Understanding Eagle Syndrome Causes, Symptoms, And Treatment Options
Eagle syndrome has drawn increasing interest from patients, with many experiencing symptoms that may resemble those caused by this condition. But what exactly is Eagle syndrome, and what are its treatment options? Let’s explore its causes, symptoms, and available treatments.
What Is Eagle Syndrome?
Eagle syndrome, first described in 1949, occurs when the styloid process (a bone at the base of the skull) becomes elongated and compresses nearby nerves or blood vessels. This can result in symptoms such as throat pain (ranging from dull and nagging to severe), difficulty swallowing, and neck, jaw, or ear pain.
Additional symptoms may include tinnitus (ringing in the ears) or increased discomfort during head movements, such as turning the head or chewing. This condition affects women more than men and is rare, with an incidence of 4–8 per 10,000 people.
Where Does Eagle Syndrome Occur?
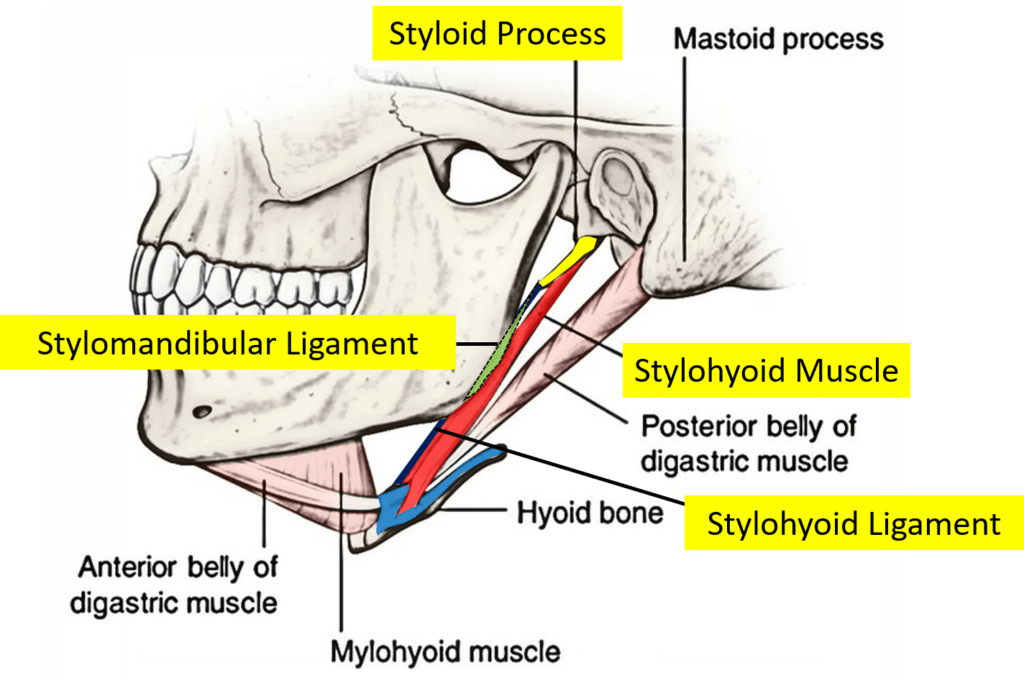
The styloid process plays a central role in Eagle syndrome. It is a bony projection located at the base of the skull, just in front of and below the ear (illustrated in yellow). It connects to the stylohyoid muscle (red), which attaches to the hyoid bone (blue). The styloid process also connects to muscles that extend to the tongue (styloglossus) and the back of the throat (stylopharyngeus).
The stylohyoid ligament links the styloid process to the hyoid bone, while the stylomandibular ligament connects it to the jawbone. These ligaments, along with several muscles, are crucial for functions like swallowing and jaw movement. This region is anatomically complex, with the styloid process vital in connecting various structures.
In addition to these ligaments and muscles, several important blood vessels and nerves are located near the styloid process. The internal jugular vein, internal carotid artery, and nerves such as the glossopharyngeal nerve (CN IX), vagus nerve (CN X), and accessory nerve (CN XI) run along its inner side.
The occipital artery, hypoglossal nerve (CN XII), and facial nerve (CN VII) are present on the outer side. The trigeminal nerve (CN V) is also situated nearby, making this area sensitive to any changes or elongation of the styloid process.
Why Is The Styloid Process Elongated?
The exact cause of styloid process elongation is not entirely understood. However, it is believed that chronic conditions affecting the jaw or neck, such as temporomandibular joint (TMJ) dysfunction, may exert excessive force on the ligaments and muscles attached to the styloid process. Over time, this strain may cause the bone to elongate.
Additionally, the stylohyoid ligament, which is normally flexible, may ossify (harden into bone) due to wear and tear, further contributing to the elongation of the styloid process.
What Causes Eagle Syndrome?
Eagle syndrome can develop from various anatomical changes or medical events that affect the structures of the neck and skull. These changes may lead to compression or irritation of nearby nerves and blood vessels, resulting in the symptoms associated with the condition. Some key factors that contribute to Eagle syndrome include the following:
Elongation Of The Styloid Process
A primary cause of Eagle syndrome is the abnormal elongation of the styloid process. While the exact cause remains unclear, elongation may occur naturally due to genetic predisposition or as part of the normal aging process, where the bone thickens and lengthens over time.
In some cases, trauma to the neck or skull may trigger excessive bone growth as a healing response, leading to the development of Eagle syndrome.
Tonsillectomy
Eagle syndrome may sometimes occur following a tonsillectomy, a surgical procedure to remove the tonsils. Post-surgical changes, such as scar tissue formation or shifts in nearby anatomical structures, may create pressure on nerves or the elongated styloid process, contributing to the onset of symptoms.
Calcification Of The Stylohyoid Ligament
The stylohyoid ligament, which connects the styloid process to the hyoid bone and aids in swallowing and speech, can sometimes undergo calcification. This process causes the ligament to harden and lose flexibility.
When calcification occurs, the stiffened ligament may pressure nearby nerves and blood vessels, particularly when combined with an elongated styloid process, intensifying symptoms such as throat, neck, or face discomfort.
What Otherwise Could Be Causing Your Symptoms?
Many other conditions can cause neck pain that are far more common than Eagle syndrome. These include damaged neck joints, pinched nerves, loose ligaments, and muscle irritation.
Additionally, conditions like temporomandibular joint (TMJ) syndrome and trigeminal neuralgia may cause facial pain, while lesions in the throat can contribute to throat pain. Considering these other potential causes is essential when evaluating symptoms similar to those of Eagle syndrome.
Symptoms of Eagle Syndrome
Eagle syndrome occurs when the elongated styloid process irritates nearby nerves, leading to various symptoms. Common sensations experienced by patients include:
- Tongue Spasm – This can result from irritation of the nerves that control tongue movement.
- Throat Pain – Irritation of the glossopharyngeal nerve (which supplies the back of the throat and tongue) or the hypoglossal nerve (responsible for tongue movement) can cause significant discomfort.
- Facial Pain – This may occur due to irritation of parts of the facial nerve or the trigeminal nerve, both of which are involved in facial sensations.
- Recurrent, Dull, And Throbbing Pain – Many patients report persistent, dull ache that can vary in intensity and often worsens with certain movements or activities.
Do Other Things Cause These Symptoms?
Yes, many other conditions can produce symptoms similar to Eagle syndrome. While only about 4% of individuals with an elongated styloid bone experience symptoms, many of these symptoms may be caused by other underlying issues.
It is important to understand this distinction, even if it may feel discouraging after believing you’ve found the cause of your discomfort.
One of the most common overlapping conditions is craniocervical instability (CCI). In CCI, the cranial nerves can become irritated due to loose ligaments that fail to properly support the head, allowing excessive skull movement on the spine. This irritation often mirrors the symptoms of Eagle syndrome, affecting the same nerves where they exit the skull.
In these cases, removing part of the styloid bone may not alleviate symptoms, as the source of the problem lies elsewhere.
We have also encountered numerous patients diagnosed with Eagle syndrome who have undergone surgery to remove their styloid bone, only to find that their symptoms persisted or even worsened. This highlights the importance of seeking expert evaluations and considering all possible causes before proceeding with surgical interventions.
Diagnosing The Condition Accurately
An accurate diagnosis is essential for addressing potential causes of discomfort related to Eagle syndrome. Physicians in the licensed Regenexx network use a comprehensive approach when evaluating musculoskeletal conditions, including cases involving the cervical region.
By assessing a patient’s symptoms, medical history, and performing a thorough physical examination, physicians can determine whether Eagle syndrome or another musculoskeletal issue may be contributing to discomfort. Key diagnostic techniques include the following:
Review Of Medical History
A detailed review of the patient’s medical history is one of the first steps in diagnosing Eagle syndrome. This helps physicians of the licensed Regenexx network identify any prior medical procedures, trauma, or conditions that may have contributed to the development of the condition.
Understanding these factors allows physicians to assess potential causes better and tailor the diagnostic process accordingly.
Physical Examination
During a physical examination, physicians of the licensed Regenexx network carefully palpate the throat, neck, and jaw to detect any tenderness or abnormalities that may be associated with an elongated styloid process or other related conditions. This hands-on assessment helps identify the potential causes of the patient’s symptoms and guides further diagnostic steps.
Imaging Techniques
Advanced imaging techniques are essential for confirming a diagnosis of Eagle syndrome, as they provide detailed visuals of the styloid process, surrounding structures, and any areas of compression or irritation.
- Computed tomography (CT) scan: A CT scan is commonly used to evaluate the elongation of the styloid process and its relationship to nearby anatomical structures. This high-resolution, cross-sectional imaging allows measuring the styloid process and identifies any abnormalities that may contribute to the condition.
- Computed tomography (CT) angiogram: A CT angiogram is a specialized imaging technique that uses contrast dye to visualize blood vessels in detail. This method is especially useful when Eagle syndrome may affect blood flow due to compression of nearby arteries. The angiogram helps detect vascular involvement, such as narrowing or compression of blood vessels, which can assist in guiding treatment decisions.
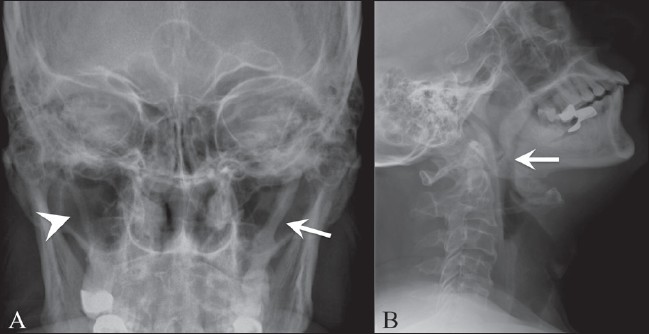
The first indication of Eagle syndrome is typically an elongated styloid process observed on an X-ray. A normal styloid process is about 25mm (1 inch) long, while a styloid process longer than 30mm is considered abnormal. However, it’s important to proceed with caution.
Approximately 4-7% of the general population has a long styloid process, yet only 4% of this percentage experience symptoms.
However, a highly accurate test to determine whether a long styloid process is causing symptoms does not currently exist. Diagnosis is typically based on a combination of imaging, such as X-rays or CT scans, and the patient’s reported symptoms.
One diagnostic option involves an ultrasound-guided or X-ray-guided numbing injection. While not definitive, this test can help determine whether surgery might alleviate your symptoms. It is crucial to consult a qualified expert who is experienced in performing this procedure.
A positive response, where your pain and symptoms subside for several hours, may suggest that the elongated styloid process is contributing to your discomfort.
Conventional Treatment Options For Eagle Syndrome
Several conventional treatment options are available for managing Eagle syndrome. Depending on the severity of the condition and the specific symptoms, your physicians may recommend the following conventional treatment options:
- Painkillers (Analgesics) – Over-the-counter or prescription painkillers, such as ibuprofen or acetaminophen, can help alleviate pain and inflammation caused by the elongated styloid process.
- Lidocaine Injections – Lidocaine injections offer temporary pain relief by numbing the area around the styloid process or the affected nerves. This minimally invasive treatment is often used for short-term symptom management or as a diagnostic tool.
- Styloidectomy – A styloidectomy is a surgical procedure that removes or shortens the elongated styloid process, relieving pressure on nearby nerves and blood vessels. This procedure offers a long-term solution for Eagle syndrome and may be recommended when other conservative treatments are not working.
Does Surgery Work?
The outcomes of surgery for Eagle syndrome are not well established, as no gold-standard randomized controlled trials are comparing surgical outcomes with non-surgical approaches. However, some lower-level studies suggest that surgery may provide relief for certain patients.
Surgical procedures in this area of the body involve working near numerous nerves and blood vessels, which may carry potential risks. Possible complications include:
- Localized infection, which may require IV antibiotics and/or additional surgery
- Trigeminal neuralgia, a condition that can cause increased facial pain due to nerve damage
- Vascular injury, which can result in severe bleeding and may require microsurgical repair of blood vessels
- Facial paralysis, resulting from injury to the facial nerve
Given these factors, individuals considering surgery may benefit from consulting with experienced medical professionals to explore all available options.
Additionally, messages warning of severe complications—such as the risk of stroke or blood vessel damage if the styloid bone is not removed—can sometimes be part of surgical sales techniques.
While patients with severe cases may face additional risks, clinical experience suggests that, for the vast majority of patients, the risk of removing the bone may outweigh the potential complications of an elongated styloid process.
An increasing number of patients are being advised to undergo surgery for Eagle syndrome. However, based on clinical analysis, many of these patients have a long styloid process but likely suffer from other causes of neck pain. Seeking expert advice and obtaining multiple opinions before considering invasive surgery is crucial.
Exploring Non-Surgical Options
Are there non-surgical ways to alleviate discomfort? Usually, yes. A thorough evaluation can help determine whether symptoms are related to an elongated styloid process or another underlying factor.
If the pain is due to a neck issue, such as a spinal problem, rather than the elongated styloid process, a variety of non-surgical treatments may be beneficial. It’s important to note that 96% of patients with a long styloid process do not have Eagle syndrome, meaning surgery may not be necessary for most individuals.
The Regenexx Approach For Eagle Syndrome
Physicians in the licensed Regenexx network offer non-surgical options that may help manage symptoms by targeting affected structures through image-guided procedures. Using comprehensive diagnostics, they may recommend interventional orthobiologic approaches, including injectates prepared with Regenexx lab processes, such as platelet-rich plasma (PRP) or bone marrow concentrate (BMC).
Procedures using Regenexx injectates are designed to support the body’s natural repair process and may help promote joint and tissue function.
For individuals seeking alternatives to surgery, the Regenexx approach offers a less invasive option focused on supporting mobility and overall joint health.
____________________________________
References:
(1) Ceylan A, Köybaşioğlu A, Celenk F, Yilmaz O, Uslu S. Surgical treatment of elongated styloid process: experience of 61 cases. Skull Base. 2008;18(5):289-295. doi:10.1055/s-0028-1086057
(2) Anuradha V, Sachidananda R, Pugazhendi SK, Satish P, Navaneetham R. Bilateral Atypical Facial Pain Caused by Eagle’s Syndrome. Case Rep Dent. 2020 Feb 25;2020:3013029. doi: 10.1155/2020/3013029. PMID: 32181021; PMCID: PMC7063204.
(3) Saccomanno S, Greco F, DE Corso E, et al. Eagle’s Syndrome, from clinical presentation to diagnosis and surgical treatment: a case report. Acta Otorhinolaryngol Ital. 2018;38(2):166-169. doi:10.14639/0392-100X-1479
(4) Gokce C, Sisman Y, Sipahioglu M. Styloid Process Elongation or Eagle’s Syndrome: Is There Any Role for Ectopic Calcification?. Eur J Dent. 2008;2(3):224-228.
(5) K. C. Prasad, M. P. Kamath, K. J. M. Reddy, K. Raju, and S. Agarwal, “Elongated styloid process (Eagle’s syndrome): a clinical study,” Journal of Oral and Maxillofacial Surgery, vol. 60, no. 2, pp. 171–175, 2002.
(6) M. Ilgüy, D. Ilgüy, N. Güler, and G. Bayirli, “Incidence of the type and calcification patterns in patients with elongated styloid process,” Journal of International Medical Research, vol. 33, no. 1, pp. 96–102, 2005.
(7) T. Jung, H. Tschernitschek, H. Hippen, B. Schneider, and L. Borchers, “Elongated styloid process: when is it really elongated?” Dentomaxillofacial Radiology, vol. 33, no. 2, pp. 119–124, 2004.
(8) Sundaram S, Punj J. Randomized Controlled Trial Comparing Landmark and Ultrasound-Guided Glossopharyngeal Nerve in Eagle Syndrome. Pain Med. 2020 Jun 1;21(6):1208-1215. doi: 10.1093/pm/pnz370. PMID: 32167550.
(9) Blackett JW, Ferraro DJ, Stephens JJ, Dowling JL, Jaboin JJ. Trigeminal neuralgia post-styloidectomy in Eagle syndrome: a case report. J Med Case Rep. 2012 Oct 2;6:333. doi: 10.1186/1752-1947-6-333. PMID: 23031688; PMCID: PMC3492092.
(10) Pigache P, Fontaine C, Ferri J, Raoul G. Transcervical styloidectomy in Eagle’s syndrome. Eur Ann Otorhinolaryngol Head Neck Dis. 2018 Dec;135(6):433-436. doi: 10.1016/j.anorl.2018.05.001. Epub 2018 Aug 31. PMID: 30174260.
