What Happens to Umbilical Cord IV Stem Cells in the Lungs? It’s NOT Pretty
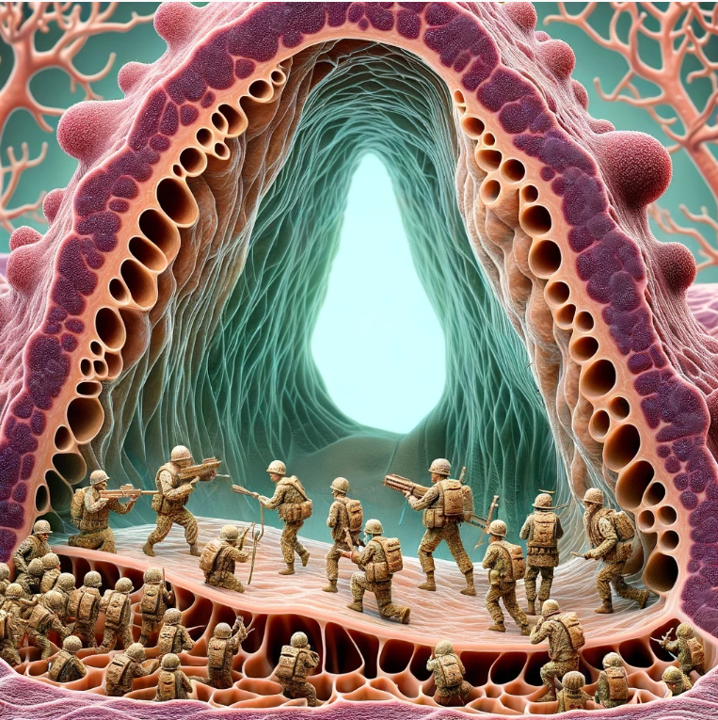
One of the most common delivery methods for stem cells is intravenous (IV). However, this seems to have been chosen more because it’s easy for the clinic than because it’s the best way to deliver stem cells. Today, I will discuss a new study and review why IV stem cell infusions remain problematic. In particular, we’ll focus on the war that’s happening in the lungs between the stem cells and the host’s immune system.
The Pulmonary First Pass Effect
We’ve known for many decades that drug medications have a hepatic first-pass effect (1). Meaning a good chunk of the drugs you take get chewed up in the Liver, and the minority of that survives to enter your bloodstream. For the last 10-15 years, we’ve known that the same thing happens with stem cells injected IV (2,3). They end up getting chewed up in a pulmonary first pass. This means that most get trapped in the lungs. However, as more has come to light on this issue, we are now finding out that stem cells injected IV get more than just trapped in the lungs, if they are allogeneic, they get killed in the lungs.
How the New Research Was Done
First, this was an animal model of IV umbilical cord stem cell injection (4). Like all animal allogenic stem cell studies, these are pooled cells, which differs from single donor expanded products. These cells are likely better tolerated than the single donor products being used out there. Why? Because when you use the stem cells of many animals, you increase the odds that some will be a match for the patient. When you use one person’s cells and place them into another, there’s a bigger chance of a mismatch.
I thought Stem Cells Were Immune Privileged or Immunoevasive?
Most physicians are taught that someone else’s stem cells (allogeneic) do not cause an immune response in the host. Regrettably, that’s not true. Many prior research studies I have covered here on this blog show that the host’s immune system recognizes allogeneic stem cells as foreign (5-7).
What Did the New Research Find?
Because the discussion portion of the paper is a review of the topic of allogeneic stem cells delivered IV, I have quoted a few passages from the paper and then have my comments. All paper references are listed below in the second reference section.
There is an initial inflammatory response after the stem cells delivered IV get stuck in the lungs:
“Overall, hUC-MSCs triggered an innate immune response shortly after being infused intravenously. The increase in inflammatory cell types agrees with findings that have shown that MSCs delivered IV induce an inflammatory response in the lung, as evidence by macrophage infiltration (28). Moreover, the localisation of macrophages in close proximity to the MSCs at 2 h post-hUC-MSC administration suggests that the clearance of the exogenous cells from the lungs might involve efferocytosis by phagocytes (56).”
The above discussion basically says that because of that initial inflammatory response, the macrophages begin to clear the stem cells, meaning these cells are being recognized as foreign.
Also, the foreign stem cells in the lungs are killed off by the host’s immune system:
“Ourselves and others have shown that following IV administration, most MSCs die within 24 h (1,2). It has been suggested that this rapid cell death might be required for the MSCs to exert their benefits (56). After IV injection, MSCs undergo apoptosis in the lung. Their subsequent efferocytosis by macrophages was suggested to be the mechanism behind the reduction in the severity of allergic asthma (64). Moreover, clinical data from patients with graft-versus-host disease (GvHD) who have been administered MSCs intravenously, as well as preclinical murine models showed that the host’s cytotoxic cells actively induce the exogenous MSCs to undergo apoptosis. This results in a recipient-induced immunomodulation which is required for improved outcomes (65). In keeping with the finding that viable MSCs are not required to ameliorate injury, heat-inactivated MSCs were able to maintain their immunomodulatory capacity and reduce sepsis in mice (66,67).”
The authors say that the newly dead or dying stem cells may still be able to have a positive impact on the host, leading to an eventual anti-inflammation host response. The bottom line is that nobody is quite sure how that works, but this response may not be all that different from the response that we see with prolotherapy. In the latter case, causing a brief inflammatory response may eventually yield healing based on the body’s response to the challenge.
The authors go on to state that even though they used stem cells from another species, the same effects were observed when cells from the same species were used. They believe the response is from stem cells being encountered in areas where they usually are not and that this causes a systemic inflammatory reaction that can be detected in the bloodstream:
“Here, we used xenogeneic cells, but studies that have used syngeneic (28) and allogeneic (68) MSCs have also observed an inflammatory immune reaction after MSC delivery, suggesting that the response is not due to the cells being from another species, but rather a response to the MSCs being present in an atypical location, which initiates a clearance mechanism (28). In line with this, the immune system reacts to cells that are not normally in contact with the bloodstream (69). The direct interaction between the MSCs and the blood immediately after infusion might trigger an instant blood-mediated inflammatory reaction (IBMIR), that would not be expected when administering cells that are normally present in the blood circulation, such as leukocytes (70). IBMIR causes platelet-, coagulation-, and complement activation, and results in the MSCs being destroyed quickly, inducing the innate immune system to eliminate them (71).”
In addition, the ultimate response of inducing more or less inflammation is likely linked to the disease state in which the MSCs are introduced:
“As discussed above, the disease context can influence MSC behaviour (76,77). MSCs can either promote or suppress the immune response as shown by in vitro culture of MSCs exposed to different clinical bronchoalveolar lavage (BAL) samples representing a wide range of lung pathologies (77). In our study, healthy animals were used; if injured animals had been studied, it is possible that the results might have differed. Thus, the understanding of the effect of IV delivery of hUC-MSCs on the innate immune system in different disease and inflammatory contexts remains to be elucidated.”
So, at the end of the day, we don’t really know how allogeneic MSCs delivered IV work:
“How the immunoregulatory properties of MSCs relates to their beneficial effects in disease and injury models remains unclear. Nevertheless, immunomodulation by innate immune cells mediated by the MSC secretome as well as by direct interaction with viable, apoptotic, inactivated, and fragmented MSCs has been established (56). Importantly, MSCs appear to be able to induce therapeutic effects without long-term engraftment (78).”
Auto vs. Allo
This is another study showing potential serious issues with allogeneic stem cells. While I knew that allogeneic stem cells caused a host immune response, I didn’t know that several papers now show that these cells, when delivered IV, are not only stuck in the lungs but killed there by the host’s immune system. That brings up the whole field of necrobiology (can dead stem cells still work?) that we are just starting to understand.
More critically, many studies continue to demonstrate problems with the “stem cells in a vial” business plan that aren’t an issue with autologous cells. For example, we know that when we use the patient’s stem cells, they “stay and play” (they survive and engraft) versus this “hit and run” mechanism of allogeneic stem cell function (8).
The upshot? Injecting someone with IV allogeneic stem cells causes a war in the lungs between the cells and the host’s immune system. They may cause an eventual anti-inflammatory response, or in the wrong patients, you may kick off an inflammatory response; there are just more questions at this point than answers. In the meantime, I wouldn’t rush down to Mexico or Panama to get IV umbilical cord stem cells, as the results of this study are a little concerning.
__________________________________________________
My References:
(1) Herman TF, Santos C. First-Pass Effect. [Updated 2023 Nov 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK551679/
(2) Ferrini E, Stellari FF, Franceschi V, Macchi F, Russo L, Murgia A, Grisendi G, Villetti G, Dominici M, Donofrio G. Persistency of Mesenchymal Stromal/Stem Cells in Lungs. Front Cell Dev Biol. 2021 Jul 16;9:709225. doi: 10.3389/fcell.2021.709225. PMID: 34336863; PMCID: PMC8322774.
(3) Fischer UM, Harting MT, Jimenez F, Monzon-Posadas WO, Xue H, Savitz SI, Laine GA, Cox CS Jr. Pulmonary passage is a major obstacle for intravenous stem cell delivery: the pulmonary first-pass effect. Stem Cells Dev. 2009 Jun;18(5):683-92. doi: 10.1089/scd.2008.0253. PMID: 19099374; PMCID: PMC3190292.
(4) Hernandez Pichardo A, Wilm B, Liptrott NJ, Murray P. Intravenous Administration of Human Umbilical Cord Mesenchymal Stromal Cells Leads to an Inflammatory Response in the Lung. Stem Cells Int. 2023 Sep 5;2023:7397819. doi: 10.1155/2023/7397819. PMID: 37705699; PMCID: PMC10497368.
(5) Joswig AJ, Mitchell A, Cummings KJ, Levine GJ, Gregory CA, Smith R 3rd, Watts AE. Repeated intra-articular injection of allogeneic mesenchymal stem cells causes an adverse response compared to autologous cells in the equine model. Stem Cell Res Ther. 2017 Feb 28;8(1):42. doi: 10.1186/s13287-017-0503-8. PMID: 28241885; PMCID: PMC5329965.
(6) Rowland AL, Miller D, Berglund A, Schnabel LV, Levine GJ, Antczak DF, Watts AE. Cross-matching of allogeneic mesenchymal stromal cells eliminates recipient immune targeting. Stem Cells Transl Med. 2021 May;10(5):694-710. doi: 10.1002/sctm.20-0435. Epub 2020 Dec 25. PMID: 33369287; PMCID: PMC8046071.
(7) Ankrum JA, Ong JF, Karp JM. Mesenchymal stem cells: immune evasive, not immune privileged. Nat Biotechnol. 2014 Mar;32(3):252-60. doi: 10.1038/nbt.2816. Epub 2014 Feb 23. PMID: 24561556; PMCID: PMC4320647.
(8) Henriksson HB, Papadimitriou N, Hingert D, Baranto A, Lindahl A, Brisby H. The Traceability of Mesenchymal Stromal Cells After Injection Into Degenerated Discs in Patients with Low Back Pain. Stem Cells Dev. 2019 Sep 1;28(17):1203-1211. doi: 10.1089/scd.2019.0074
References from the Paper Being Reviewed:
(1) Scarfe L, Taylor A, Sharkey J, Harwood R, Barrow M, Comenge J, Beeken L, Astley C, Santeramo I, Hutchinson C, Ressel L, Smythe J, Austin E, Levy R, Rosseinsky MJ, Adams DJ, Poptani H, Park BK, Murray P, Wilm B. Non-invasive imaging reveals conditions that impact distribution and persistence of cells after in vivo administration. Stem Cell Res Ther. 2018 Nov 28;9(1):332. doi: 10.1186/s13287-018-1076-x. PMID: 30486897; PMCID: PMC6264053.
(2) Eggenhofer E, Benseler V, Kroemer A, Popp FC, Geissler EK, Schlitt HJ, Baan CC, Dahlke MH, Hoogduijn MJ. Mesenchymal stem cells are short-lived and do not migrate beyond the lungs after intravenous infusion. Front Immunol. 2012 Sep 26;3:297. doi: 10.3389/fimmu.2012.00297. PMID: 23056000; PMCID: PMC3458305.
(28) Hoogduijn MJ, Roemeling-van Rhijn M, Engela AU, Korevaar SS, Mensah FK, Franquesa M, de Bruin RW, Betjes MG, Weimar W, Baan CC. Mesenchymal stem cells induce an inflammatory response after intravenous infusion. Stem Cells Dev. 2013 Nov 1;22(21):2825-35. doi: 10.1089/scd.2013.0193. Epub 2013 Aug 9. PMID: 23767885.
(56) Weiss DJ, English K, Krasnodembskaya A, Isaza-Correa JM, Hawthorne IJ, Mahon BP. The Necrobiology of Mesenchymal Stromal Cells Affects Therapeutic Efficacy. Front Immunol. 2019 Jun 4;10:1228. doi: 10.3389/fimmu.2019.01228. PMID: 31214185; PMCID: PMC6557974.
(64) Galleu A, Riffo-Vasquez Y, Trento C, Lomas C, Dolcetti L, Cheung TS, von Bonin M, Barbieri L, Halai K, Ward S, Weng L, Chakraverty R, Lombardi G, Watt FM, Orchard K, Marks DI, Apperley J, Bornhauser M, Walczak H, Bennett C, Dazzi F. Apoptosis in mesenchymal stromal cells induces in vivo recipient-mediated immunomodulation. Sci Transl Med. 2017 Nov 15;9(416):eaam7828. doi: 10.1126/scitranslmed.aam7828. PMID: 29141887.
(66) Weiss ARR, Lee O, Eggenhofer E, Geissler E, Korevaar SS, Soeder Y, Schlitt HJ, Geissler EK, Hoogduijn MJ, Dahlke MH. Differential effects of heat-inactivated, secretome-deficient MSC and metabolically active MSC in sepsis and allogenic heart transplantation. Stem Cells. 2020 Jun;38(6):797-807. doi: 10.1002/stem.3165. Epub 2020 Mar 12. PMID: 32101344.
(67) Xia Z, Ye H, Choong C, Ferguson DJ, Platt N, Cui Z, Triffitt JT. Macrophagic response to human mesenchymal stem cell and poly(epsilon-caprolactone) implantation in nonobese diabetic/severe combined immunodeficient mice. J Biomed Mater Res A. 2004 Dec 1;71(3):538-48. doi: 10.1002/jbm.a.30185. PMID: 15481051.
(68) Moll G, Jitschin R, von Bahr L, Rasmusson-Duprez I, Sundberg B, Lönnies L, Elgue G, Nilsson-Ekdahl K, Mougiakakos D, Lambris JD, Ringdén O, Le Blanc K, Nilsson B. Mesenchymal stromal cells engage complement and complement receptor bearing innate effector cells to modulate immune responses. PLoS One. 2011;6(7):e21703. doi: 10.1371/journal.pone.0021703. Epub 2011 Jul 1. PMID: 21747949; PMCID: PMC3128611.
(69) Moll G, Ankrum JA, Kamhieh-Milz J, Bieback K, Ringdén O, Volk HD, Geissler S, Reinke P. Intravascular Mesenchymal Stromal/Stem Cell Therapy Product Diversification: Time for New Clinical Guidelines. Trends Mol Med. 2019 Feb;25(2):149-163. doi: 10.1016/j.molmed.2018.12.006. Epub 2019 Jan 30. PMID: 30711482.
(70) Soria-Juan B, Escacena N, Capilla-González V, Aguilera Y, Llanos L, Tejedo JR, Bedoya FJ, Juan V, De la Cuesta A, Ruiz-Salmerón R, Andreu E, Grochowicz L, Prósper F, Sánchez-Guijo F, Lozano FS, Miralles M, Del Río-Solá L, Castellanos G, Moraleda JM, Sackstein R, García-Arranz M, García-Olmo D, Martín F, Hmadcha A, Soria B; Collaborative Working Group “Noma Project Team”. Cost-Effective, Safe, and Personalized Cell Therapy for Critical Limb Ischemia in Type 2 Diabetes Mellitus. Front Immunol. 2019 Jun 4;10:1151. doi: 10.3389/fimmu.2019.01151. Erratum in: Front Immunol. 2020 Sep 02;11:2029. PMID: 31231366; PMCID: PMC6558400.
(71) Song X, Xie S, Lu K, Wang C. Mesenchymal stem cells alleviate experimental asthma by inducing polarization of alveolar macrophages. Inflammation. 2015 Apr;38(2):485-92. doi: 10.1007/s10753-014-9954-6. PMID: 24958014.
(76) Abreu SC, Rolandsson Enes S, Dearborn J, Goodwin M, Coffey A, Borg ZD, Dos Santos CC, Wargo MJ, Cruz FF, Loi R, DeSarno M, Ashikaga T, Antunes MA, Rocco PRM, Liu KD, Lee JW, Matthay MA, McKenna DH, Weiss DJ. Lung inflammatory environments differentially alter mesenchymal stromal cell behavior. Am J Physiol Lung Cell Mol Physiol. 2019 Dec 1;317(6):L823-L831. doi: 10.1152/ajplung.00263.2019. Epub 2019 Sep 25. PMID: 31553626; PMCID: PMC6962599.
(77) Spees JL, Lee RH, Gregory CA. Mechanisms of mesenchymal stem/stromal cell function. Stem Cell Res Ther. 2016 Aug 31;7(1):125. doi: 10.1186/s13287-016-0363-7. PMID: 27581859; PMCID: PMC5007684.
(78) Calcat-I-Cervera S, Rendra E, Scaccia E, Amadeo F, Hanson V, Wilm B, Murray P, O’Brien T, Taylor A, Bieback K. Harmonised culture procedures minimise but do not eliminate mesenchymal stromal cell donor and tissue variability in a decentralised multicentre manufacturing approach. Stem Cell Res Ther. 2023 May 4;14(1):120. doi: 10.1186/s13287-023-03352-1. PMID: 37143116; PMCID: PMC10161493.

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
