Yet Another ACL Surgery Avoided?
I don’t know how many MRIs we have now showing healing of ACL tears due to the Perc-ACLR procedure that we created. This is yet another one shown above. Let’s dig in.
The Past Version of How to Deal with an ACL Tear
ACL tears and subsequent ACL reconstruction (ACLR) surgery have been the bread and butter of orthopedic sports medicine for decades. In fact, if there ever was one surgery that defined that field due to its frequent use in athletes, ACLR would be it. That procedure involves ripping out the torn ligament, drilling graft tunnels, and then inserting a tendon to act as a ligament. ACLR has been associated with many unflattering research findings through the years including that it does nothing to prevent arthritis, causes a second hit to the cartilage, and leaves the knee more vulnerable to ACL retear.
Enter the Future in 2011
In around 2011, we began to inject the ACL with stem cells. At first, this was very tough to do, as there were no medical texts that showed how to do this procedure. Frankly, using x-ray guidance, it took about 1-2 years to figure out how to get the cells into the ligament reliably. Then it took another 2-3 years to figure out how to get the cells into all parts of the ligament. However, by 2015/2016 we had perfected the procedure and began logging a furious series of MRIs from before and after the procedure that showed amazing results of ligament healing. A compilation of those MRIs is in the video below:
How Could This Work?
The procedure uses bone marrow from the patient which is rich in mesenchymal stem cells. We further concentrate the stem cell fraction of that bone marrow aspirate in our advanced lab and then inject those cells into the damaged ACL. Based on the copious MRI evidence we have, the cells likely set up a healing reaction in the ligament and cause the damaged ligament tissue to heal. We have published two papers to date on the results and have just finished recruiting a randomized controlled trial (1,2).
The Main Differences Between the Two Procedures
A Surgical ACL Reconstruction (S-ACLR) is VERY different than a Percutaneous ACL Repair (perc-ACLR). First, one is surgery and the other is a precise image-guided injection, hence the side effect profile is obviously much lower for the injection. Second, the S-ACLR rips out the original equipment and replaces it with tendon that goes in at a steeper angle and can never replace the properties and position sensing ability of the native ligament. The perc-ACLR keeps that ligament and it’s position sensors.
However, Perc-ACLR can only successfully tackle about 2 in 3 patients that currently get surgery. Hence, the selection of patients is critical.
The New MRI
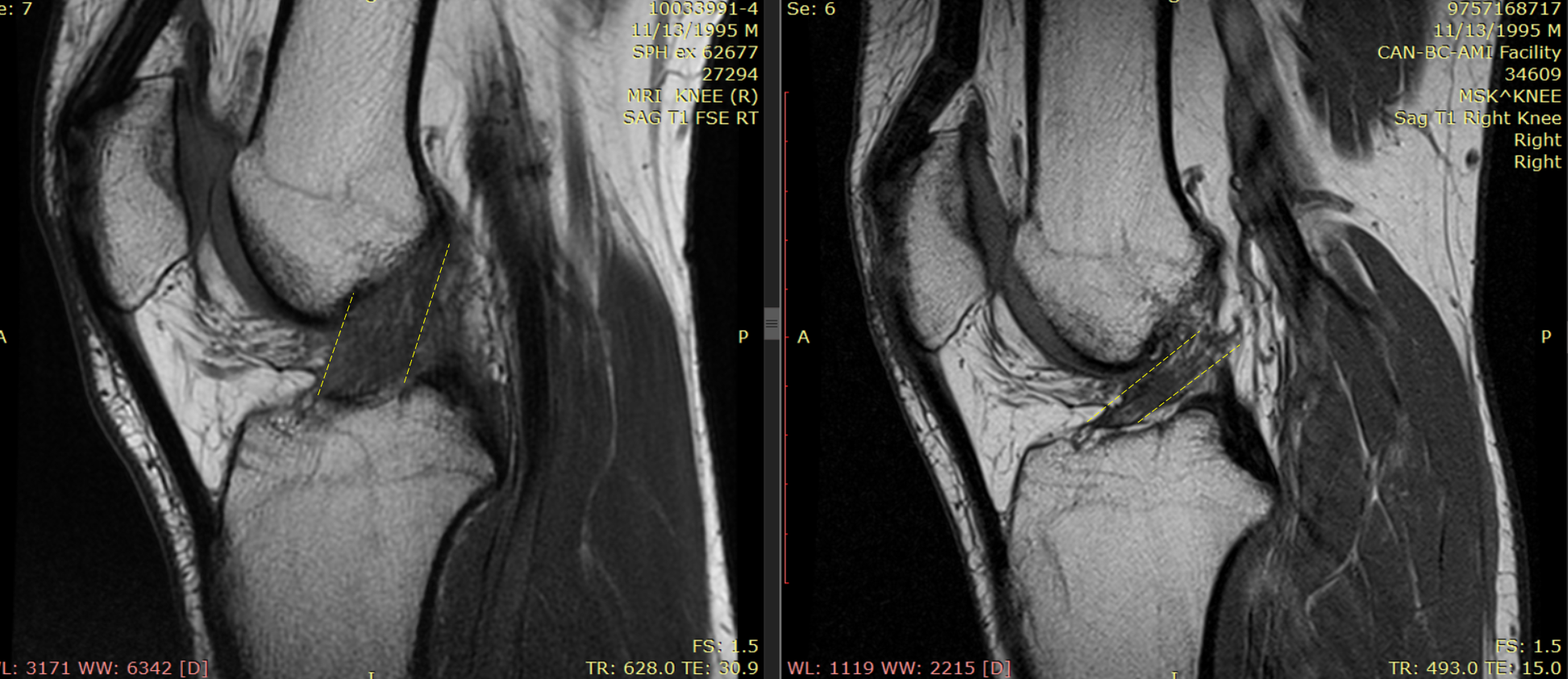
This patient is a 35-year-old international visitor to our Colorado facility who injured his ACL while playing sports in November of 2019. His MRI on the left shows a complete tear of the ACL (inside the yellow dashed lines). It’s gone from a darker dense ligament to this lighter “blown out” morphology. That’s an ACL surgery all day long here in the states, but he knew about our groundbreaking Prec-ACLR procedure so he flew here to get it done. In March, just before the world shut down, we performed a bone marrow aspiration and then precise fluoroscopy-guided injection of his own high dose bone marrow concentrate into the tears. His new MRI, which was taken some 4 months later, shows a dense and dark ligament with almost normal morphology (inside the yellow lines). He was cleared to get out of his brace and slowly begin working out at a higher level. That recovery will ultimately be about half the time of a surgical ACL repair. To see how this procedure is performed, check out my video below:
Beware of Fake ACL Stem Cell Procedures
As with anything in medicine, when something works due to hard work and advanced skills, those with fewer skills will try to copy it. Hence, a fake Prec-ACLR procedure is just like that Gucci purse you can buy for cheap on a street corner that will fall apart in a few months. Why?
The problem is that the real Perc-ACLR procedure takes many hundreds of hours of training and an expensive fluoroscopy unit to perform accurately. Just injecting the cells somewhere in the vicinity of the ACL won’t work. Using fake and dead amniotic or umbilical cord “stem cells” also won’t work.
The upshot? I’ve lost track of how many ACL tears we’ve healed with the Perc-ACLR procedure. As a physician, it’s personally gratifying to see these amazing before and after images. For patients, they get a procedure with less downtime and they get to keep their original equipment!
____________________________________________
(1) Centeno CJ, Pitts J, Al-Sayegh H, Freeman MD. Anterior cruciate ligament tears treated with percutaneous injection of autologous bone marrow nucleated cells: a case series. J Pain Res. 2015;8:437–447. https://www.ncbi.nlm.nih.gov/pubmed/26261424
(2) Centeno C, Markle J, Dodson E, et al. Symptomatic anterior cruciate ligament tears treated with percutaneous injection of autologous bone marrow concentrate and platelet products: a non-controlled registry study. J Transl Med. 2018;16(1):246. https://www.ncbi.nlm.nih.gov/pubmed/30176875

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
