The Vagus Nerve, Neck Pain, Anxiety, Headaches, and Depression
On this page:
- The function of the vagus nerve
- Neck pain and the vagus nerve
- Other symptoms of an irritated vagus nerve
We’ve seen neck pain patients for years with lots of seemingly unrelated symptoms. Many have suffered from depression, anxiety, headaches, and some even cardiac problems like runs of tachycardia. So what’s causing all of this? Let’s delve into some new research on the vagus nerve.
The Function of the Vagus Nerve
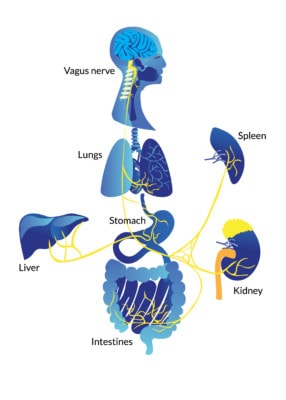
Not all who wander are lost and the vagus nerve — Latin for “wandering” nerve — keeps us found. The tenth of the twelve cranial nerves, the vagus nerve reaches from the brain into the far reaches of our body not unlike the root system of a tree.
The longest, largest, and most complex of the cranial nerves, the vagus nerve influences symptom changes in all sorts of problems such as depression, migraines, epilepsy, inflammation, and arthritis, among others. In addition, stimulating the nerve with medical devices has been shown to be effective in treating many conditions (5,6)
FatkhulAnwari/ Shutterstock
The more we learn about this wandering nerve, the more we realize we need to know. For example, we know that by stimulating the vagus nerve we can treat depression. Further down, the system reaches the gut, and those with digestive issues and acid reflux are often found to have insufficient vagal activity. In between, the nerve’s activation or deactivation connects to the well-being of the heart, lungs, and immune system (2).
And while we still don’t know all that the vagus nerve does, we have come to understand that it is the Zen mediator of the parasympathetic nervous system — the laid-back sibling to the sympathetic system and its fight-or-flight response. Meaning that if the vagus nerve is working well, we can relax and become meditative. If it’s not working, then we become anxious and overstimulated.
The ‘wanderer’ controls our relaxation levels by slowing heart rate, switching off inflammatory responses, and initiating the release of calming chemicals (1). Enough activity can soothe an asthma attack or even an epileptic seizure. Incredibly, research shows that many conditions exacerbated by inflammation or stress can be helped by stimulating the vagus nerve. In fact, an entire medical device industry has sprung up around surgically implanted stimulators for the vagus nerve.
Historically, a surgical implant in the chest with a wire and lead that goes to the neck is used for stimulation of the vagus nerve. The idea is that by electrically stimulating the nerve, we can treat patients whose nerve isn’t working well.
In addition to implantable stimulators, there is a new treatment with FDA approval that employs a patch pressed against the neck to soothe migraines and cluster headaches (5). And now new research is underway into cures for mental health disorders such as depression (3). Meaning, when you control the vagus nerve, you control quite a bit about how a person feels on a day to day basis.
Neck Pain and the Vagus Nerve
When doctors see patients with chronic neck pain, many aren’t sure how to interpret what they see. Many of these patients are anxious, depressed, and just a little “crazy.” In fact, when I was in training and then just beginning private practice, many of my colleagues thought most of these chronic neck pain patients were “crazy and lazy.” The lazy part came from the fact that many were made worse by traditional physical therapy and didn’t want to continue hurting themselves.
For me, all of that changed after a key study was published that showed that if you got rid of their neck pain, these patients were no longer crazy, meaning that depression and anxiety went away (4). Meaning, that the study showed us that something going on in the neck was causing these symptoms. So patients weren’t crazy and lazy, they just had a neck problem. Could this be the vagus nerve?
Where the vagus nerve travels may explain why we see patients with lots of crazy symptoms. This includes depression, anxiety, and rapid heart rate (tachycardia). Why the rapid heart rate? The vagus nerve acts as the brakes for the heart. So irritation of the nerve by surrounding muscles or bones can lead to inhibition of the nerve thus removing the brakes for heart rate, which means a faster heart. The nerve has also been implicated in headaches (7).
Other Symptoms of an Irritated Vagus Nerve
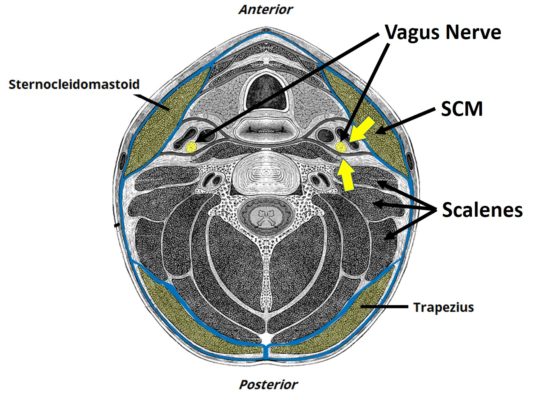
The image below shows the mid-neck (click on the image below to see a bigger version). Note that the vagus nerve is right behind the Sternocleidomastoid muscle (SCM) and right in front of the scalenes. What are some of the tightest muscles in the necks of patients who have had injuries like whiplash? The SCM and the scalenes. Hence, irritation of the vagus nerve by these structures may explain many of the symptoms we see in these patients. In addition, remember that the vagus nerve is “the wanderer,” so it goes lots of other places where it can get irritated or have pressure placed on it. Let’s explore some of those.
If we go back to the top, where the vagus nerve comes out of the skull, we can see why these same symptoms commonly plague patients with craniocervical instability (CCI). In the image below, you’re looking at the skull base as the dotted lines and the two circles are holes in the skull where the different nerves exit. The Foramen magnum is the big hole at the bottom of the skull where the spinal cord and nerves exit. The Jugular Foramen is another smaller hole where the spinal accessory nerve and the vagus nerve come out.

In CCI patients, the skull is not stable on the neck. So these nerves are bound to get yanked around more, leading to irritation and vagus nerve dysfunction. In addition, the spinal accessory nerve also goes to the SCM and upper trap muscles, which are also muscles that are commonly tight in these patients. Meaning an irritated nerve can cause a tight and irritated muscle.
Let’s also take a look at the proximity of the vagus nerve to the atlas, which is C1. In the diagram I created to the left, note that the vagus nerve exits that jugular foramen and then travels right over the side of the atlas (C1 highlighted in yellow).
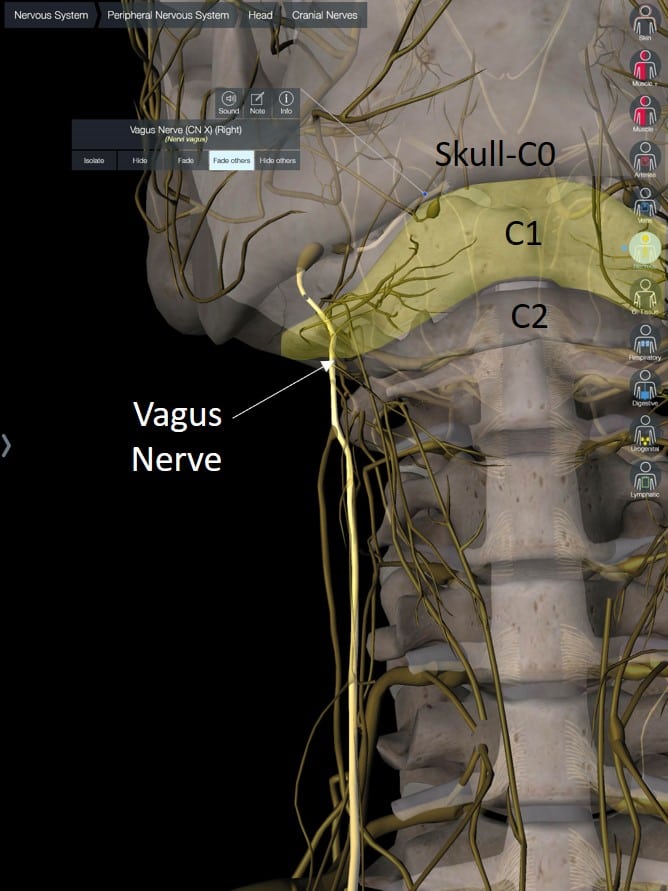
In patients with CCI, C1 is often unstable in a side-to-side direction, which can be seen as too much C1-C2 overhang on a DMX study. Hence, the vagus nerve can be bagged in more than one spot in CCI patients.
So is it any wonder that many have rapid heart rate? Or anxiety? Or depression? Their vagus nerve is getting yanked something fierce every time they move their neck and head.
The upshot? The vagus nerve is responsible for lots of stuff in our bodies. If it works well, it helps us relax. If it doesn’t, we can get a rapid heart rate, anxiety, depression, and a host of other issues. This nerve is also likely responsible for many of the symptoms that neck pain and CCI instability patients suffer. Hence, they’re not “crazy or lazy,” their vagus nerve is just really messed up!
_____________________________________________
References
(1) Keltner D. Secrets of the Vagus Nerve. Greater Good Magazine. The Science of a Meaningful Life video series. July 2012. https://greatergood.berkeley.edu/video/item/secrets_of_the_vagus_nerve
(2) Yuan H, Silberstein SD. Vagus Nerve and Vagus Nerve Stimulation, a Comprehensive Review: Part I. Headache. 2016 Jan;56(1):71-8. doi:10.1111/head.12647
(3) Lv H, Zhao YH, Chen JG, Wang DY, Chen H. Vagus Nerve Stimulation for Depression: A Systematic Review. Front Psychol. 2019;10:64. doi:10.3389/fpsyg.2019.00064
(4) Wallis BJ, Lord SM, Bogduk N. Resolution of psychological distress of whiplash patients following treatment by radiofrequency neurotomy: a randomised, double-blind, placebo-controlled trial. Pain. 1997 Oct;73(1):15-22. doi:10.1016/s0304-3959(97)00060-2
(5) Johnson RL, Wilson CG. A review of vagus nerve stimulation as a therapeutic intervention. J Inflamm Res. 2018;11:203–213. doi:10.2147/JIR.S163248
(6) Thayer JF. Vagal tone and the inflammatory reflex. Cleve Clin J Med. 2009 Apr;76 Suppl 2:S23-6. doi:10.3949/ccjm.76.s2.05
(7) Lendvai IS, Maier A, Scheele D, Hurlemann R, Kinfe TM. Spotlight on cervical vagus nerve stimulation for the treatment of primary headache disorders: a review. J Pain Res. 2018;11:1613–1625. doi:10.2147/JPR.S129202

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
