Back Surgery Gone Bad: Did Your Stabilizing Muscles Get Fried?
What causes back surgery gone bad? There are many theories, but the answer may be sitting on your MRI film and may have never been read out. The issue may have been caused by an old school surgical technique. Let me explain.
There’s a lot of information on a low back MRI that’s often missed. Imagine if your big thigh muscle suddenly got 80% smaller. Could you walk? Would this be a big deal? It would of course be disabling, yet the same thing is happening to the stabilizing muscles of a large percentage of all patients with chronic low back pain and it goes completely unnoticed by most radiologists who didn’t get the memo that this was important. This is despite hundreds of peer reviewed articles showing the importance of this muscle atrophy. While I’m talking about the multifidus muscle, there’s another big issue concerning low back muscle loss I’d like to highlight this morning: long-term muscle damage due to retractors used in surgery.
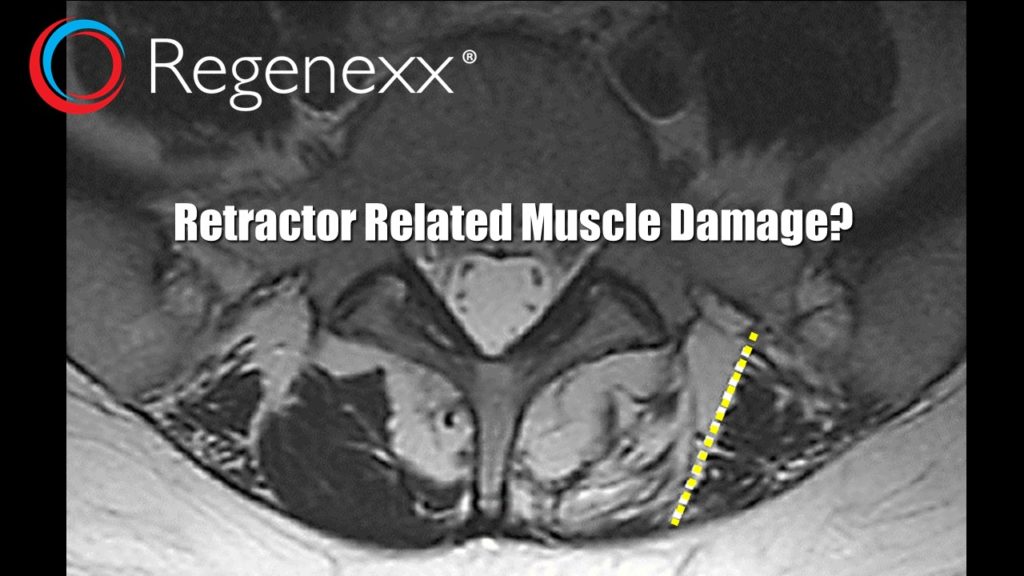
Yesterday a patient came in after two failed low back surgeries. She was miserable and spends a few days each month in bed when her back goes out. She and her husband were frustrated and demoralized, having dealt with this for years. One of the things that jumped out on her MRI was the epic amount of muscle loss. There was also a clue on the image as to what had happened to her low back muscles on the left – a straight line cut where the muscle was left and where it was gone. In the recent movie Prometheus, the crew of the ship spots a feature on the surface of a planet that doesn’t look natural and one of the characters says, “God doesn’t build in straight lines…” Indeed, this patient wasn’t born with this straight line on her MRI film – it was caused by her surgery. It’s commonly known as retractor damage (see dashed white line above). In the picture above, the dark stuff to the right of that line is surviving muscle, the white stuff to the left is where living muscle used to be and this has now been replaced by fat.
A retractor is a surgical instrument that holds tissue back so the surgeon can see and work in an area of the body. The instrument usually has a flat blade. Quite a bit of pressure is applied to the muscles and soft-tissue when a retractor is used. The concept that this can lead to low back muscle damage is well studied. Animal studies show that it’s from denervation (damage to the muscle nerve supply due to sustained pressure) and disuse of muscles that have been disconnected from their normal attachments sites onto back bones. In fact, smart surgeons in 2007 have studied that by just releasing the retractor every 15 minutes to let blood flow again in the nerves and muscles, the amount of muscle damage is lessened and that this correlates with less post-operative back pain! We can also go back to 2004 to find reports of studies that show that the length of time that the retractor is used is directly related to the muscle injury and residual back pain after surgery. In fact, the oldest scientific article on the subject I can find goes back to the early 1990s.
So why do we still see this type of post-surgical muscle damage? Many things in medicine change slowly. In addition, with the emphasis now being placed on efficiency, letting off a retractor every 15 minutes during a surgery has practical problems. For example, during a two hour procedure you would have to do this 8 times, with each break resulting in a field that needed to be re-established. In addition, in heavier patients where large amounts of fatty tissue are also being held back, it may take another 5-10 minutes just to get the same surgical field of view established.
So what can I do to avoid back surgery gone bad?
A few simple things….If you have chronic back pain after a surgery that unpredictably acts up, first get a qualified doctor to see if you have retractor related muscle damage. It’s pretty common, as I’ve seen two cases in my office in the last 6 weeks. If you need back surgery, consider advanced non-surgical options first. But if you still need the surgery, make sure beforehand that your surgeon is willing to release the retractors every 15 minutes to avoid this type of nerve and muscle damage!

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.