The Side Effects of Hip Labrum Surgery: Brian’s Story
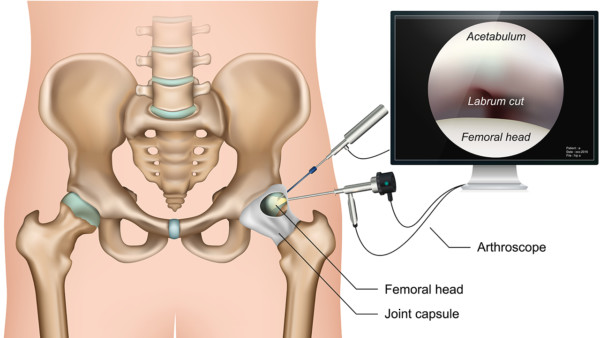
Hip Arthroscopy
Medicalstocks/Shutterstock
- Hip labrum surgery complications can make the hip unstable.
- Hip labrum surgery shouldn’t be performed based only on MRI findings and a quick exam.
- Hip labrum tears can be normal wear and tear and may not be the cause of hip pain or an indicator for surgery.
- Hip surgery won’t work if the problem isn’t really in your hip, and many times the problem is actually in the low back.
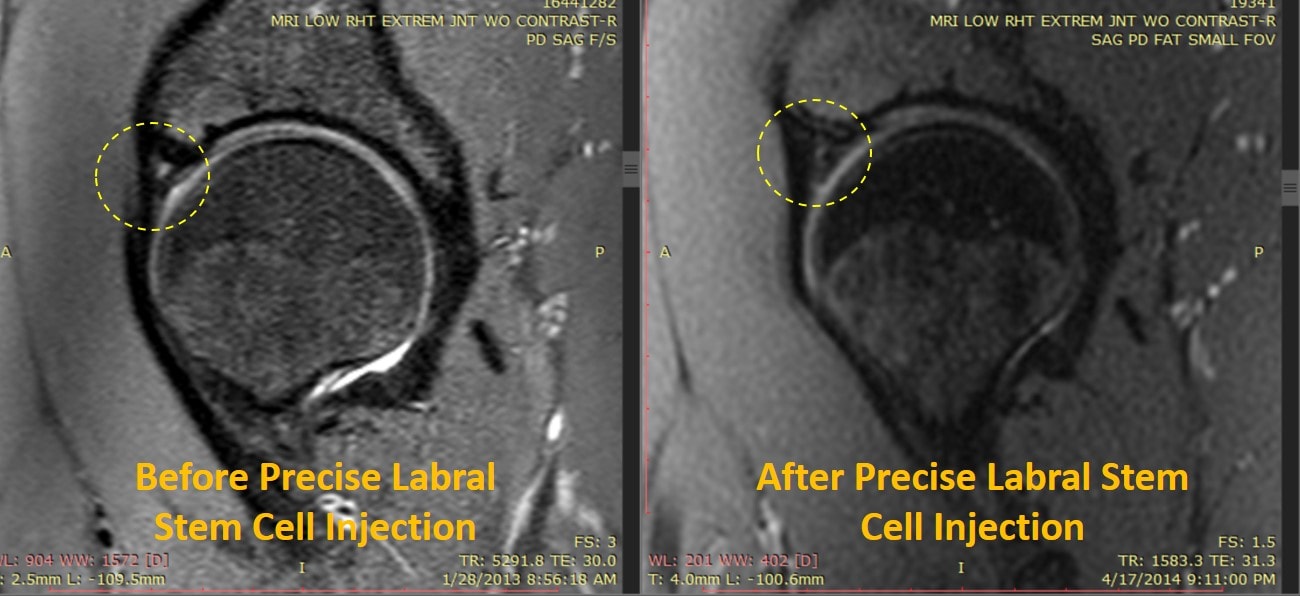
- Platelet or stem cell injections may be able to replace the surgery.
Brian’s Important Story
“I first noticed hip discomfort in 2008, and at the time did not appear concerning so I was recommended for physical therapy. By 2011 I had visited 3 different medical physicians, and my hip discomfort had not improved, but rather worsened and as a result an MRI arthrogram was ordered for my hip. The radiology came back showing that I had an acetabular labrum tear. When the diagnosis was shared with me I was informed that it is not uncommon for people to have labrum tears, and that many people don’t even know they have one as they’re asymptomatic. Nonetheless I was informed to follow-up with an orthopedic surgeon who specializes in arthroscopic hip repairs (fun fact he was actually one of the guys who helped to innovate the procedure). When I spoke with him he informed me that my presentation was classic for a labrum tear. I was intending to begin medical shcool in 2012, and as I was not improving with physical therapy, the physician felt confident I would have relief from the acetabular labrum repair with femoroplasty and acetabuloplasty and be ready for school. Following the arthoscopic hip surgery in March 2012 the news that I received was that my hip socket during the surgery ended up appearing very different in person as compared to the CT and MRI’s that were performed prior. The physician had called my mother on the phone and mentioned that the cartillage damage was more extensive than he thought, and that he did the best he could do to suture and mend the cartilage.
After three months of rehabilitation I did not notice my symptoms improving, and actually felt a lot worse than I did prior. When I followed up with my surgeon, I shared my experience with him and he felt confident that additional shaving of the head of my femur and acetabulum would allow my hip socket to have better articulation and relief of my symptoms. The decision of having an additional hip arthoroscopy proved to be a major mistake as the corrections that were made to my hip socket were such that I lost the ability to walk. I thought that in a couple weeks following the surgery I would be able to start bearing weight again, but after a couple months I was dismayed to discover that I was unable to bear any weight at all on my leg without falling, and that any position beyond horizontal brought me extreme pain. My sleep, which was difficult prior to the hip arthroscopies, became unaccomplishable without the use of narcotics and after 3 months of vicodin I was waned off and placed on up to 4800 mg Neurontin.
While this was going on my family and I continued to schedule referrals to physicians who, though many were well intended, were not very helpful. The feedback we received ranged from: drug seeking behavior, anxiety about starting medical school, psychosomatic, and even when my symptoms were taken seriously the only solution that was on the table was a hip replacement. This absolutely terrified me, and my unwillingness to undergo a hip replacement was usually followed by advise that I needed to find a way to get on with my life then. Words can’t do justice to how emotionally, psychologically, and physically debilitating this experience was for me. Not being taken seriously or having my symptoms explained as drug-seeking behavior, though did lead me to a great cognitive-behavioral therapist, was an awful experience to go through.
My family and I spent 10 months, during which I was not able to walk without the use of crutches, in and out of doctor’s offices as well as posting my medical information online in search of help. This brought us to Regenexx, and after one discussion on the phone I experienced more empathy than any of the other 15 physicians I saw in person. Since then my walking has been restored, my sleep has been getting better, I no longer take neurontin or vicodin, I have begun medical school, and I have grown from feeling completely depressed and hopeless to optimistic that a functional life is in store for me.
While the orthopedic surgeon who performed my arthroscopic surgeries made mistakes, I do not blame him for it. I honestly believe, whether this is true or not, that he was doing the very best he could within his knowledge and ability. From my experience in healthcare I have discovered that there are not a lot of options in the minds of many physicians, whether surgeon or not, besides physical therapy, medication, and surgery. Is it because of the regulated atmosphere of healthcare? Is it because of the preferential treatment that pharmaceutical companies receive from the FDA? Is it due to the medical training that prepares medical students for Step/Board exams rather than patient care? Has the process of specialization in healthcare caused confirmation bias in certain fields? While these questions are the correct ones to ask, the answers I do not have. As I continue with my medical training I will continue to be wrestling with these questions, but as a result of my experience I have found myself to have a deep appreciation for physicians who take their patients seriously and have the desire to solve complex problems.”
Yesterday I injected his torn L5-S1 low back disc. This was likely causing the symptoms on the bottom of his foot (through irritation of the S1 nerve). However, it was injecting his SI joint that caused his usual groin pain, the same pain that he initially sought care for many years ago! So it’s likely that even though he had a labral tear, it wasn’t causing his pain. His SI joint was the real cause. Hence the reason why labral surgery never got rid of the pain.
The upshot? It’s been a pleasure getting Brain back on track in his medical education. We found a kid struggling to walk, with his medical-school education on indefinite hold due to the side effects of hip labrum surgery, and now he’s finally finished his first year of medical school! Hopefully Brian will use this experience to motivate himself to be the kind of physician who thinks outside the box!

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.