Meniscus Tear MRI? – Please Read This
Key points:
- Meniscus tears in middle-aged or older people are as important as wrinkles – they are a sign of normal aging
- New research shows that all sorts of once serious findings exist in the knees of patients without pain
- Many studies now show that the most commonly used surgery to treat meniscus tears doesn’t work
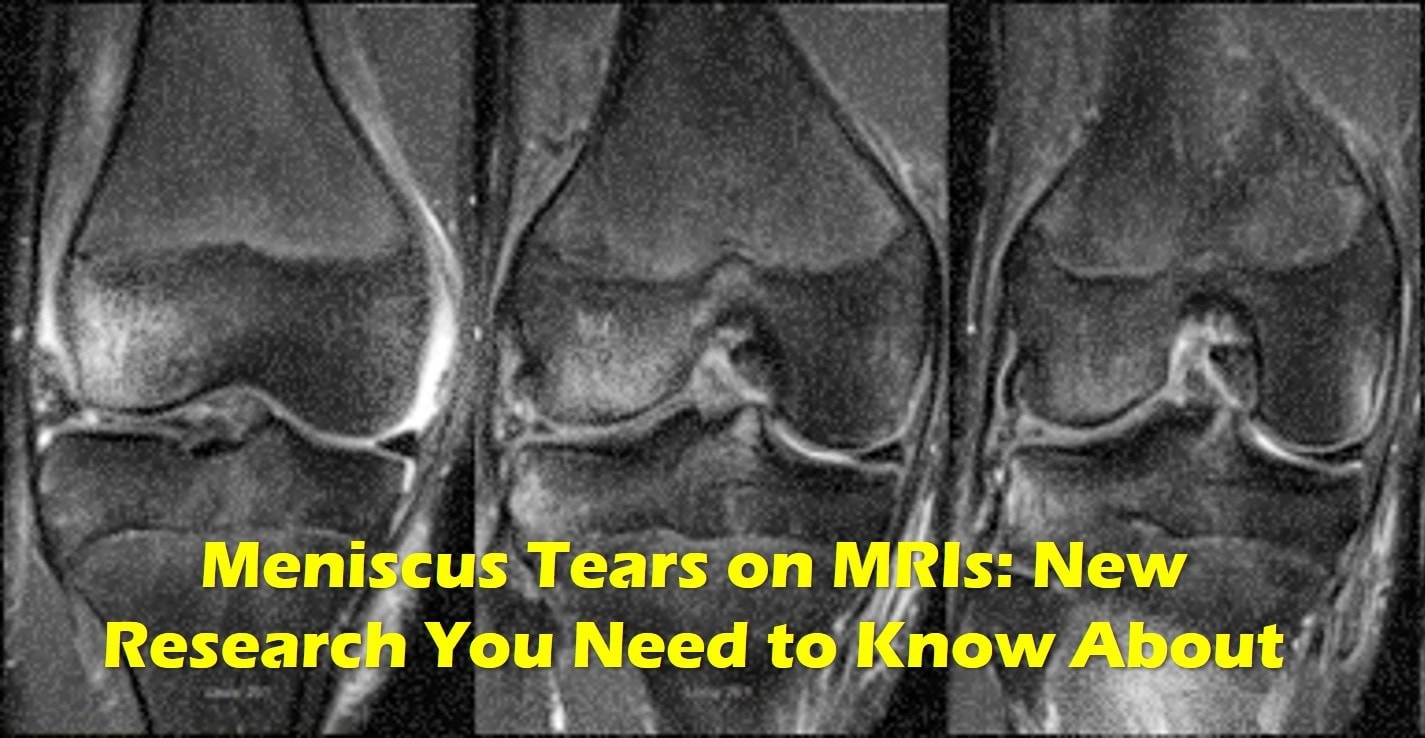
Meniscus tear MRI is a common imaging technique used when patients have knee pain. Regrettably, when a meniscus tear is seen on MRI, what happens next is often surgery. However, many research studies have been done in this area including a new one using the best MRI machine currently available and they all say the same thing. Take your meniscus tear finding on MRI with a big grain of salt and stay away from surgery. Let me explain.
What is Meniscus Tear MRI?
MRI uses magnetic fields to see tissue. It’s often used to visualize a tear in the meniscus, which is a figure-8 shaped structure that cushions the bones of the knee joint. Regrettably, this is often where the problems start. Why? Turns out meniscus tears may be one of the biggest medical scams ever devised. Surprised? Read on.
The History of MRI Findings and Knee Pain
You would think that if your doctor sees a problem like a meniscus tear on your MRI that this would be the cause of your knee pain. After all, something or nothing happened and your knee began to hurt. Hence, it makes sense that the cause of that pain could be seen on an MRI scan. However, the hard truth is more complex.
Back in 2008 researchers publishing in the New England Journal of Medicine reported that most people over age 35 without knee pain had everything from meniscus tears to cartilage loss on their MRI’s (1). These findings began the first major questioning of whether meniscus tear MRI had much value. Meaning, were meniscus tears a problem or just a function of normal aging like wrinkles?
As more research came together, Scandinavian scientists in 2014 published an editorial that physicians and patients alike should look at meniscus tears with the same diagnostic weight we give wrinkles (2). Again, that meniscus tears were about as important as wrinkles on your face, they are simply of a sign of normal aging.
Do you want to learn more about how to read your knee MRI? See my video below:
The New Meniscus Tear MRI Study
The new research used 3 Tesla MRI in 230 knees of patients without knee pain (9). These MRI scanners are the most powerful scanners with double to triple the resolution of the MRI machines in current use. Hence, these machines see more stuff that could be wrong with the knee when compared to most MRI’s.
What did they find? The MRI’s showed abnormalities in 97% of the non-painful knees. 30% had meniscus tears, cartilage and bone marrow lesions at the knee cap area (patellofemoral). About 1/3 of the knees had severe cartilage lesions. Tendon damage was detected in about 1 in 5 patients.
Remember, these were patients who had NO knee pain. Hence if so many patients have big problems on their knee MRI’s and have no pain, why are we freaking out about meniscus tears on MRI’s when patients have knee pain? Let’s dig in further.
Do All Meniscus Tears Need Surgery? Should I Get Meniscus Surgery?
So if most meniscus tears in patients who are middle-aged and older aren’t likely to be causing pain and are simply signs of normal aging, should you get surgery? No. In addition, we now have multiple large high-level studies that the most common surgery performed, Arthroscopic Partial Meniscectomy, doesn’t work (10-12). Why then is it offered to millions? Great question.
What Else Can be Done if My Knee Hurts?
Steroid Injections
These are medications that can reduce swelling, also known as cortisone. The problem is that recent research shows that the injections don’t work as well as we thought and destroy normal cartilage (13).
Viscosupplementation
This is a fancy word for an injection of a specialized lubricating gel. These products mimic the natural fluid (synovial fluid) in the knee. Brand names include Orthovisc, Synvisc, Supartz, and Euflexxa. Do these injections work? That research is all over the map at this point, meaning some studies are positive and others negative (14, 15). However, overall, these shots seem to work for about 6 months. The good news? There isn’t research that shows they hurt cartilage and most studies point in the direction of these products helping arthritis (16).
PRP
PRP is created by concentrating platelets from the patient’s blood. The platelets in PRP then release growth factors that can help reduce swelling and help damaged cartilage cells. The research on PRP as a knee arthritis treatment is very good with multiple studies showing that PRP beats viscosupplementation (17). However, these injections are not yet covered by most insurance plans, with costs ranging about $1-2,000 USD per PRP injection. Despite this, Regenexx has been able to obtain coverage from large self-insured employers.
The upshot? Meniscus tear MRI findings are not as big a deal as we once thought. Hence, please be careful about choosing procedures that don’t chop out your meniscus based on a tear that was likely there before your knee began to hurt! You meniscus tears are simply a sign of normal aging!
_________________________________
References:

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
