PRP Injections for Knee ACL Tears: A Few Sandwiches Short of a Picnic
When I was in medical school I had a British girlfriend who used to use the very English expression, “A few sandwiches short of a picnic”. That saying immediately came to mind as I reviewed a new study published by orthopedic surgeons in the middle east as they compared ACL surgery to PRP injection. It also comes to mind as I see more and more mid-levels attempt to inject torn ACLs at “stem cell” clinics. Let’s dig in.
A Few Sandwiches Short of a Picnic
So what does this British expression mean? It describes someone who is not very bright. For example, “That new guy is a few sandwiches short of a picnic”.
A New PRP ACL Study
This new study out of the middle-east is a great way to explore the concept of a few sandwiches short of an “orthobiologic” picnic. In this study, the investigators took “ACL Rupture” patients and randomized them to get surgical reconstruction or an intra-articular platelet-rich plasma (PRP) injection (1). They found that surgical reconstruction produced a slightly better drop in pain and better range of motion. However, the study gets a “few sandwiches short of a picnic” award. Why?
“ACL Ruptures”
First, the study says nothing about what type of “ACL Ruptures” they treated. This is a big miss, as, in the world of orthobiologic injections, these are the types of ACL tears:
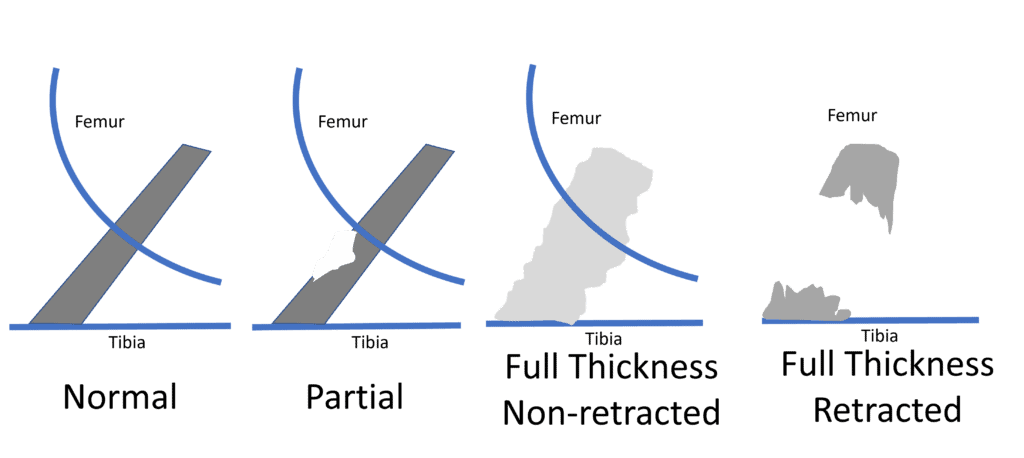
Injections of orthobiologics, based on our extensive experience can only help the middle two tear types (Partial and Full Thickness Non-Retracted). They can not help the type to the far right when the two ends of the ligament are snapped back like a rubber band. Hence, if the authors of this paper had more full thickness retracted tears being treated, it was doomed before it began.
PRP “Intra-articular”
Next, the surgeons performing the study made no attempt to get the PRP inside the damaged ligament and instead injected it inside the knee joint in general (intra-articular). Why did this qualify them for our “few sandwiches short of a picnic” award? Let’s explore that problem.
Below is a picture of what a ligament looks like at magnification once it’s removed from the body, dried, and stained:
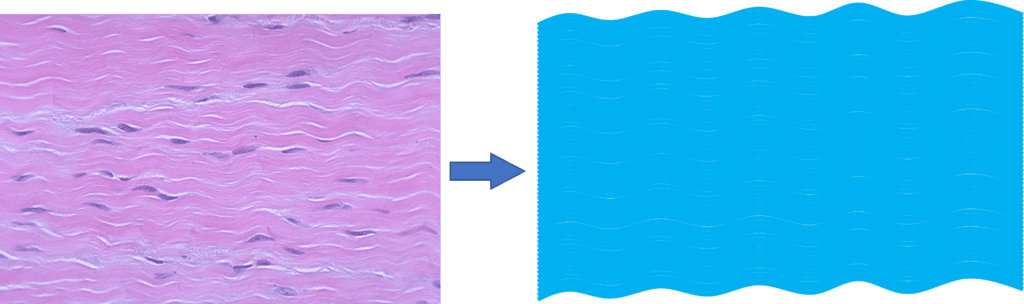
On the right, I drew a diagram to represent the dense fibers of a ligament. Below is what a partially torn or a complete non-retracted tear looks like under a microscope:
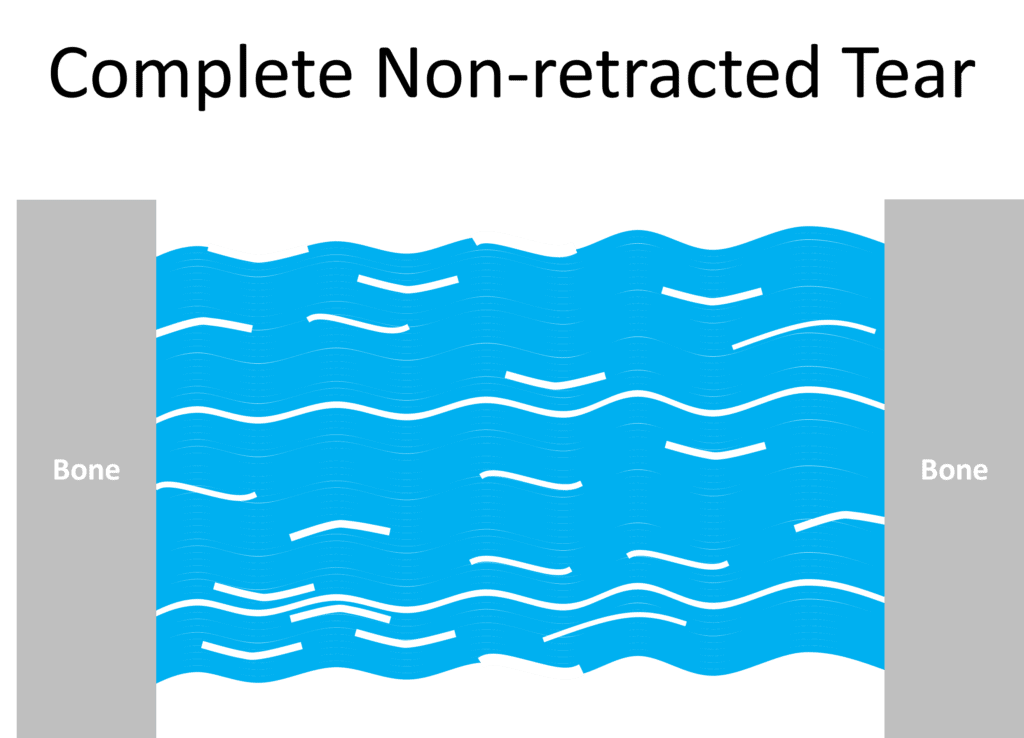
Note the white areas are tears in the individual fibers that make up the ligament. Now here’s what would happen if you injected PRP or even stem cells containing bone marrow concentrate (BMC) into the joint and not into the ligament:
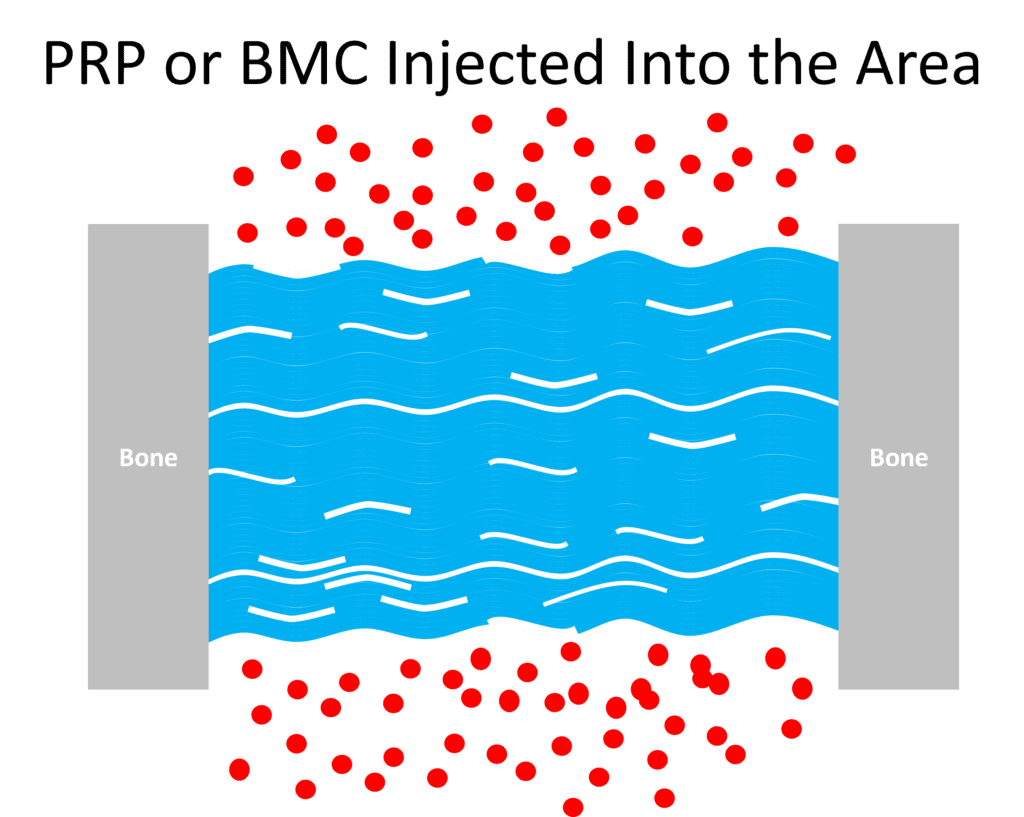
Note that the red dots are the platelets or stem cells. They can’t get into this dense fibrous ligament tissue to reach the tears, so they do little good. Now here’s what it looks like if the doctor uses precise imaging guidance to get inside the ligament:
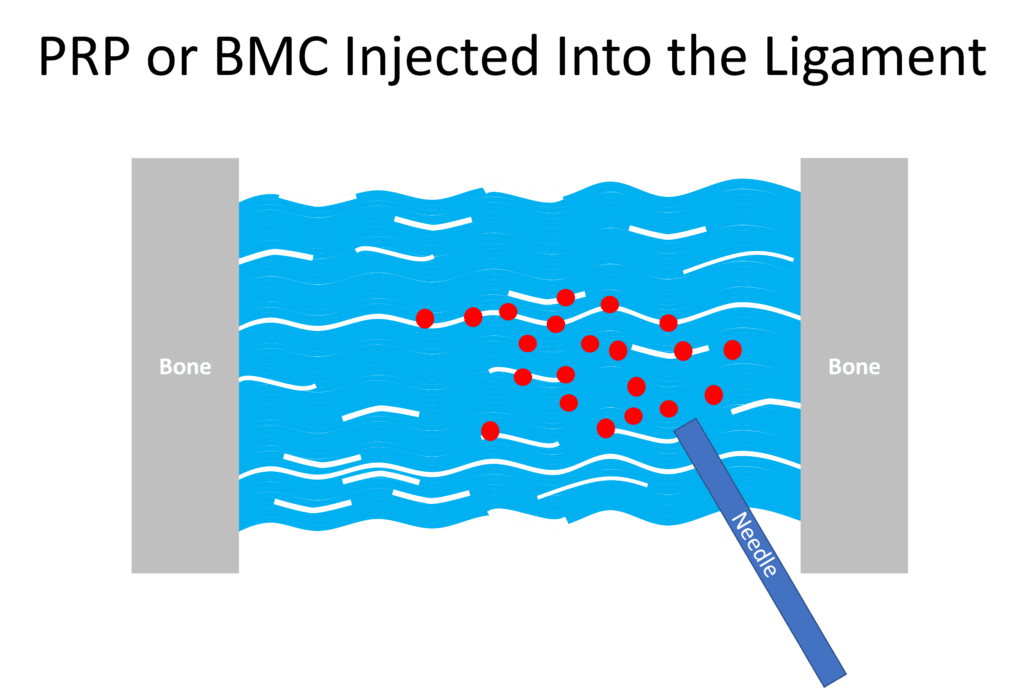
Now the platelets and the stem cells can reach the damaged ligament fibers. In summary, injecting into the knee joint doesn’t make sense to treat a damaged ligament like the ACL.
How this Study Should Have Been Done to Determine if PRP Could Help ACL Tears
A real injection into the ACL looks like this:
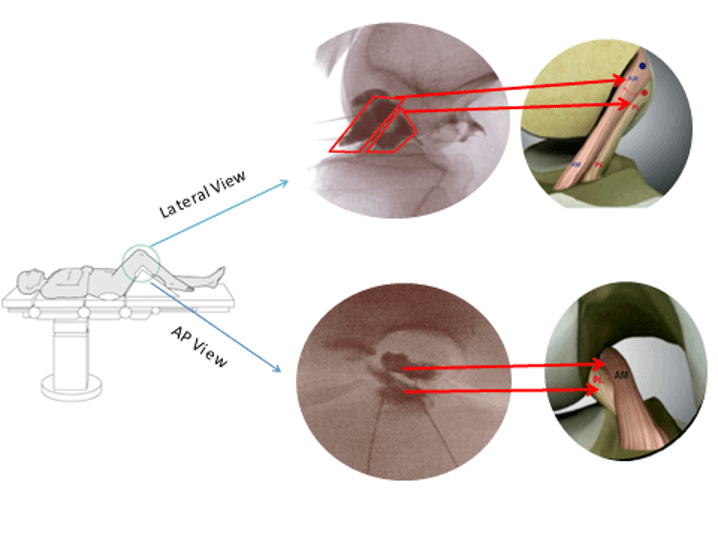
Here the doctor uses a c-arm fluoroscope and contrast to inject inside the ligament, which is a very precise injection that must get the PRP or BMC into the ligament bands. Here’s a video of the injection:
Hence, injecting into the actual ligament would have taken an immense amount of retraining for these orthopedic surgeons. We have published three research studies on the efficacy of this precise injection technique called Perc-ACLR (2-4).
The Mid-Level and Alt Med Clinic Fake and Bake
It’s not just orthopedic surgeons in the middle east who don’t know which end is up when trying to use orthobiologic injections to treat ACL tears, we also see this happening here in clinics run by mid-levels like QC Kinetix and alternative medicine clinics claiming to inject ACL tears (like chiro clinics). IMHO, neither possesses the skill levels to perform the proper precise ACL injection, so whatever is injected is just parked in the knee joint and not in the damaged ACL where it needs to be.
The upshot? I hope you can see why this most recent ACL PRP study is a few sandwiches short of a picnic. In addition, realize that at this point, few clinics offering to treat a torn ACL can actually get the PRP or BMC inside the damaged ligament, so few can actually produce ligament healing results.
___________________________________________________
References:
(1) Eslami S, Fattah S, Taher SA, Rezasoltani Z. Platelet-rich plasma therapy or arthroscopic surgery on repair of anterior cruciate ligament rupture. Eur J Transl Myol. 2022 Aug 1. doi: 10.4081/ejtm.2022.10538. Epub ahead of print. PMID: 35916761.
(2) Centeno CJ, Pitts J, Al-Sayegh H, Freeman MD. Anterior cruciate ligament tears treated with percutaneous injection of autologous bone marrow nucleated cells: a case series. J Pain Res. 2015;8:437–447. https://www.ncbi.nlm.nih.gov/pubmed/26261424(3)
(3) Centeno C, Markle J, Dodson E, et al. Symptomatic anterior cruciate ligament tears treated with percutaneous injection of autologous bone marrow concentrate and platelet products: a non-controlled registry study. J Transl Med. 2018;16(1):246. https://www.ncbi.nlm.nih.gov/pubmed/30176875
(4) Centeno C, Lucas M, Stemoer I, Dodson E.
-Guided Injection of Anterior Cruciate Ligament Tears with Autologous Bone Marrow Concentrate and Platelets: Midterm Analysis from a Randomized Controlled Trial. Bio Ortho J Vol 3(1):e29–e39; October 5, 2021.

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
