is a real problem, and if your doctor isn’t considering it, you should find another doctor!
References
Flicker, P. L., et al. “Lumbar muscle usage in chronic low back pain. Magnetic resonance image evaluation.” Spine (Phila Pa 1976). 1993 Apr;18(5): 582–6.
Hildebrandt, M., et al. “Correlation Between Lumbar Dysfunction and Fat Infiltration in Lumbar Multifidus Muscles in Patients with Low Back Pain.” BMC Musculoskelet Disord. 2017 Jan 10;18(1):12.
Sions, J. M., et al. “Multifidus Muscle Characteristics and Physical Function Among Older Adults With and Without Chronic Low Back Pain.” Arch Phys Med Rehabil. 2017 Jan;98(1):51–57.
Teichtahl, A. J., et al. “Lumbar disc degeneration is associated with modic change and high paraspinal fat content—a 3.0T magnetic resonance imaging study.” BMC Musculoskelet Disord. 2016 Oct 21;17(1):439.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.