What is the Future of Orthopedics?
The pace of innovation has been accelerating at a break neck pace this past two decades. Just contemplate for a second that the Internet was born in the late 90s and in 15 short years has come to dominate our lives. The future of orthopedics is also about to shift into high gear. Why? Because we have our first technologies in wide spread use that can now repair tissue and these technologies will continue to improve over the next two decades, turning the world of surgical orthopedics on it’s head.
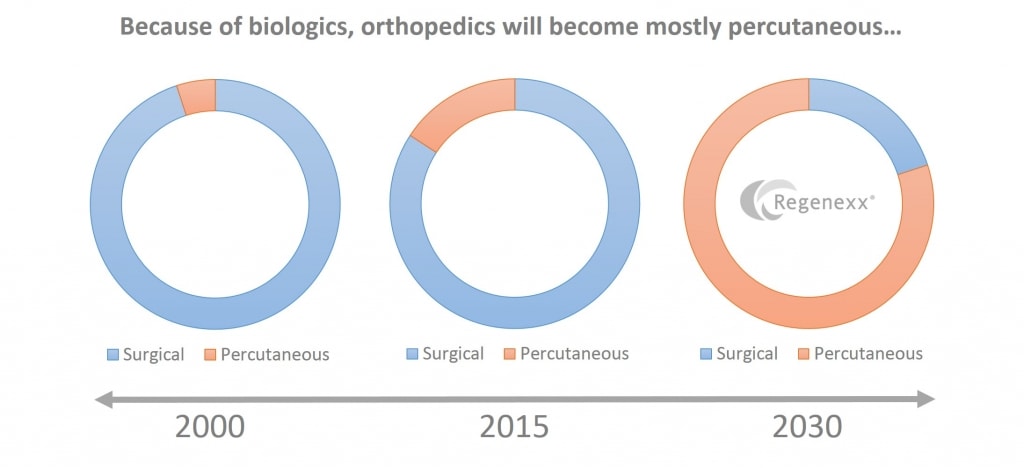
The video above shows that by the turn of this century, the future of orthopedics hadn’t changed all that much since the late 1980s. Meaning, what was done in 1990 wasn’t all that much different than what was done in 2000. While there were some improvements in devices that were used in arthroscopic surgery, no earth shattering changes occurred. The same really held true by 2005. In addition, while arthroscopy had been a major advance in the 1980s in that it allowed less invasive surgery to be performed and widened the number of problems that could be treated, the basic concepts behind operating didn’t change with arthroscopy. Those concepts also really haven’t changed by 2014. They are-sew back together torn tendon-ligament tissue, bolt together damaged structural tissue like bone, and cut out tissue that won’t heal. The next 15 years will be quite different (click on the video below or the picture above for a short video discussion).
The big picture concept that hasn’t changed since the time of the Greeks and Romans is that tissue heals when it heals and how it wants to heal and this determines residual pain and function. That conceptual understanding is now changing. From the 1950s forward, we’ve only had one thing that could be injected to help pain and improve function-high dose steroids. Regrettably newer research has shown that high dose steroids are awful for your orthopedic tissues and stem cells. Based on what I’ve observed since 2005, injectable agents like platelet rich plasma and stem cells can help tissue heal or reduce it’s degradation, help pain, and increase function.
The thing about the current round of first generation autologous (meaning your own) biologics is that they alter this playing field. The basic reason to operate is in many ways eliminated. For example, if a precise injection of PRP can help heal tendonitis, what’s the rationale for operating at all? This is why we’re so focused on developing second and third generation autologous biologics and providing our physicians with the advanced training to precisely place these agents where they need to be. There will also be even more dramatic biologics coming down the pike, each one taking a little bite out of the case for needing to operate. In addition, as the tools improve that allow physicians to place these agents through needles to heal an ever expanding array of tissues, at some juncture it will seem a bit barbaric that we once used to operate on these orthopedic problems. In fact, we’ll view this the same way we now view an open heart surgery scar in a world where 95% of all of the cardiac work is performed through a catheter without surgery.
The upshot? The future of orthopedics isn’t surgical, it’s in needle based procedures of ever increasing sophistication. That’s why we spend so much time and energy at Regenexx refining Interventional Orthopedics!

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.