What Is Capsular Distension?
One of the procedures we perform is capsular distension. What is this and why is it done? Let’s dig in.
Understanding How Joints Move and Can Lose Motion
Aksanaku/Shutterstock
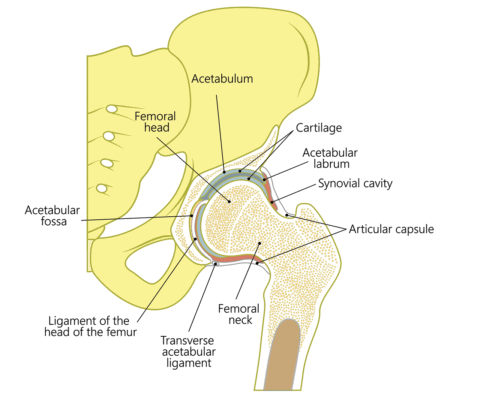
Joints like the hip and shoulder are ball in socket joints surrounded by a covering called a joint capsule. In order to get needed motion, the joint capsule has to have built-in accordion-like structures that stretch open with certain movements and close with others. In some cases, in particular, when there is inflammation, the accordion-like structures can become scarred down. This causes the joint to lose motion.
This condition, of loss of range of motion of a joint, is usually called adhesive capsulitis. This diagnosis is commonly used in the shoulder, however, it’s really the same thing in the hip. This condition is more common in patients with diabetes or who are prediabetic.
One problem this condition causes is that the joint can no longer distribute force in many different areas on the joint surface. For example, in the hip, if there is little range of motion, the weight-bearing forces of the body are placed in one spot more than others. This can cause excessive wear and tear at that spot.
Traditional Treatment for Treating Adhesive Capsulitis
How do you treat this scarred down joint capsule causing lost range of motion? Physical therapy can be tried and sometimes works well, but when it doesn’t, the next step is usually “MUA”. This stands for “Manipulation Under Anesthesia” and is when a surgeon places a patient asleep and then physically cranks on the joint to break up the scar tissue. The problem is that often the lost range of motion will return as this process can cause more inflammation which causes the accordion-like folds to scar down again.
New Ways to Treat Adhesive Capsulitis
We use a different technique to treat adhesive capsulitis called capsular distention. What’s that? The doctor places a needle into the joint and first injects a cartilage friendly anesthetic. That is then followed by an injection of platelet lysate, a product that’s made from the patient’s blood platelets that contains healing growth factors and anti-inflammatory cytokines. A super low dose steroid is also injected, which causes reduced inflammation without hurting the cartilage. The doctor injects enough of this mix to fill the joint up and expand it to stretch out and open up the accordion-like structures. The doctor then gently moves the joint around to get as close to a normal range of motion as possible.
Hence the goal here is to get your normal range of motion back by stretching out and breaking up the scarred down joint capsule. Our goal is to also leave behind an anti-inflammatory as well as growth factors to reduce the swelling and enhance the healing.
How and When Do We Use this Procedure?
We often use this procedure when there is a loss of range of motion in the shoulder or hip. Oftentimes, this would be used to get that movement back before other procedures, like a stem cell procedure. For example, for a patient who has hip arthritis and lost range of motion in a hip, we’ll try to get that range of motion back through capsular distention a few days before the stem cell procedure. The goal is to reduce the weight on any one area of the hip joint as the patient heals.
The upshot? This capsular distention procedure can work well to get range of motion back to hips and shoulders. In addition, our goal is to get this range of motion back not by destroying tissue like a traditional MUA, but through helping it heal.

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
