Is Multiple Dose PRP to Treat Knee OA Cost Effective for Health Plan Coverage vs Single Dose?

As the CMO for Regenexx, it’s my job to thread the needle between access to ground-breaking interventional orthobiologics treatments via a self-funded health plan and wasting an employer’s money by authorizing care that we know doesn’t work or doesn’t work well enough compared to traditional surgery. This past year, I have been asked several times by our network providers if they could pursue multiple injections of PRP since a few studies have suggested that this works better than a single shot to help knee OA. Hence, I thought I would take some time to look at this issue from a cost-outcome perspective. In other words, is it worth it to an employer to cover three shots versus one?
PRP For Knee OA
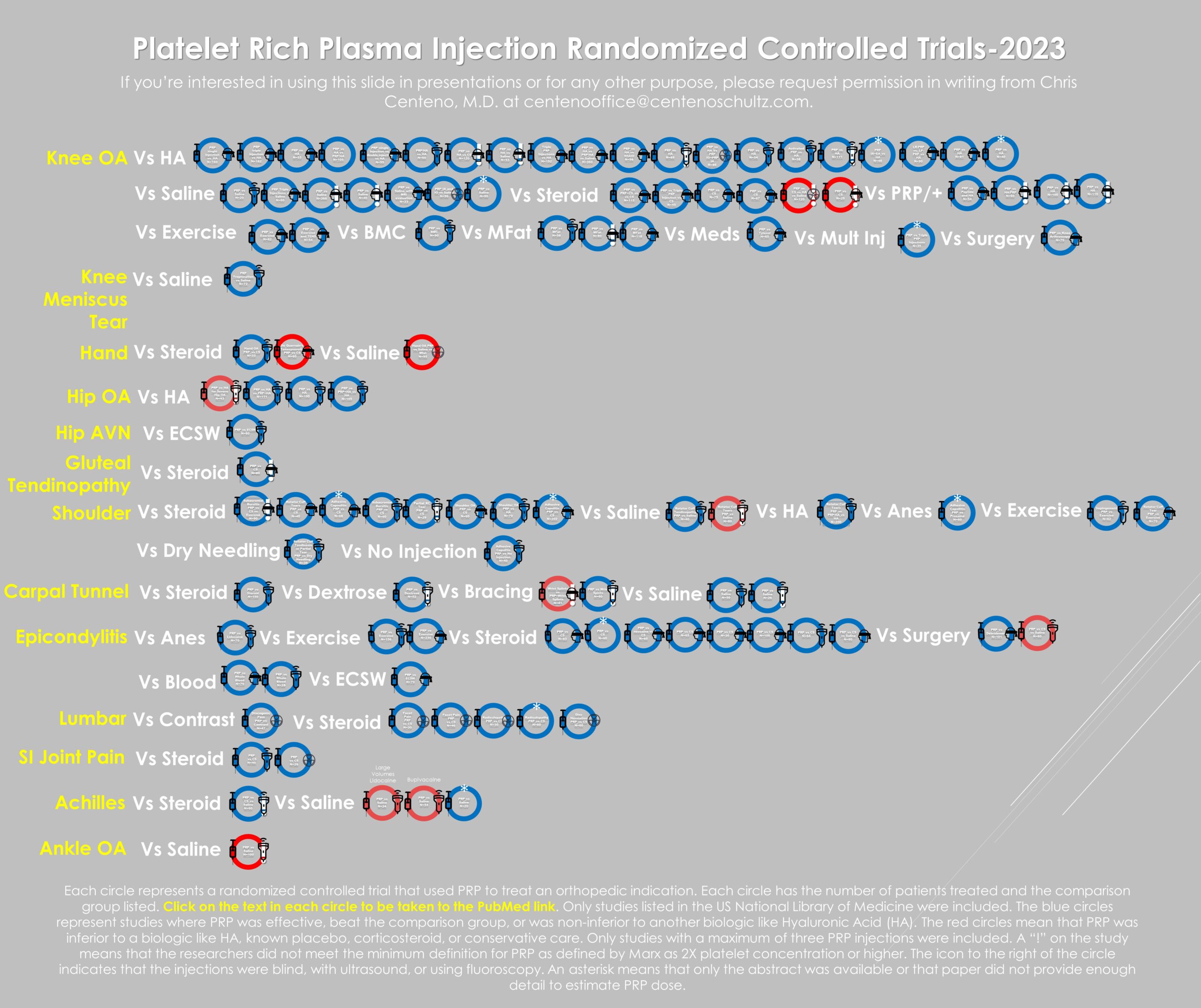
As you may know, I did an extensive literature review of the dozens of randomized controlled trials that support the efficacy of PRP used to treat knee OA. I also looked at a failure analysis based on the use of “fake PRP”. Meaning, that a huge factor in clinical trial failure was any study that used “PRP” less than 2X concentrated. That summary is linked above.
Reviewing the 1 Shot versus 3 Shot PRP Literature: Which Studies Actually Used PRP?
To start this review, I used a study published last year that performed a systematic review and meta-analysis (1). The first issue that’s obvious from looking at a table on PRP prep in this meta-analysis is that of the seven included studies, one used fake PRP:

In other words, based on blood drawn and injected and applying a platelet capture efficiency factor, the Subramanyam et al paper couldn’t have produced PRP that was more concentrated than 2X.
To make sure I was dealing with real PRP, I pulled the above papers to review methods:
- Patel began with 100 ml of whole blood and based on their description produced PRP>2X (2).
- Vilchez has never been published in a peer-reviewed setting and the references only point to a clinicaltrials.gov study design (3).
- Kavadar drew 30-40 cc of whole blood and ended up with 4-5 cc of PRP, which even with poor efficiency isolation meets the criteria for >2X (4).
- Guvendi shows us measured platelet concentration numbers which clearly exceed 2X (5).
- When looking at Simental in the table above, the authors state that there is no information on the PRP composition. This isn’t the case when you pull the paper. The authors state that the platelet concentration was 206% and 209%, so this paper just barely meets the criteria of having >2X PRP (6).
- Yurtbay took 32 ml of blood and ended up with 8 ml. Even with a poor platelet recovery system, the PRP is highly likely to be >2X (7).
This leaves 5 of the 7 papers that have both been published and used PRP at 2X or greater platelet concentration.
How Much Benefit Did You Get for Spending 3X as Much?
The next part of this analysis is how long the authors observed the outcome of these interventions. For example, is 6 months enough? From an economic standpoint, PRP is expensive enough that you would need at least one year of positive results. In addition, a 1-2 year mark would also be where you would want to see a three-shot injection routine separate from a one-shot. Hence, I excluded all studies without at least a year of data. This meant that since Kavadar, Guvendi, and Patel, only measured changes until 6 months, they were excluded.
How much improvement in outcome for 3 shots is worth it compared to one? My sense is that we can look at this in two different ways. The first is that the 3-shot protocol should produce at least 3 times the improvement. For example, if the one-shot protocol produced a 25% improvement in function, the three-shot had better produce at least 75%. However, another way to look at this is if the three-shot produces results that look more like disease modification. What might that look like? The improvement continues over time for a long time.
In getting into the above-referenced meta-analysis, its purpose wasn’t to look at the magnitude of the effect but instead, whether 3 PRP shots statistically beat 1 shot. However, we can look at the magnitude of the effect by pulling the data from the two papers left standing:

So of the two studies left, the magnitude of the effect is about 20-40%. That means that the improvement is 20-40% better with three shots over one. For the above graph, I used the Yurtbay outcome timepoint at 12 months as this showed the best separation between the two groups.
Does this Math Make Sense?
So we’re spending 3 times as much to get about 20-40% improvement in effect at 1-2 years. That math doesn’t seem to make sense, but is there more to this story? Let’s look at the Simental study results over two years:

Here we see that the 1 PRP shot group does well, but plateaus after 6 months, but that the 3 shot group continues to get better over two years. It should be noted that this is only 18 and 17 patients per group. This could also be a placebo effect, as one group knew they had three shots versus one group knew they only had one.
Is there a way we can get a sense of how a placebo effect would look in this type of treatment? It just so happens that Yurtbay has placebo groups for both the one-shot and three-shot protocols:
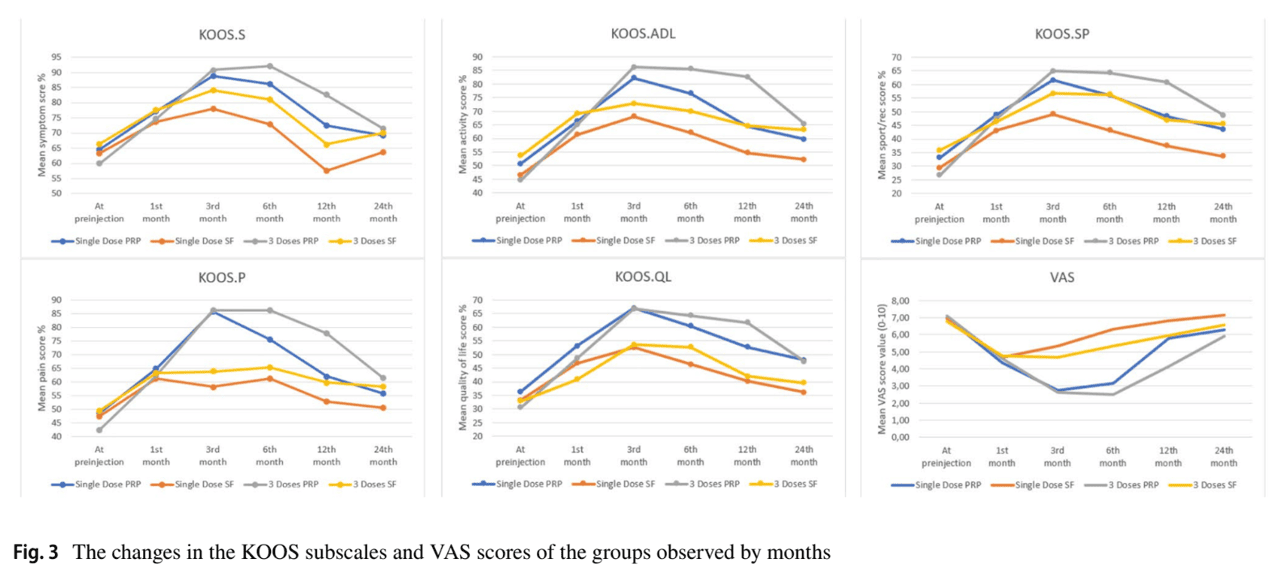
The above graphs from Turtbay do show some placebo effects between the 1 and 3 saline injection groups, but we also see that the two PRP groups do better than the two saline groups.
However, looking at these graphs from Yurbay, there’s another issue. We don’t see the outcome difference between 1 shot and 3 shots of PRP at two years as shown in Simental. Instead, the effects tend to wear off in both groups from the first year to the second. That could be because we’re looking at more patients here at about 50-60 in a group.
Do Either of These Studies Use Proper PRP Dosing for These Age Groups?
What is the proper dose of PRP for knee osteoarthritis? Our research group and others have looked at this issue (7-8). It’s likely that for PRP dose in older patients, more is better. In my clinical experience, concentrations for older patients should be in the at least 7X to 10X range. What were the concentrations used in these two studies?
- Simental-2X
- Yurtbay-If we apply a 50% platelet recovery which is typical we get 2X.
Hence, both of these studies severely underdosed these middle-aged and early elderly patients by using PRP that barely met the definition of 2X. What would these results look like if these patients had received 10X PRP?
The upshot? While the data on three versus one shot of PRP in one study looks promising, in another study with a larger n, that approach isn’t impressive. These data certainly don’t support that spending 3 times as much produces much better results. Perhaps more research on this topic where patients are properly dosed and taken out to two years will bolster one of these storylines. In the meantime, an employer looking to cover three PRP shots over one is likely wasting their health plan money.
_______________________________________
References:
- Tao X, Aw AAL, Leeu JJ, Bin Abd Razak HR. Three Doses of Platelet-Rich Plasma Therapy Are More Effective Than One Dose of Platelet-Rich Plasma in the Treatment of Knee Osteoarthritis: A Systematic Review and Meta-analysis. Arthroscopy. 2023 Dec;39(12):2568-2576.e2. doi: 10.1016/j.arthro.2023.05.018. Epub 2023 May 24. PMID: 37236291.
- Patel, Sandeep, et al. “Treatment with platelet-rich plasma is more effective than placebo for knee osteoarthritis: a prospective, double-blind, randomized trial.” The American journal of sports medicine 41.2 (2013): 356-364.
- Vilchez Cavazos F. Intra-articular injections of platelet-rich plasma in knee osteoarthritis: Unique application versus triple application. ClinicalTrials.gov identifier NCT02370420. https://clinicaltrials.gov/ct2/show/study/NCT02370420. Published February 25, 2015. Updated February 19, 2018. Accessed January 30, 2023.
- Kavadar G. Demircioglu D.T. Celik M.Y. Emre T.Y. Effectiveness of platelet-rich plasma in the treatment of moderate knee osteoarthritis: A randomized prospective study.
J Phys Ther Sci. 2015; 27: 3863-3867. - Güvendi E.U. Askin A. Güvendi G. Kocyigit H. Comparison of efficiency between corticosteroid and platelet rich plasma injection therapies in patients with knee osteoarthritis.
Arch Rheumatol. 2018; 33: 273-281. - Simental-Mendía M. Acosta-Olivo C.A. Hernández-Rodríguez A.N. et al. Intraarticular injection of platelet-rich plasma in knee osteoarthritis: single versus triple application approach. Pilot study. Acta Reumatol Port. 2019; 44: 138-144.
- Yurtbay A. Say F. Çinka H. Ersoy A. Multiple platelet-rich plasma injections are superior to single PRP injections or saline in osteoarthritis of the knee: The 2-year results of a randomized, double-blind, placebo-controlled clinical trial. Arch Orthop Trauma Surg. 2022; 142: 2755-2768
- Berger DR, Centeno CJ, Steinmetz NJ. Platelet lysates from aged donors promote human tenocyte proliferation and migration in a concentration-dependent manner. Bone Joint Res. 2019 Feb 2;8(1):32-40. doi: 10.1302/2046-3758.81.BJR-2018-0164.R1. PMID: 30800297; PMCID: PMC6359887
- Bansal, H., Leon, J., Pont, J.L. et al. Platelet-rich plasma (PRP) in osteoarthritis (OA) knee: Correct dose critical for long term clinical efficacy. Sci Rep 11, 3971 (2021). https://doi.org/10.1038/s41598-021-83025-2
Originally published on

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.