Why Most Fat Stem Cells Harvested via Liposuction are DOA…
Stem cells are very sensitive to certain medications that physicians commonly use. One of the known medication problem areas is local anesthetics. Fat stem cells are harvested via liposuction where large amounts of anesthetic are used. Now a new study shows that the most common local anesthetic used kills fat stem cells dead.
There are stem cells in your fat and there are new clinics springing up all the time offering to hoover that fat out and isolate the stem cells for clinical use. The most common process of taking the fat is called tumescent liposuction. This is where the doctor takes large volumes of dilute local anesthetic and injects it into the fat tissue with a solution of epinephrine (adrenaline) to constrict the blood vessels. Since liposuction by it’s very nature involves breaking up large stretches of tissue (i.e. the fat doesn’t just vacuum out), the lidocaine anesthetic helps the pain and the epinephrine reduces the bleeding in what would otherwise be a very bloody procedure.
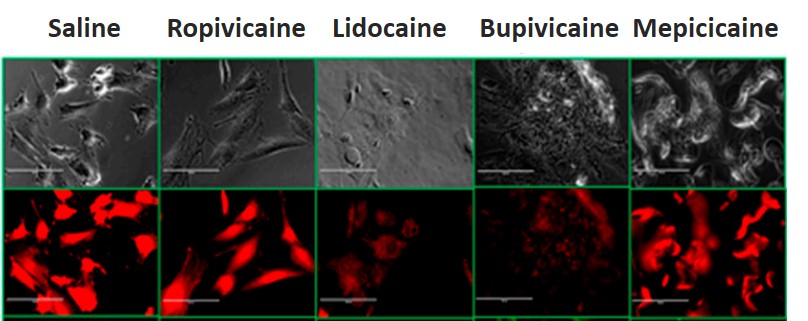
Local anesthetics are a problem for stem cells. We first found this out in 2007. Last year, our research team published a study looking at several anesthetics with human mesenchymal stem cells and found that the two most commonly used, lidocaine and marcaine (bupivicaine), are quite toxic to stem cells. This is even at low concentrations. To get a visceral understanding of how bad these effects can be, rather than showing graphs, take a look at the microscope pictures below. The bottom strip shows stem cells being lit up in our research lab by fluorescent microscopy. Note that for the saline control (salt water) and for Ropivicaine (an anesthetic commonly used in labor and delivery wards), the stem cells stay a robust reddish orange against the black background, indicating good health. However, when the cells are exposed to lidocaine and bupivicaine (the two most commonly used anesthetics today), the color goes away (meaning the cells are dead or dying).
The study looked to see if the most commonly used technique to harvest fat stem cells (used by 99% of all physicians who use fat stem cells), hurt the cells. The authors performed liposuction on middle aged women and then exposed the cells to conditions that mimicked either local anesthesia or the type of tumescent anesthesia discussed above. While the study demonstrated more stem cells in the tumescent group, those cells were killed off in a dose dependent manner by lidocaine. In addition, the lidocaine was causing the stem cells to go toward pre-programmed cell death (apoptosis).
The upshot? The most commonly used technique to harvest stem cells from fat kills stem cells. We’ve been warning our colleagues since 2007 when we first observed that the most commonly used liposuction anesthetic kills stem cells, not to use local anesthetics around stem cells. We finally published a paper on the topic to try to get the word out. However, many plastic surgeons and others using tumescent liposuction with lidocaine have sworn that they’ve gotten “good viability” of the cells. The issue with this statement is that the technology the clinics use to test the viability is not very sophisticated. In addition, since the clinics never culture the cells (the ultimate test of their health) because they don’t have that ability, they never truly get to see if the cells survive past a few hours. So while fat stem cells aren’t ideal for orthopedic uses, what do you do if you’re planning a fat stem cell procedure? If the doctor who is performing the procedure doesn’t know that lidocaine is a problem after this information has been publicly available for the last 5-7 years and now this new study…run…

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.