Why a Normal MRI Report May Be an Increasingly Dangerous Thing…
We see patients every day who have normal MRI’s and pain and patients who have abnormal MRI’s and little pain. I’ve blogged about this extensively. Given that, for orthopedic imaging, a well-trained and observant physician can usually find more than the reading radiologist and also knows where to look, reading the MRI personally is a key part of establishing a diagnosis. Regrettably, most of my colleagues don’t read their own films and rely on the radiology report. This morning I’ll show you why this is a problem and also talk about how changes in pain nomenclature will make the lives of pain patients everywhere much worse. In essence, by trying to seek a simple label, one large organization is creating a way for armies of providers to misdiagnose patients.
First, an Example of Why Relying on the Radiology Report Can Be a Bad Idea…
The patient I’d like to introduce today has turned his left ankle a few times and has recently begun to get lateral ankle pain. He underwent an MRI, which was read out by the radiologist as normal, so based on the report, there’s nothing wrong with that ankle. Right? Wrong! In fact, actually performing an exam, looking at the images, and performing additional stress imaging shows that the radiologist completely missed the diagnosis.
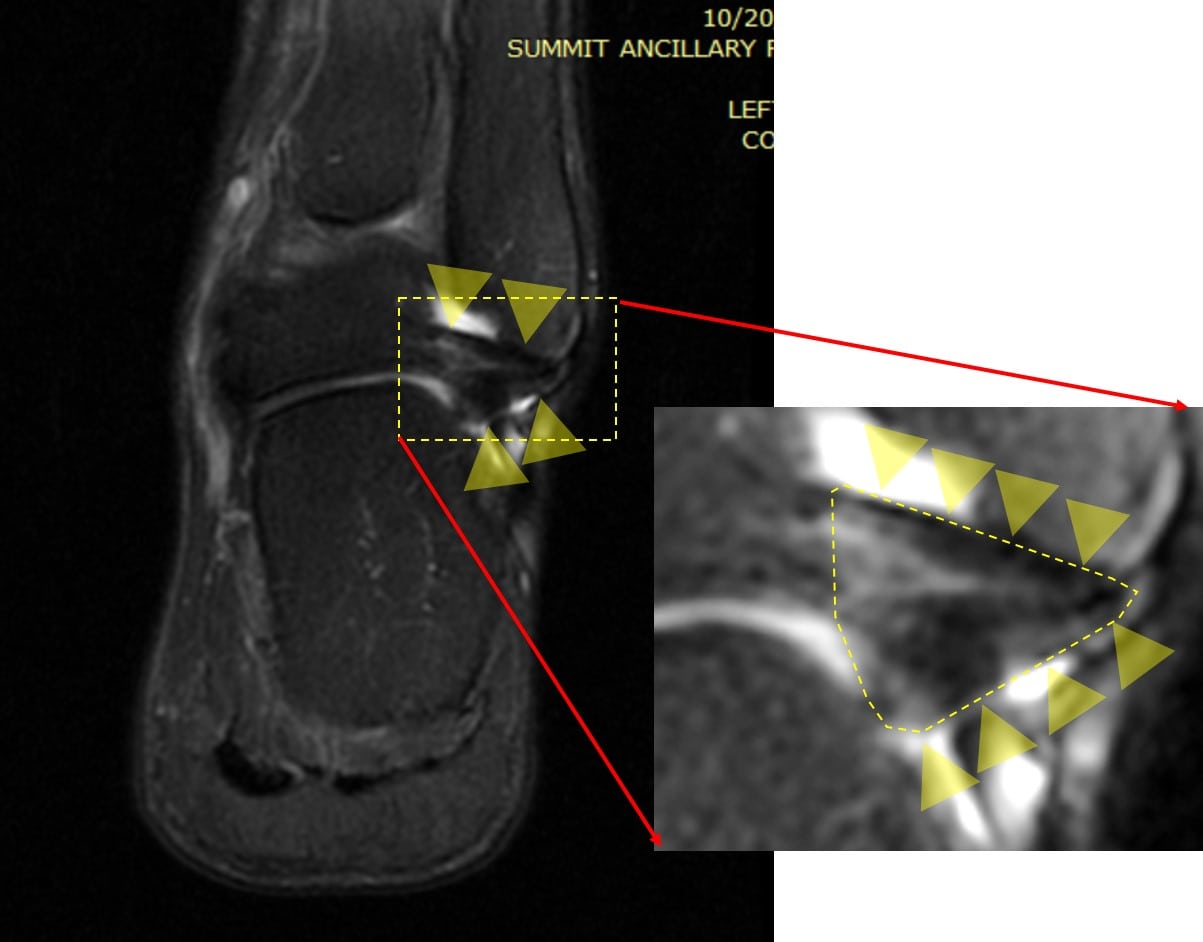
First, the MRI image below is looking at the front of the ankle and shows a mix of the calcaneofibular and talofibular ligament. These are outside ankle ligaments that hold the joint together and are commonly sprained. These ligaments are outlined by the yellow arrowheads:
The blown-up area on the right defines those ligaments with the dashed yellow lines. They are further highlighted by the yellow arrowheads. A normal ligament should be uniformly dark. However, notice the white areas in the triangle-shaped ligament. These are not normal and suggest that there may be small tears in the ligament.
New Imaging Technologies Find the Problem
The ligaments that hold your joints together are like pieces of strong duct tape. The most accurate way to find out about if they’ve been damaged is simple and the same way you would test two blocks if you had taped them together. You would try to move one block on the other to determine if the duct tape was holding. While you could also inspect the duct tape by looking at it, the best test is always to stress the bond to see if it’s strong. The same holds true with the ligaments in your body.
Taking an MRI of a ligament gives you a picture, as above. By more carefully inspecting the ligament on the image, it looks like there may be a damaged ligament. However, if I really want to see if the ligament has an issue, I have to stress it. To do this, ultrasound works well. I can see the ligament and the bones while I try to pry them apart. This is what I did below:
Note that I have what looks like two mountains separated by a valley. Each mountain is actually a bone labeled with a letter (“F” for fibula and “C” for calcaneus). The ligament lives in the valley and is labeled “L” for ligament. On the left, the two mountains come apart as I try to pry the bones apart. This is NOT normal and represents a damaged ligament consistent with the MRI image. The two mountains on the right don’t come apart, so this is a normal ligament on his asymptomatic side.
In summary, this guy never really had a normal MRI. His ligaments are clearly damaged. In the past, this was just bad medicine and could be written off as problems with an imperfect care system. However, now one of the major pain-management organizations wants to rewrite the nomenclature that would describe what’s wrong with this guy. This will take his missed diagnosis from a nuisance to a big problem. Why? The new naming system will blame it all on his overactive nerves, giving him a new false diagnosis and ensuring that his ankle slowly deteriorates into severe arthritis over the next decade. Let me explain.
The New Nomenclature
The IASP is an international organization that is largely an academic group of pain researchers. As I have blogged, there’s a bizarre new twist on the 1980’s concept that chronic pain is “all in the head.” Due to new research confirming that some patients in chronic pain have overactive nerves and the fact that this can be treated with expensive drugs, pharma, coming off hits like the nerve-pain drug Lyrica, has been pushing for more patients to be classified as having overactive nerves. In addition, physical therapists who are profiting off the lucrative medical education market have begun to teach a generation of providers that if patients have overactive nerves, all they need is psychological counseling to solve their perceived disability. So we have a perfect storm setting up a change in how to diagnose pain.
The new term proposed by IASP is nociplastic pain. This is the definition:
“Nociplastic pain*
Pain that arises from altered nociception despite no clear evidence of actual or threatened tissue damage causing the activation of peripheral nociceptors or evidence for disease or lesion of the somatosensory system causing the pain.”
Yikes, that’s some super-dense researcher speak, so let me translate. In patients who don’t have a clear diagnosis of why they hurt, the doctor can label them as having overactive nerves. I’m hoping that you can see how this impacts our patient with the normal ankle MRI whose ankle hurts when he walks. Given that few physicians would have ever known to perform a stress ultrasound exam of his ankle and almost all would have believed the radiology report that there was nothing wrong (and never looked at the images themselves), our poor patient would have eventually been labeled with nociplastic pain. He would have either been placed on nerve-pain medication or sent to a physical therapist to talk him out of pain. In the meantime, all he really needs is a precise guided injection of PRP to help heal the damaged ligament. In addition, if the ligament stays lax because of a missed diagnosis, his ankle joint will eventually get damaged and become arthritic. So you get the picture of how this new term is very dangerous for patients whose doctors will think that a normal MRI equals no problems and who never take the time to investigate further.
The upshot? We don’t need more terms for pain. We need to educate providers on how to diagnose what’s wrong with the musculoskeletal system. In the meantime, if your doctor can’t read an MRI in front of you or doesn’t know how to use ultrasound, you need to run!

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.