Hip Replacement vs Hip Resurfacing: Differences and Risks
One of the more successful marketing efforts in the world of joint replacements has been “hip resurfacing.” While it’s still a hip replacement, it just sounds so much sexier and less invasive. However, despite the Madison Avenue veneer, the procedure has had many problems that need to be understood when considering hip resurfacing instead of a hip replacement.
Hip Replacement vs Hip Resurfacing
Why would one consider a hip resurfacing instead of a hip replacement? At first blush, it’s because the hip resurfacing sounds less invasive. That also means fewer complications, right? Maybe not.
Alila Medical Media/Shutterstock
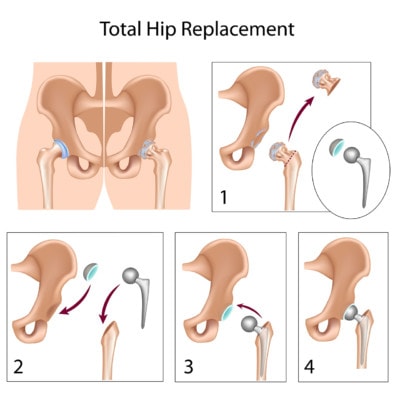
Hip replacement involves cutting off the proximal end, or the head, of the femur (the long bone of the leg that connects the knee to the hip). The hip is a ball-and-socket joint, and the socket side is a shallow process in the pelvic bone called the acetabulum. Cartilage and bone are shaved out of this socket, and an artificial socket made of metal or polyethylene, for example, is either cemented or screwed into place, and a liner is added to act as cartilage. A hole is then drilled vertically into the middle of the bone where a metal stem-like device is inserted, and a metal ball to form the head of the artificial hip is added to the stem.
A hip resurfacing involves replacing the acetabulum side of the hip joint, but the head of the femur is not removed. Instead, it is cut back, or resurfaced, and a cap is placed over the top of it. While hip resurfacing may be less extreme in literal terms, in that the head of the femur bone is not amputated, and have more rapid recovery times, it is still a highly invasive surgery associated with many complications. In fact, in some ways, it’s complication rates are higher than hip replacement.
The Problems with Hip Resurfacing
You’d think a seemingly less-involved hip surgery would have fewer complications, but, unfortunately, the literature isn’t supporting this. While there may be fewer patients experiencing problems in some cases, in other cases, the side effects of hip resurfacing are even worse. Let’s review.
Pseudotumors Following Hip Resurfacing
Pseudotumors are growths that resemble tumors on imaging. They are typically areas of fluid buildup, inflammation, or a tissue reaction of some type and can occur in many areas of the body. It’s not really clear what causes them; however, we know they are common following hip replacement. One study found as much as one-third of patients who undergo hip replacement then developing a pseudotumor. While they aren’t cancerous, they can be painful as they become inflamed and put pressure on the nerves and blood vessels around them.
Unfortunately, pseudotumors are also common in hip resurfacing patients, with one study finding that 28% of patients suffer from this complication. This same study found an even higher number of pseudotumors in hip replacement patients than the study in the paragraph above—over 40%—regardless of the material used in the replacement device. Patients with pseudotumors also experience more pain and poorer function following surgery.
Metal Particles Following Hip Resurfacing
I’ve also shared studies in the past that actually found poorer outcomes in some cases with hip resurfacing when compared to hip replacements. For example, higher levels of the metals chromium and cobalt have been found in the blood of patients following hip resurfacing than in those with a total hip replacement. These patients were also found on MRI to have changes to the structure of certain areas of their brain responsible for visual function. Even the FDA has issued warnings in the past about the metal particles that are shed from these hip resurfacing devices.
Early Failure of Hip Resurfacing Devices
One study (see prior link above) found that in females and males with smaller femoral heads, hip resurfacing wasn’t as effective as hip replacement, and in women, in particular, the hip resurfacing devices were failing, on average, about five years earlier than a hip replacement prosthetic. Even younger patients who opt for a hip resurfacing as a less extreme option fare no better with failure rates; in patients under age 55, five-year revision rates were nearly twice as much as those with a hip replacement.
The upshot? So when trying to choose between hip resurfacing and hip replacement, the decision shouldn’t be based on the perception that one seems less invasive. As you’ve seen, in many ways, the side effects are worse with hip resurfacing. In the meantime, our goal as a clinic is always to try to avoid the surgery altogether by using precise injections of the patient’s own platelets or stem cells.

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
