What Is a Proper Diagnostic Block Headache Work-up?

Credit: Shutterstock
There are so many structures in the neck and head that can cause headaches that it’s almost tough to find them all and put them on a big list. However, after having many patients with chronic headaches come into the office and claim that after a simple Occipital Nerve Block that they have had a full diagnostic workup, I thought it was time for a review of all of these things. So let’s jump in.
What Is an Interventional Diagnostic Workup for Headache?
If you have a chronic headache and neck pain, you may want to begin with yesterday’s blog that goes over all of the different approaches to headache pain based on medical specialty. From an Interventionist standpoint, there are MANY things that cause headaches and each one needs to be crossed off of a big list. How does that work?
The idea here is centered around a diagnostic block. That means that the doctor uses imaging guidance to place the needle in a very precise and specific spot and then injects numbing medicine. The concept is that if structure A is causing the headache, once that structure is numbed out, all or part of the headache should go away for the duration of the numbing effect. Once the structure causing the headache is identified, we can then decide how best to treat that issue.
How Often Is a Proper Headache Work-up Like the One Described Here Performed?
ALMOST NEVER! I have yet to see a patient walk in my office, no matter what famous Medical Center they have been to or which famous department head they saw, get a complete diagnostic work-up for all of the things that can cause headache. What usually happens is that they see a Neurologist who performs a few simple, blind (without guidance) in-office nerve blocks and when that doesn’t help, the work-up is considered complete. As you’ll see below, a proper diagnostic block work-up is MUCH MORE COMPLEX than what the neurologist considered.
Does This Mega-Workup Always Need to Be Done?
NO. Oftentimes the doctor, based on physical exam and history can get clues as to what’s causing the headache and just begin treatment and this will be successful. This larger workup should only be performed if that fails. Obviously, the workup stops once the culprit is found.
A Proper Diagnostic Block Work-up For Headache
A proper headache work-up is quite complex because there are so many neck and head structures that can cause headaches. This is an almost complete list:
- C0-C1 facet joint
- C1-C2 facet joint
- C2-C3 facet joint
- Greater occipital nerve
- Lesser occipital nerve
- Third occipital nerve at C2-C3
- Third occipital nerve at posterior C2
- Superficial cervical plexus at the SCM
- Supraoribital and supratrochlear nerves
- Auriculo-temperoal nerve
- C2 dorsal root ganglion
- C2-C3 Disc
- Sphenopalatine Ganglion
- Many muscle trigger points
The Upper Cervical Facet Joints
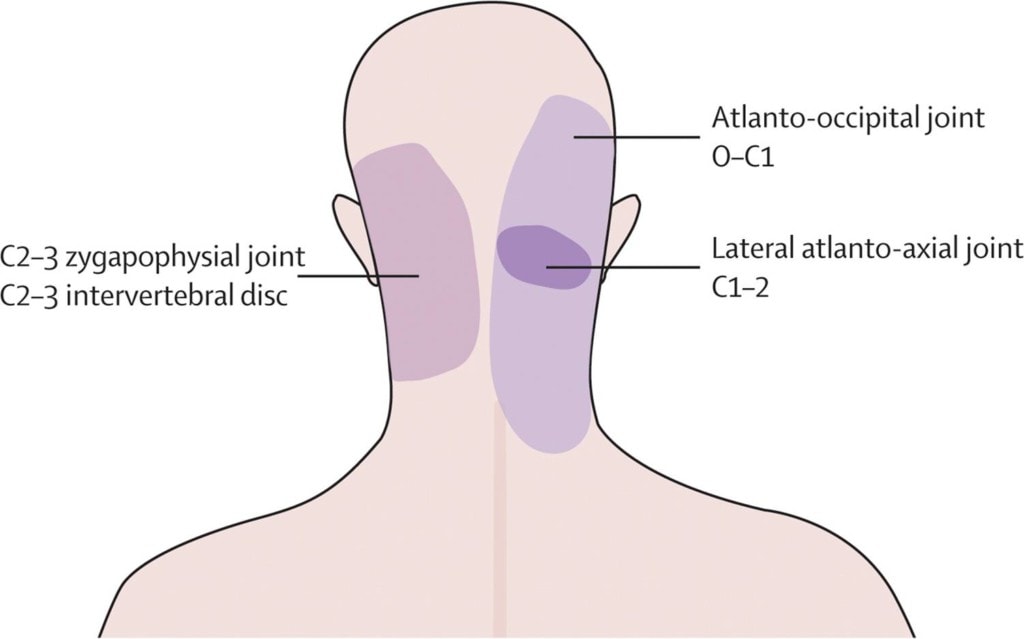
These are small finger-sized joints that occur at each level and on each side of your neck. They can be injured in trauma like a car crash or if there is upper neck instability (CCI). They can be also be injured by wear and tear. Each joint refers pain to various parts of the head as shown above. While injection of the C2-C3 joint can be easily performed by many interventional pain physicians, finding someone with loads of experience in injecting the C1-C2 and C0-C1 joint can be more problematic.
The Occipital Nerves
Credit: Shutterstock
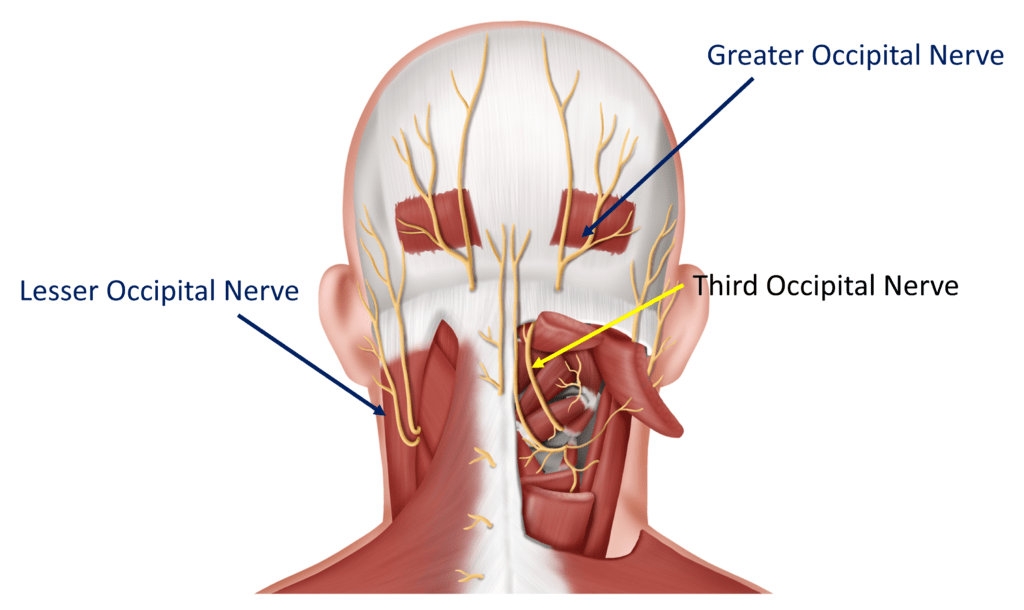
The Occipital nerves are at the back of the head. Any tightness in the muscles near these nerves can cause them to become irritated and since they all innervate the head, when irritated, the patient gets headaches. Injecting the Greater and Lesser Occipital nerves for a diagnostic block is not hard to do and is commonly done by neurologists in the office. You need to make sure the back of your head goes numb to make sure the nerve was actually blocked correctly.
The third Occipital nerve is harder to inject, so this should be done only by an experienced Interventional Pain Management doctor. It can be blocked at two places:
- The outside part of the C2-C3 Facet joint-This is commonly done using x-ray guidance.
- The back of the upper neck at C2, just on the backside (posterior) of the Suboccipital muscles (Obliquus Capitis Inferior, Rectus Capitis Minor, Rectus Capitis major) using ultrasound imaging.
Superficial Cervical Plexus/Transverse Cervical Nerve
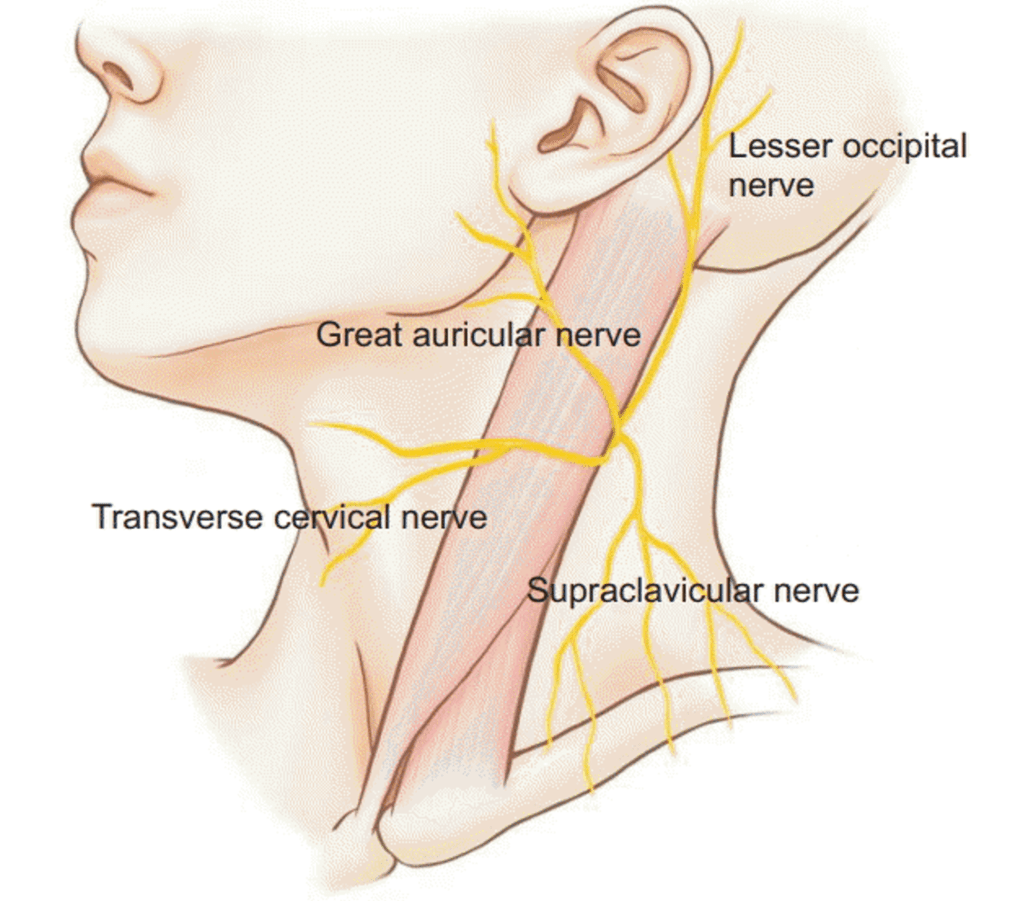
A very big collection of nerves exits just under and from behind the Sternocleidomastoid (SCM). This is called the Superficial Cervical Plexus. These nerves go lots of places with one becoming the Lesser Occipital Nerve mentioned above. This plexus can cause headache pain behind the ear or on the side and in the back of the head. The Greater Auricular nerve causes pain in front of the ear and the Transverse Cervical nerve goes into the front of the neck while the Supraclavicular nerve goes to the collar bone area.
These nerves commonly get irritated when the SCM muscle (the big strap muscle in the front of the neck) gets too tight. This can happen for lots of reasons, but we often see it in conjunction with upper neck problems at c1-C2. This nerve can be numbed with precise ultrasound guidance with the injectate being placed under the back part of the SCM muscle where the nerves exit.
Auriculo-temperoal Nerve
The Auriculo-temporal nerve lives on the side of the head and just behind the TMJ and jaw. Hence, it’s often irritated in patients with TMJ syndrome and causes headaches on the side of the head. A block here needs to be performed with ultrasound or x-ray guidance.
C2-C3 Disc

The intervertebral discs in the neck and back can cause pain. The C2-C3 disc, if painful, can cause pain in the back of the neck, at the base of the back of the skull. To see if this is causing pain, the doctor needs to perform a Diagnostic Discogram using x-ray guidance and contrast at the C2-C3 disc. This procedure pressurizes the disc to see if this type of headache pain is reproduced.
Sphenopalatine Ganglion

This is a Ganglion (a collection of sensory nerves) in the nasal cavity that can cause headaches and often pain in the roof of the mouth and teeth. The good news is that it’s easy to block. The doctor just needs to place some topical lidocaine on a long Q-tip cotton swab and place it into the far back wall of the nasal cavity, as shown above.
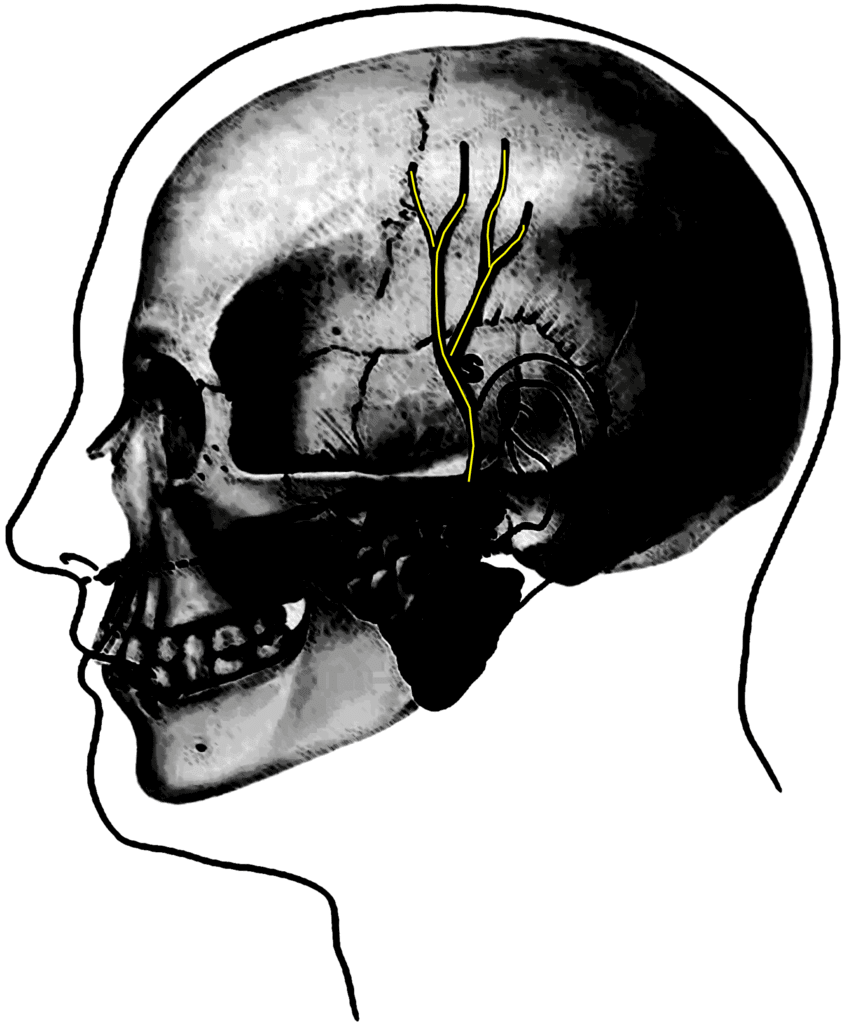
Supraorbital and Supratrochlear Nerves
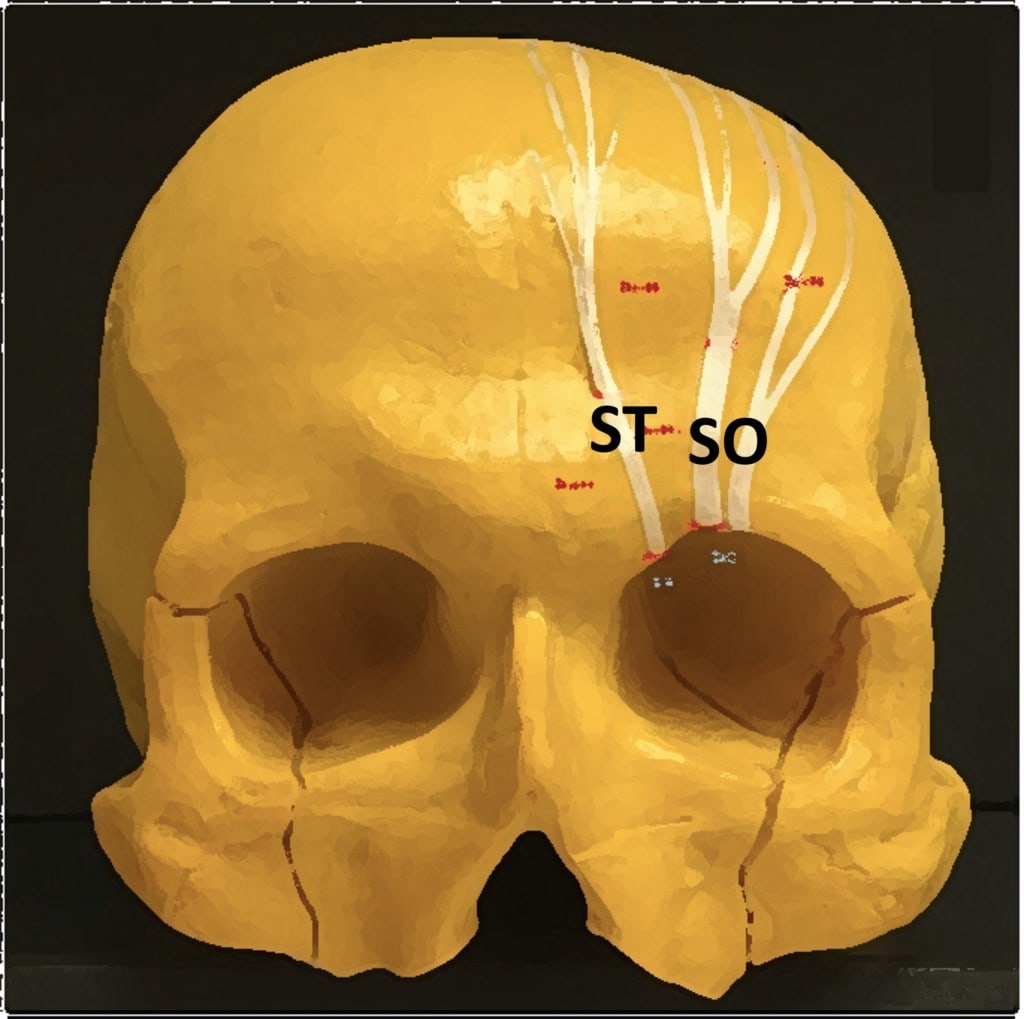
Frontal headache (pain in the front of the head) can be caused by irritation of the Supraorbital (SO) and Supratrochlear (ST) nerves that exit at the top of the eye socket. In particular, these can be irritated by a tight Frontalis muscle and these types of headaches are often treated with botox injections into this muscle. For diagnostic purposes, the doctor has to find the place that these nerves exit using ultrasound and block them at that those spots.
C2 Dorsal Root Ganglion
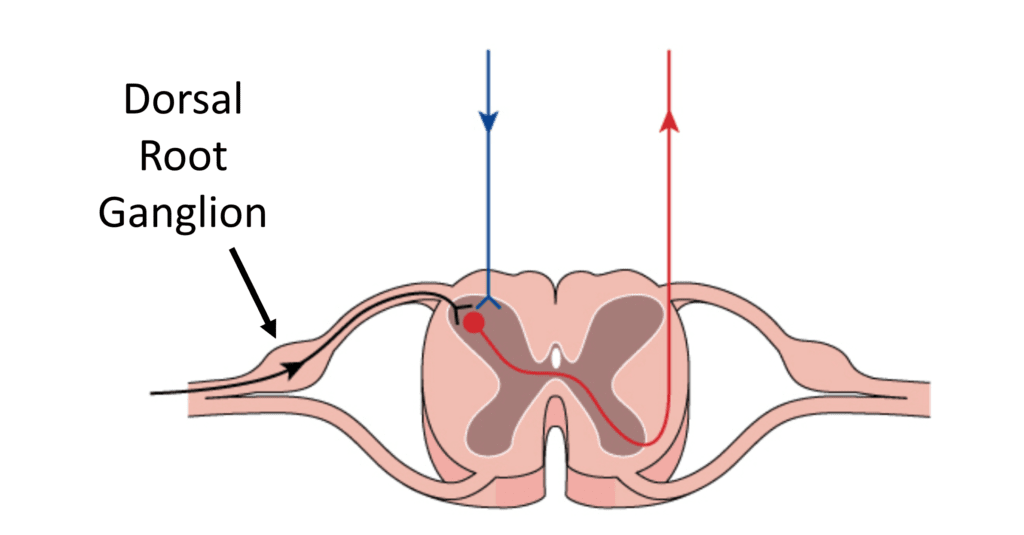
The Dorsal Root Ganglion is the sensory part of the spinal nerve. This nerve can be irritated by Craniocervical Instability, a bone spur in the upper neck bones, or arthritis in the C1-C2 facet joint. The headache will be in the back of the head and this nerve requires a careful and precise injection of numbing medicine using x-ray guidance and should only be performed by those physicians experienced in upper cervical injections.
Trigger Points
Muscles can refer pain to distant sites when a portion gets shortened and bunches up, something called a trigger point. Muscles like the Longus Colli, Splenius Capitis, Splenius Cervicis, and Sternocleidomastoid can refer pain to various parts of the head and neck. This diagnosis can be made with trigger point numbing injections which require ultrasound guidance in some cases.
Where Can You Get This Type of Workup?
The good news is that most experienced spine interventionists who routinely use ultrasound and fluoroscopy (x-ray) guidance should be able to perform this complete work-up. The bad news is that few seem to take the time. Hence, now armed with the complete list, you can now make sure all of it gets done.
If You Find the Right Spot, How Is That Treated?
Once the offending structure is found, today you should expect a regenerative medicine approach first. Meaning, something is injected that can help healing. That can be Platelet-Rich Plasma, Platelet Lysate, stem cells, etc… It’s also possible to use Radiofrequency Ablation (RFA) in some of these spots, but the issue is that killing the nerve (which is what RFA does) should only come after attempts at healing the nerve have failed. Steroid injections can also be tried, but again, this has downsides like toxicity to local cells.
The upshot? As you can see, a proper diagnostic block workup for headaches coming from the neck (or head structures) is complex. That’s why this full workup rarely gets done. However, now you know what you should expect. In the end, knowledge is power!

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
