Stem Cells and Disc Repair
A Japanese researcher named Sakai, captured my interest in Mesenchymal Stem Cells (MSC’s). He published a work in 2003 that I picked up on in the summer of 2005. I was hooked. In this study he created a degenerated disc by using a “stab model”, meaning he stuck a really big needle into the disc and sucked out the inside (nucleus pulposis). The disc rapidly “went bad” by losing it’s ability to hold onto water (went dark on MRI) and began losing disc height (collapsing). He then placed MSC’s into the disc and after 6-12 weeks the disc regained it’s normal bright signal on MRI and started “plumping up” or gaining increased height. As an interventional pain physician struggling everyday to manage patients with severe low back pain and leg pain from sciatica, this was an amazing discovery. We could possibly stop managing pain and start fixing the problem.
As you may have read elsewhere, lumbar disc repair is the holy grail of musculoskeletal stem cell work. Why? Because it’s very tough to do. While Sakai was able to regenerate rabbit discs and others have regenerated the discs of dogs, pigs, and rats, it’s likely allot harder in humans. The reason is that biped humans (we that walk on two legs) are really tough on our low back discs. They start to lose their blood supply and nutrition when we’re teenagers, and for some of us it’s downhill from there. Not so in the average animal disc, where the forces are much kinder. So while stem cells injected into an animal disc might be entering a warm and cozy environment, cells entering a human disc are being forced to live in a very hostile environment. Think of a person being left to fend for himself in the desert without food and water for weeks. The cells don’t like this type of environment.
Our IRB approved disc research effort began in late 2005 with simple BMAC transplants. Ineffective. We then went to implanting culture expanded MSC’s into the disc, essentially replicating much of the animal research. Ineffective. We then spent about a year in further basic research, moving two steps back before we could take one forward. We finally figured out why the cells were unable to take hold, fixed that issue and started to see good reliable resolution of low back disc bulges causing sciatica. With a simple x-ray guided injection series and without surgery we were able to take the patent’s leg pain away and repair the injury to the back of the disc. This then lead to a case series (research paper) which has been recently submitted for scientific publication. However, in animals it was relatively easy to get rid of the disc bulge and rehydrate the disc (get a dark disk to go bright again). That’s a big deal as that means the disc can operate as a good schock absorber. So we went back to the drawing board another time trying to achieve this as well. We’re happy to announce that we now have solid evidence that we can rehydrate discs. The MRI’s below are a case in point:
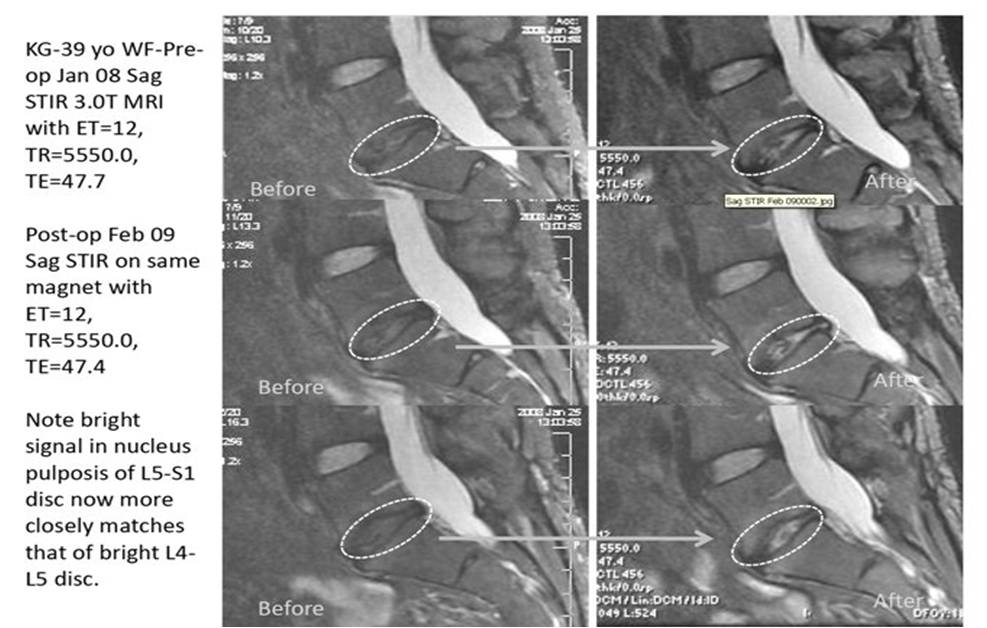
This is a patient who had a failed low back surgery (L5-S1 discectomy) and who had no long-term response to epidural injections. For the last several years, she had increasing low back and leg pain/tingling. Her disc bulge and lack of hydration at L5-S1 was worsening over time on serial MRI’s. As an aside, discs on MRI go one direction once they start losing water and collapsing, they get darker on MRI (an indication that they are getting dried out), lose their height, and get bigger bulges.
The screen shot above shows the L5-S1 dark disc in the dashed circle. The left pictures are that disc before the Regenexx-C disc procedure and the right images are 13 months after treatment. Note that the disc has gone from dark (dehydrated and a bad shock absorber) to bright (holding onto more fluid-better shock absorber). Note that none of the other serial images in this patient showed the change in this disc. Radiologists often like to see things in at least two planes (the above is sagittal), so here is the axial of the same disc (“saw you in half” view):
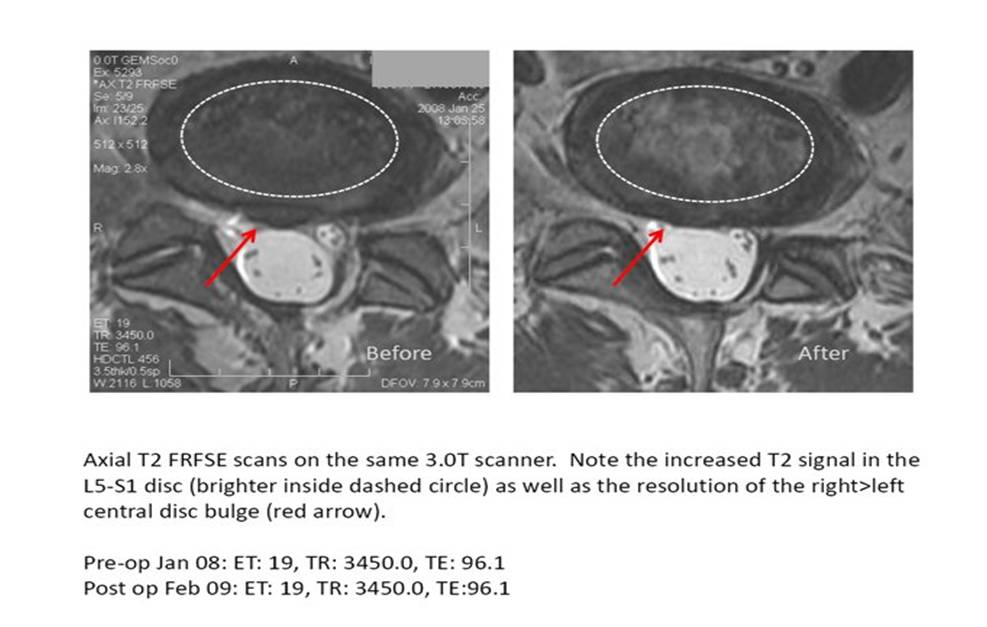
Notice the disc bulge in the before image on the left (red arrow) now not there on the right image (13 months post Regenexx-C disc procedure). Also notice the brighter water signal in the dashed circle on the right (more white stuff seen in the disc). The patient reported improved back pain and no more leg numbness and tingling. She went back to much of her old pre-injury activities.
So what does all of this mean? Our recent improvements to the procedure have allowed us to finally begin to rehydrate the disc. We’re very excited about this new finding and believe it will offer many patients the opportunity to avoid low back surgery. On the flip side, we can’t be certain that every low back patient we treat will get these same results.

If you have questions or comments about this blog post, please email us at [email protected]
NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
